J Korean Ophthalmol Soc.
2011 Oct;52(10):1249-1253. 10.3341/jkos.2011.52.10.1249.
A Case of Endogenous Aspergillus Endophthalmitis Associated with Mycotic Cerebral Aneurysm
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Chungbuk National University, Cheongju, Korea. jbchae@chungbuk.ac.kr
- KMID: 2215011
- DOI: http://doi.org/10.3341/jkos.2011.52.10.1249
Abstract
- PURPOSE
To report a case of a endogenous Aspergillus endophthalmitis associated with mycotic cerebral aneurysmal rupture.
CASE SUMMARY
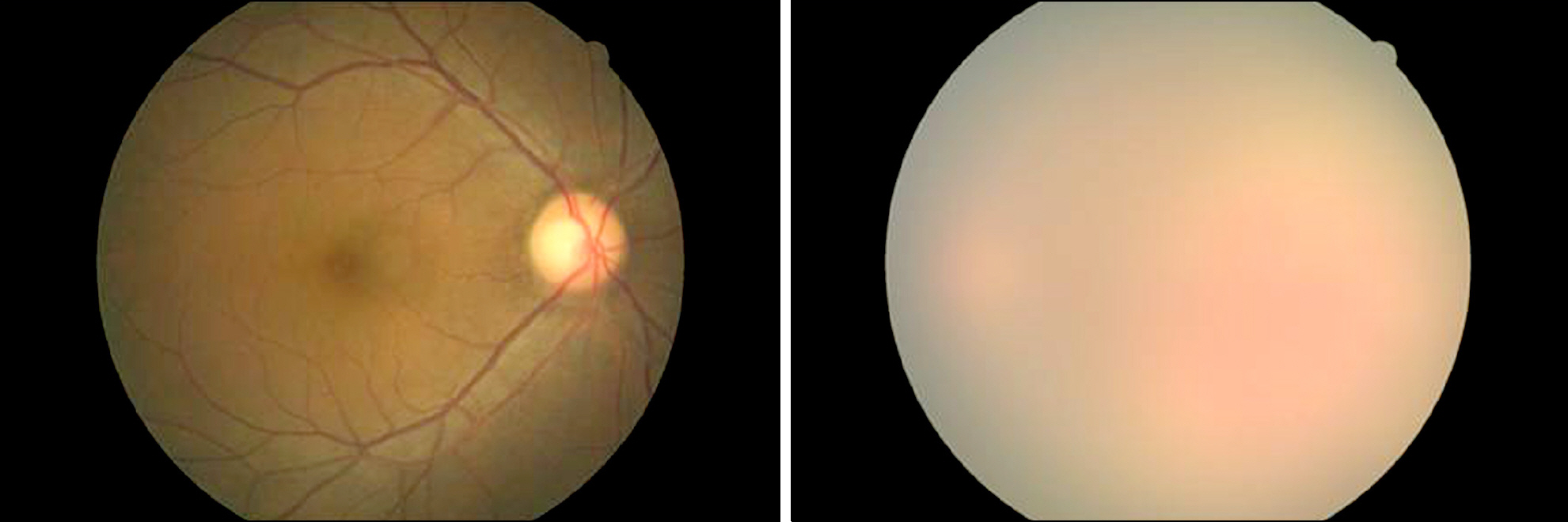
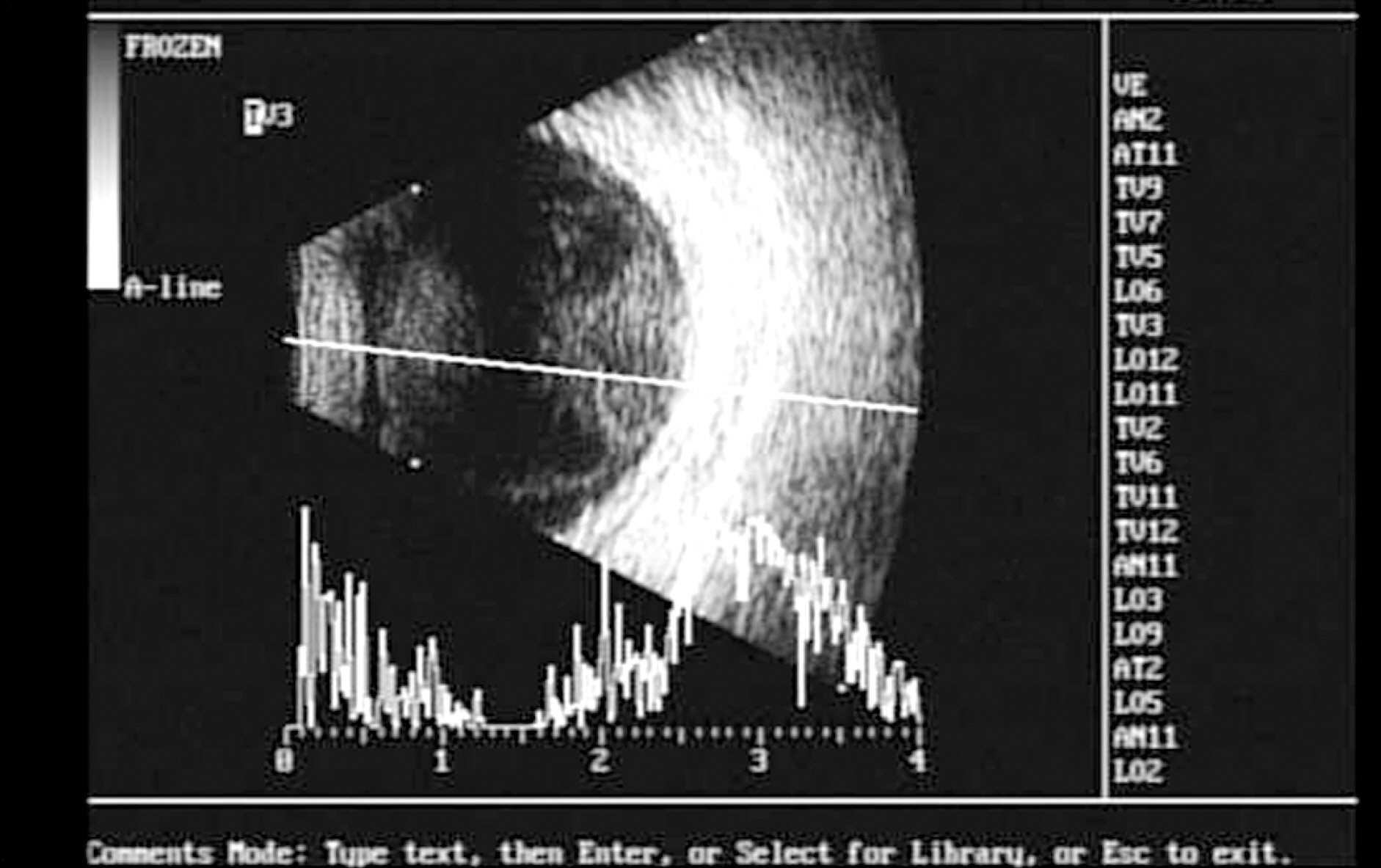
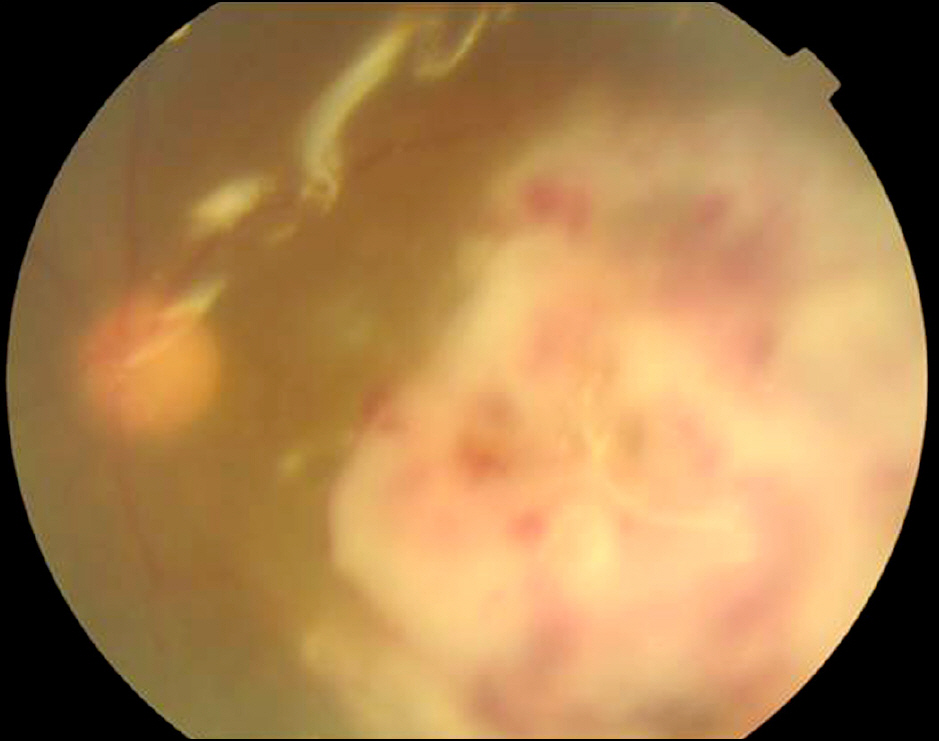
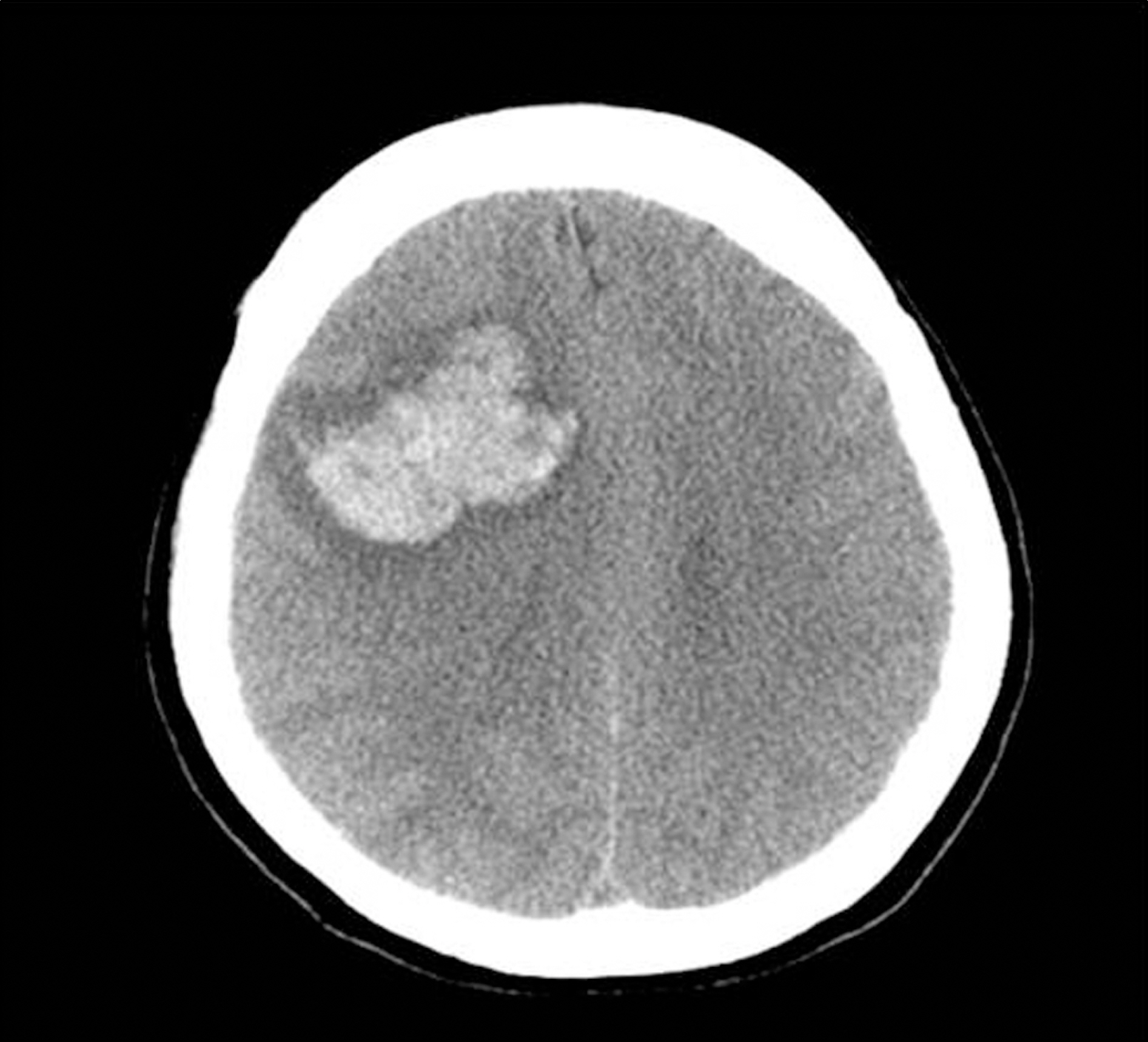
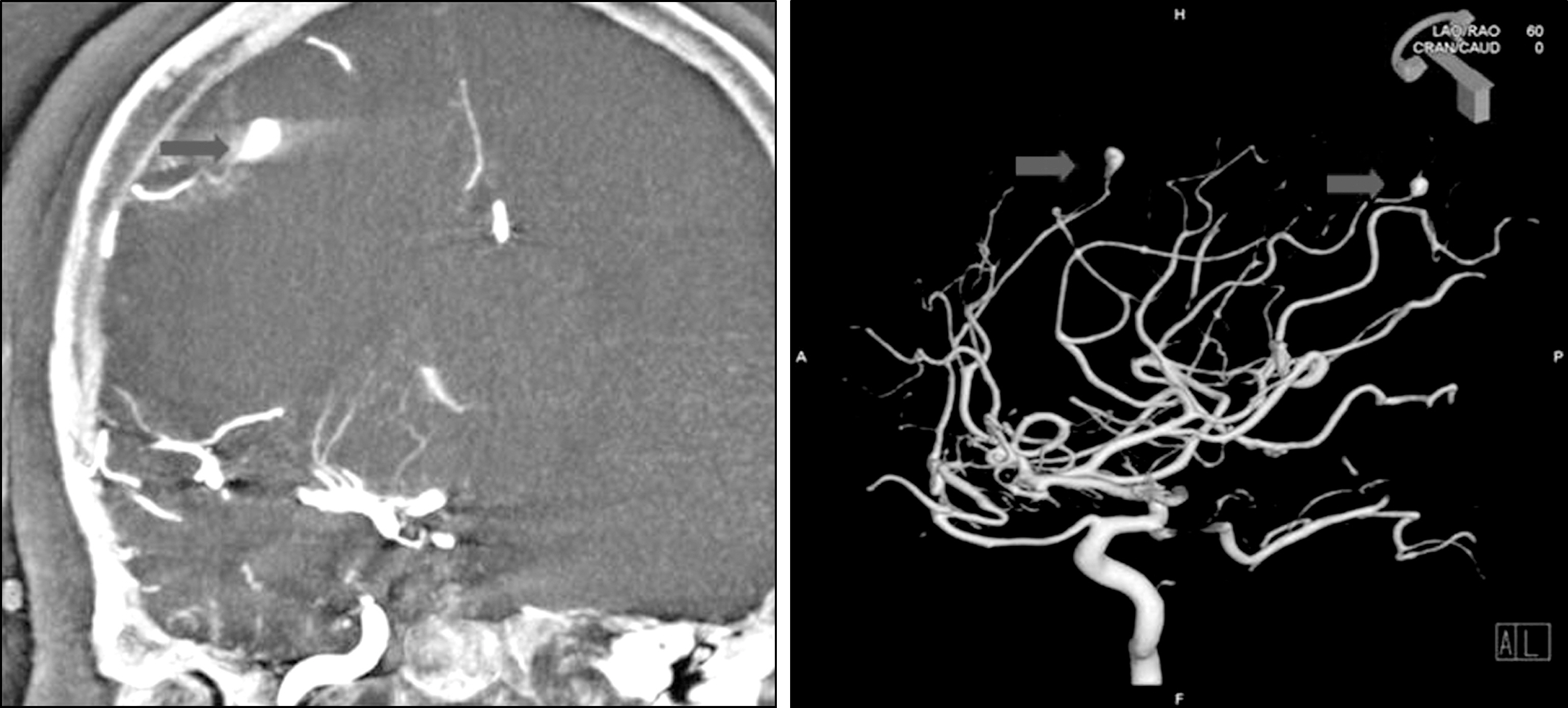
