J Korean Ophthalmol Soc.
2011 Oct;52(10):1254-1258. 10.3341/jkos.2011.52.10.1254.
Cilioretinal Artery Occlusion as the First Clinical Manifestation of Ocular Syphilis
- Affiliations
-
- 1Department of Ophthalmology, Chungnam National University College of Medicine, Daejeon, Korea. kimjy@cnu.ac.kr
- KMID: 2215012
- DOI: http://doi.org/10.3341/jkos.2011.52.10.1254
Abstract
- PURPOSE
To report a case of a neurosyphilis patient with cilioretinal artery occlusion as the first manifestation.
CASE SUMMARY
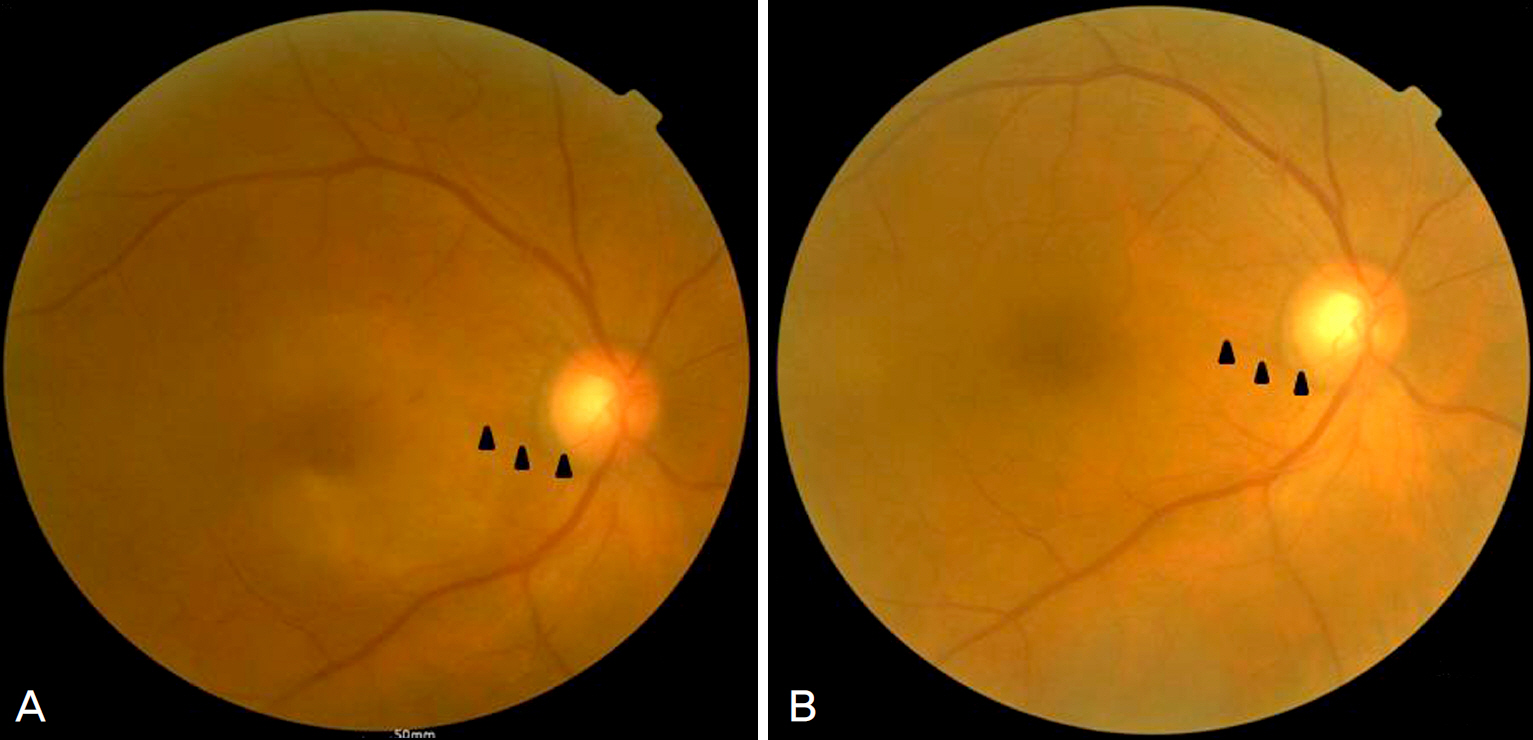
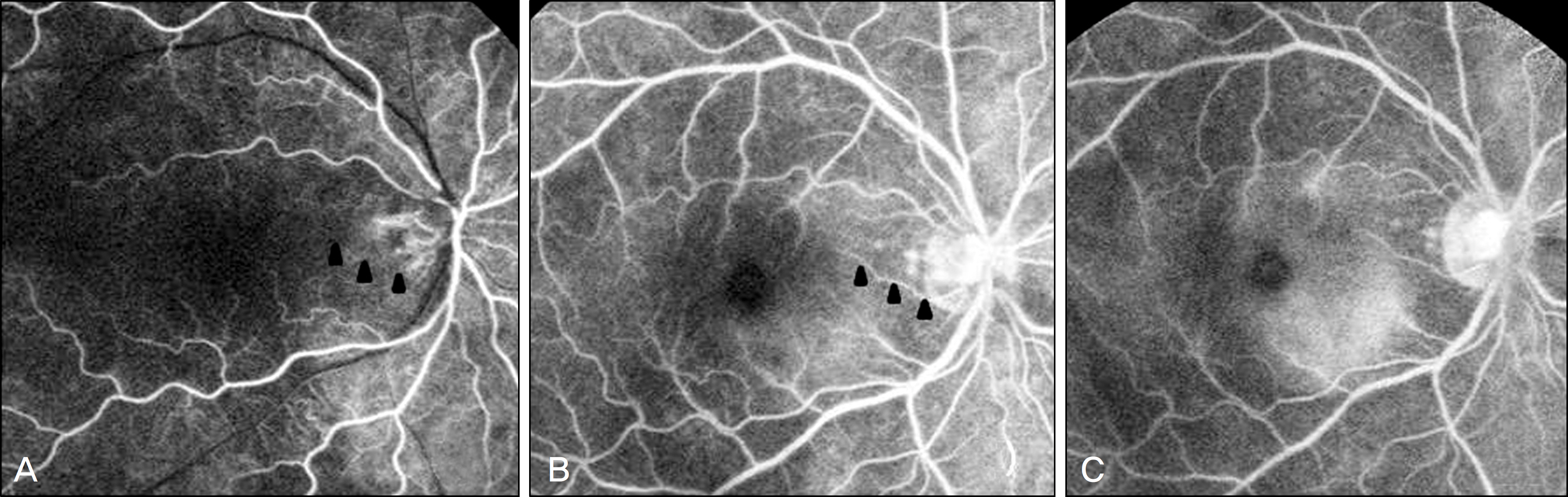
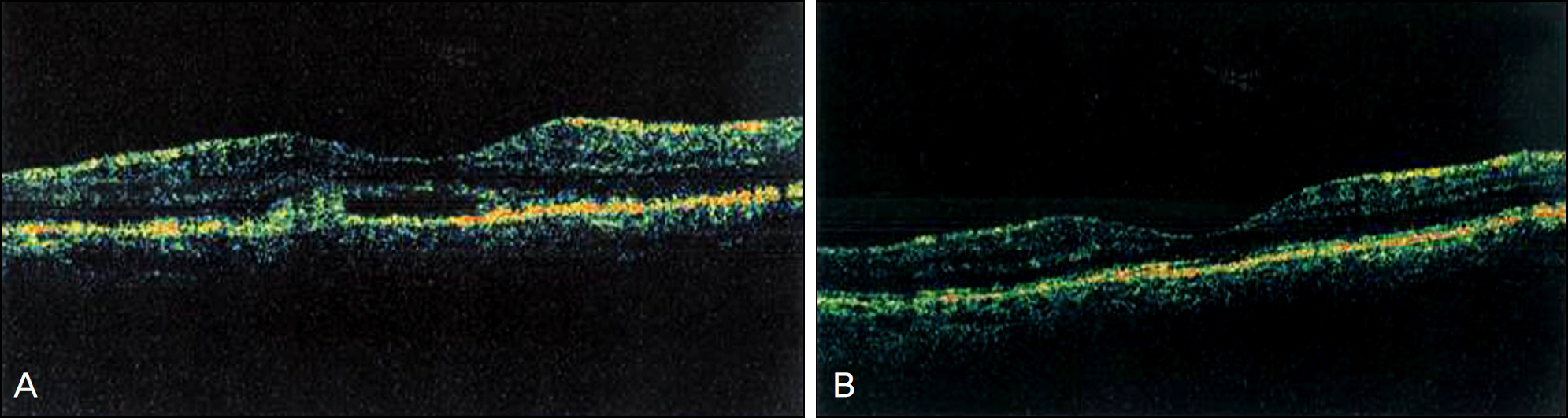
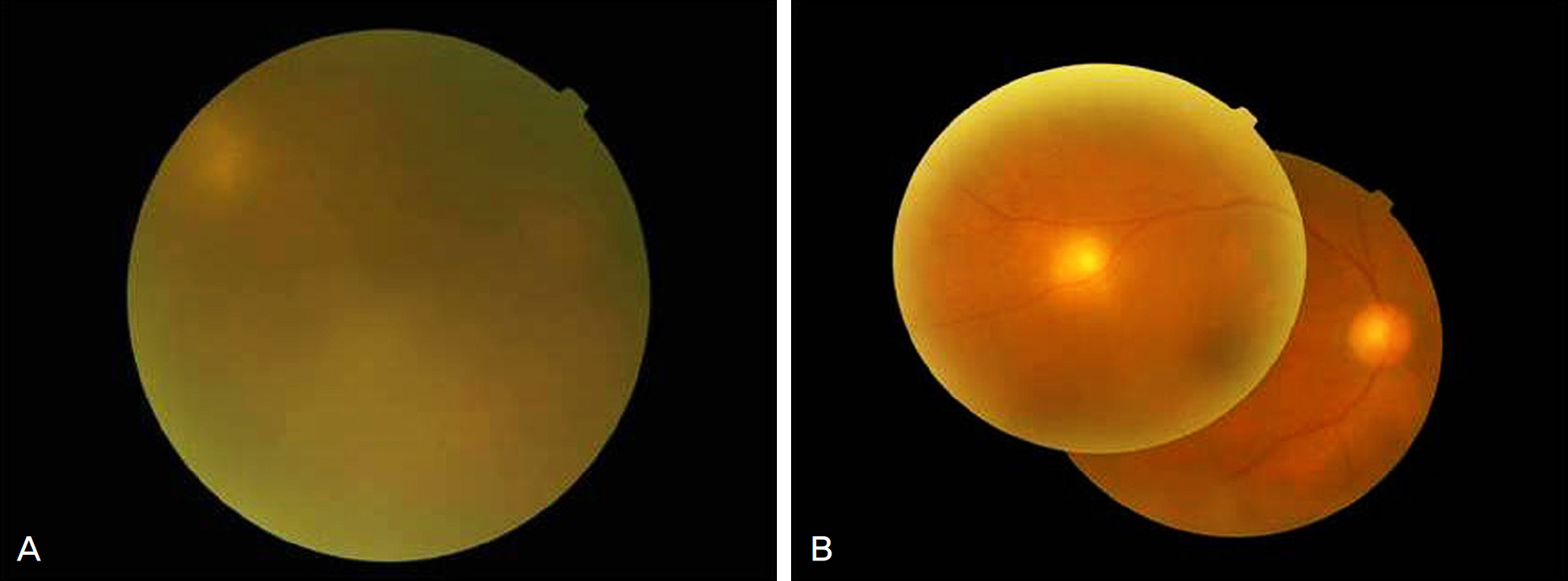
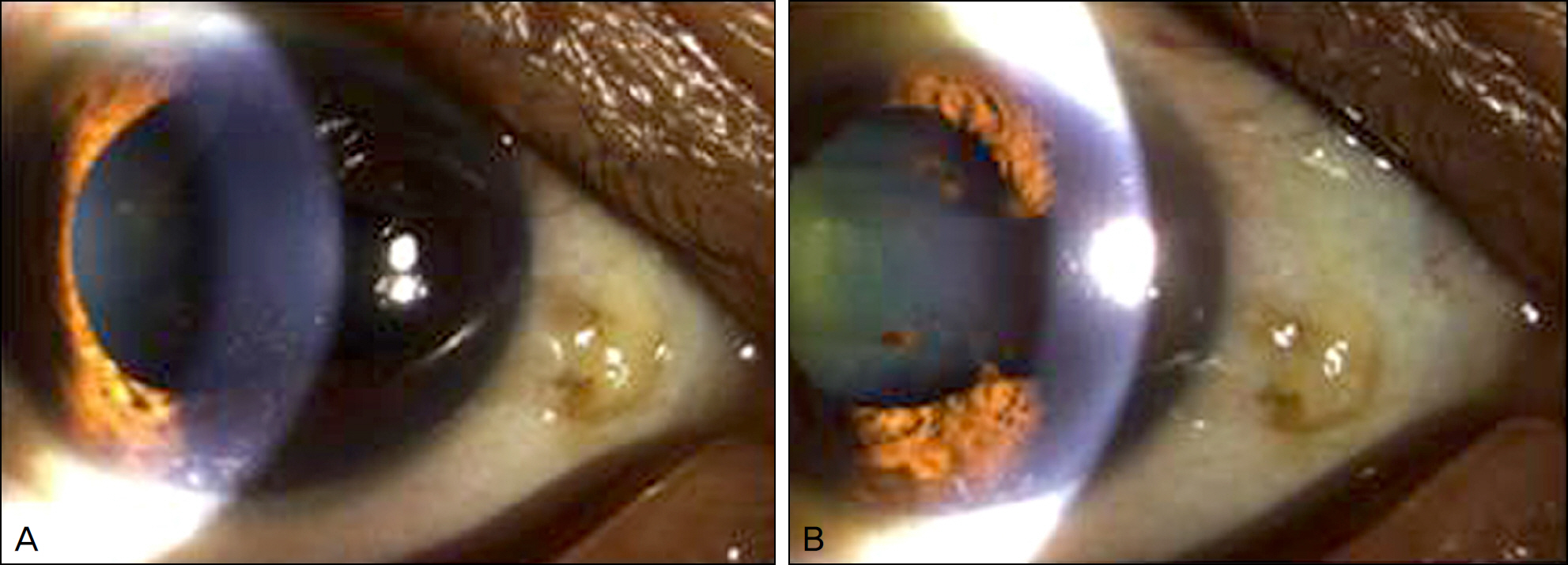
A 58-year old man presented with a visual impairment which developed 5 days earlier in his right eye. During initial evaluation, the visual acuity in the right eye was 0.02. On fundus examination, a whitening adjacent to the macula was observed and fluorescein angiography showed filling delay and late leakage