J Korean Ophthalmol Soc.
2012 Jul;53(7):934-940. 10.3341/jkos.2012.53.7.934.
Cultured Organisms and Antibiotic Susceptibility in Infectious Ocular Disease: Results Over a Ten-Year Period
- Affiliations
-
- 1Department of Ophthalmology, Chonbuk National University Hospital and Medical School, Research Institute of Clinical Medicine, Jeonju, Korea. you2ic@paran.com
- KMID: 2215850
- DOI: http://doi.org/10.3341/jkos.2012.53.7.934
Abstract
- PURPOSE
To investigate the ocular regional incidence, causative species and antibiotic susceptibility in patients with infectious ocular disease whose causative organism was isolated.
METHODS
A total of 519 eyes in 519 patients with infectious ocular disease, who were diagnosed by smears and cultures from January 2000 to December 2009 were retrospectively reviewed.
RESULTS
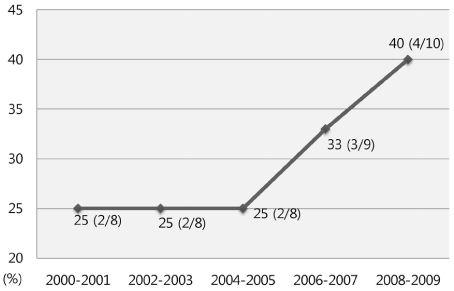
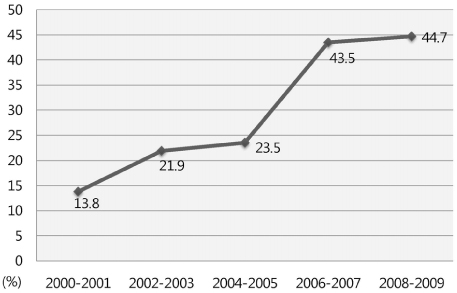
The mean age of the 519 patients was 54.0 years, and 66.1% of the patients were male. The most common systemic disease was diabetes mellitus. The most common previous ocular disease was keratoconjunctivitis. Specimens were most frequently swabbed from the cornea, where 81.2% were bacteria isolates and 18.8% fungi isolates. The most prevalent causative organism was Staphylococcus epidermidis, and the most prevalent fungus was Fusarium species. Vancomycin, ceftazidime, and fourth-generation fluoroquinolone maintained high antibiotic susceptibility. Methicillin-resistant Staphylococcus aureus and methicillin-resistant Staphylococcus epidermidis were increasing near the end of the reference period, and endophthalmitis was more common in methicillin-resistant Staphylococcus.
CONCLUSIONS
Identifying the causative organism in infectious ocular disease by smears and cultures is essential. More effective treatment of infectious ocular disease would be possible by analyzing the frequent organism, clinical manifestations, and antibiotic susceptibility. More caution is necessary due to the increase in methicillin-resistant Staphylococcus.
Keyword
MeSH Terms
Figure
Reference
-
1. Khosravi AD, Mehdinejad M, Heidari M. Bacteriological findings in patients with ocular infection and antibiotic susceptibility pattern of isolated pathogens. Singapore Med J. 2007. 48:741–743.2. McClellan KA. Mucosal defense of the outer eye. Surv Ophthalmol. 1997. 42:233–246.3. Jones DB. Decision-making in the management of microbial keratitis. Ophthalmology. 1981. 88:814–820.4. Blanton CL, Rapuano CJ, Cohen EJ, Laibson PR. Initial treatment of microbial keratitis. CLAO J. 1996. 22:136–140.5. Limberg MB. A review of bacterial keratitis and bacterial conjunctivitis. Am J Ophthalmol. 1991. 112:4 Suppl. 2S–9S.6. Liesegang TJ. Bacterial keratitis. Infect Dis Clin North Am. 1992. 6:815–829.7. Afshari NA, Ma JJ, Duncan SM, et al. Trends in resistance to ciprofloxacin, cefazolin, and gentamicin in the treatment of bacterial keratitis. J Ocul Pharmacol Ther. 2008. 24:217–223.8. Snyder ME, Katz HR. Ciprofloxacin resistant bacterial keratitis. Am J Ophthalmol. 1992. 114:336–338.9. Williamson-Noble FA, Sorsby A. Conrad B, editor. Etiology of the eye diseases; developmental defects; heriedity. The Eye and Its Diseases. 1950. 2nd ed. Philadelphia: WB Saundars Company;309–321.10. Hahn YH, Lee SJ, Hahn TW, et al. Antibiotic susceptibilities of ocular isolates from patients with bacterial keratitis: a multi-center study. J Korean Ophthalmol Soc. 1999. 40:2401–2410.11. Jensen HG, Felix C. In vitro antibiotic susceptibilities of ocular isolates in North and South America. In Vitro Antibiotic Testing Group. Cornea. 1998. 17:79–87.12. Ooishi M, Miyao M. Antibiotic sensitivity of recent clinical isolates from patients with ocular infections. Ophthalmologica. 1997. 211:Suppl 1. 15–24.13. Ramesh S, Ramakrishnan R, Bharathi MJ, et al. Prevalence of bacterial pathogens causing ocular infections in South India. Indian J Pathol Microbiol. 2010. 53:281–286.14. Kim HT, Lee JY, Chung SK. The cultured organisms and in vitro antibiotic sensitivity of ocular bacterial infection. J Korean Ophthalmol Soc. 1999. 40:941–949.15. Kalkanci A, Ozdek S. Ocular fungal infections. Curr Eye Res. 2011. 36:179–189.16. Thomas PA. Fungal infections of the cornea. Eye. 2003. 17:852–862.17. Freidlin J, Acharya N, Lietman TM, et al. Spectrum of eye disease caused by methicillin-resistant Staphylococcus aureus. Am J Ophthalmol. 2007. 144:313–315.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Cultured Organisms and In Vitro Antibiotic Sensitivity of Ocular Bacterial Infection
- Clinical Features of Infectious Keratitis in West Coast Area of Chungcheongnam-do, Korea
- The Resistance to Ciprofloxacin in Bacterial Ocular Disease
- Analysis of Inpatients with Bacterial Keratitis Over a 12-Year Period: Pathogenic Organisms and Antibiotic Resistance
- Ten-year Trends in Infectious Keratitis in South Korea