A 51-year-old woman was referred to our retina clinic for decreased visual acuity in the left eye. The patient had previously undergone a liver transplant for liver cirrhosis and hepatocellular carcinoma. On fundus examination, vitreous opacities with a yellowish-white subretinal abscess were observed. There were no abnormal findings except the positive sign in the laboratory serum Aspergillus antigen test performed on admission. Based on the suspicion of endogenous endophthalmitis, pars plana vitrectomy was performed with intravitreal antibiotics injection to treat fungal and bacterial infections. There was no growth in either the vitreous or anterior chamber culture. After vitrectomy, visual acuity improved and the inflammation subsided. However, by the three-week follow-up, acute-onset left hemiplegia with a right hemisphere cerebral hemorrhage had occurred. Cerebral magnetic resonance angiography showed multiple mycotic aneurysms characterized by a large and fusiform appearance. The patient was treated with neuro-embolization and was stabilized with minimal sequalae.
CONCLUSIONS
Although the immunocompromised endophthalmitis patient can be treated using proper management, brain lesions such as mycotic aneurysm may exist and should be carefully considered.
Keyword
MeSH Terms
-
Abscess
Aneurysm
Aneurysm, Infected
Anterior Chamber
Anti-Bacterial Agents
Aspergillus
Bacterial Infections
Brain
Carcinoma, Hepatocellular
Cerebral Hemorrhage
Endophthalmitis
Eye
Female
Follow-Up Studies
Hemiplegia
Humans
Inflammation
Intracranial Aneurysm
Liver
Liver Cirrhosis
Magnetic Resonance Angiography
Middle Aged
Retina
Transplants
Visual Acuity
Vitrectomy