of the cilioretinal arteries. The patient was diagnosed with cilioretinal artery occlusion. Two weeks after his initial visit, visual acuity in the patient's right eye improved to 0.7 and retinal whitening was decreased on fundus examination. Three months later, a visual decrease in the right eye reoccurred and the visual acuity was 0.01. Anterior chamber cell reaction with hypopyon was observed on slit lamp examination and vitreal opacity was noted during fundus examination. Among the numerous tests performed in order to determine the cause of uveitis, RPR antibody and treponemal antibody were found positive. The patient was diagnosed with neurosyphylis and 2 weeks after intravenous administration of penicillin, visual acuity improved to 0.7 and anterior chamber cell reaction as well as vitreal opacity decreased.
CONCLUSIONS
The authors reported a case of cilioretinal artery occlusion suspected secondary to neurosyphilis.
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Manifestations of Ocular Syphilis Combined with Neurosyphilis
Yong Wun Cho, Che Ron Kim, Yong Seop Han, In Young Chung, Jong Moon Park
J Korean Ophthalmol Soc. 2014;55(4):602-607. doi: 10.3341/jkos.2014.55.4.602.
Reference
-
References
1. Song YM, Choi O. A study of the cilioretinal artery in Korean. J Korean Ophthalmol Soc. 1981; 22:363–6.2. Wood AC. Syphilis of the eye. Am J Syph Gonor Vener Dis. 1943; 27:133–86.3. Deschenes J, Seamone CD, Baines MG. Acquired ocular syphilis: diagnosis and treatment. Ann Ophthalmol. 1992; 24:134–8.4. Schlaegel TF Jr, Kao SF. A review (1970–1980) of 28 presumptive cases of syphilitic uveitis. Am J Ophthalmol. 1982; 93:412–4.
Article5. Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001; 12:433–41.
Article6. Barile GR, Flynn TE. Syphilis exposure in patients with uveitis. Ophthalmology. 1997; 104:1605–9.
Article7. Hong MC, Sheu SJ, Wu TT, Chuang CT. Ocular uveitis as the initial presentation of syphilis. J Chin Med Assoc. 2007; 70:274–80.
Article8. Morgan CM, Webb RM, O'Connor GR. Atypical syphilitic cho-rioretinitis and vasculitis. Retina. 1984; 4:225–31.
Article9. Savir H, Kurz O. Fluorescein angiography in syphilitic retinal vasculitis. Ann Ophthalmol. 1976; 8:713–6.10. Lobes LA Jr, Folk JC. Syphilitic phlebitis simulating branch vein occlusion. Ann Ophthalmol. 1981; 13:825–7.11. Yokoi M, Kase M. Retinal vasculitis due to secondary syphilis. Jpn J Ophthalmol. 2004; 48:65–7.
Article12. Lee MJ, Park YG, Ahn JK. Isolated cilioretinal artery occlusion in pseudoexfoliation syndrome: A case report. J Korean Ophthalmol Soc. 2006; 47:1686–90.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Cilioretinal Artery Occlusion in Pseudoexfoliation Syndrome: A Case Report
- A Case of Cilioretinal Artery Occlusion Associated with Central Retinal Vein Occlusion
- A Case of Ocular Ischemic Syndrome Associated with Multiple Branch Retinal Artery Occlusion and Neovascular Glaucoma
- A Clinical Study of 36 Cases of Retinal Artery Occlusion
- Central retinal vein occlusion combined with cilioretinal artery occlusion