Anti-Bacterial Agents
Figure
Reference
-
References
1. Hassan IJ, MacGowan AP, Cook SD. Endophthalmitis at the Bristol Eye Hospital: an 11 year review of 47 patients. J Hosp Infect. 1992; 22:271–8.2. Irvine WD, Flynn HW Jr, Miller D, Pflugfelder SC. Endophthalmitis caused by gram negative organisms. Arch Ophthalmol. 1992; 110:1450–4.3. Shrader SK, Band JD, Lauter CB, Murphy P. The clinical spectrum of endophthalmitis: incidence, predisposing factors, and features influencing outcome. J Infect Dis. 1990; 162:115–20.
Article4. Bohigian GM, Olk RJ. Factors associated with a poor visual result in endophthalmitis. Am J Ophthalmol. 1986; 101:332–41.
Article5. Greenwald MJ, Wohl LG, Sell CH. Metastatic bacterial endophthalmitis: a contemporary reappraisal. Surv Ophthalmol. 1986; 31:81–101.
Article6. Puliafito CA, Baker AS, Haaf J, Foster CS. Infectious endophthalmitis. Review of 36 cases. Ophthalmology. 1982; 89:921–9.7. Smith SR, Kroll AJ, Lou PL, Ryan EA. Endogenous bacterial and fungal endophthalmitis. Int Ophthalmol Clin. 2007; 47:173–83.
Article8. Liu YC, Cheng DL, Lin CL. Klebsiella pneumoniae liver abscess associated with septic endophthalmitis. Arch Intern Med. 1986; 146:1913–6.
Article9. O'Brien CJ, Kyle GM. Metastatic Staphylococcus aureus endophthalmitis: a case report. Br J Ophthalmol. 1988; 72:189–91.10. Liao HR, Lee HW, Leu HS, et al. Endogenous Klebsiella pneumoniae endophthalmitis in diabetic patients. Can J Ophthalmol. 1992; 27:143–7.11. Jackson TL, Eykyn SJ, Graham EM, Stanford MR. Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Surv Ophthalmol. 2003; 48:403–23.
Article12. Binder MI, Chua J, Kaiser PK, et al. Endogenous endophthalmitis: an 18-year review of culture-positive cases at a tertiary care center. Medicine (Baltimore). 2003; 82:97–105.13. Okada AA, Johnson RP, Liles WC, et al. Endogenous bacterial endophthalmitis: report of a ten-year retrospective study. Ophthalmology. 1994; 101:832–8.14. Schiedler V, Scott IU, Flynn HW Jr, et al. Culture-proven endogenous endophthalmitis: clinical features and visual acuity outcomes. Am J Ophthalmol. 2004; 137:725–31.
Article15. Hwang JH, Cho NC. Prognostic factors in patients with endogenous endophthalmitis. J Korean Ophthalmol Soc. 2009; 50:858–63.
Article16. Coskuncan NM, Jabs DA, Dunn JP, et al. The eye in bone marrow transplantation. VI. Retinal complications. Arch Ophthalmol. 1994; 112:372–9.17. Hunt KE, Glasgow BJ. Aspergillus endophthalmitis. An unrecognized endemic disease in orthotopic liver transplantation. Ophthalmology. 1996; 103:757–67.18. Weishaar PD, Flynn HW Jr, Murray TG, et al. Endogenous Aspergillus endophthalmitis. Clinical features and treatment outcomes. Ophthalmology. 1998; 105:57–65.19. Essman TF, Flynn HW Jr, Smiddy WE, et al. Treatment outcomes in a 10 year study of endogenous fungal endophthalmitis. Ophthalmic Surg Lasers. 1997; 28:185–94.20. Barami K, Ko K. Ruptured mycotic aneurysm presenting as an intraparenchymal hemorrhage and nonadjacent acute subdural hem-atoma: case report and review of the literature. Surg Neurol. 1994; 41:290–3.
Article21. Jones HR Jr, Siekert RG, Geraci JE. Neurologic manifestations of bacterial endocarditis. Ann Intern Med. 1969; 71:21–8.
Article22. Kurino M, Kuratsu J, Yamaguchi T, Ushio Y. Mycotic aneurysm accompanied by aspergillotic granuloma: a case report. Surg Neurol. 1994; 42:160–4.
Article23. Ho CL, Deruytter MJ. CNS aspergillosis with mycotic aneurysm, cerebral granuloma and infarction. Acta Neurochir. 2004; 146:851–6.
Article24. Nonaka N, Yamazaki M, Onishi Y, et al. An autopsied case of pachymeningitis associated with a ruptured, cerebral aneurysm due to Aspergillus infection. Rinsho Shinkeigaku. 2001; 41:673–8.25. Kleinschmidt-DeMasters BK. Central nervous system aspergillosis: a 20-year retrospective series. Hum Pathol. 2002; 33:116–24.26. Barrow DL, Prats AR. Infectious intracranial aneurysms: comparison of groups with and without endocarditis. Neurosurgery. 1990; 27:562–72.
Article27. Okada Y, Shima T, Nishida M, et al. Subarachnoid hemorrhage caused by Aspergillus aneurysm as a complication of transcranial biopsy of an orbital apex lesion.case report. Neurol Med Chir. 1998; 38:432–7.28. Corvisier N, Gray F, Gherardi R, et al. Aspergillosis of ethmoid sinus and optic nerve, with arteritis, and rupture of the internal carotid artery. Surg Neurol. 1987; 28:311–5.
Article29. Takeshita M, Izawa M, Kubo O, et al. Aspergillotic aneurysm formation of cerebral artery following neurosurgical operation. Surg Neurol. 1992; 38:146–51.
Article30. Partridge BM, Chin AT. Cerebral aspergilloma. Postgrad Med J. 1981; 57:439–42.
Article31. Sekhar LN, Dujovny M, Rao GR. Carotid-cavernous sinus thrombosis caused by Aspergillus fumigatus. Case report. J Neurosurg. 1980; 52:120–5.32. Piotrowski WP, Pilz P, Chuang IH. Subarachnoid hemorrhage caused by a fungal aneurysm of the vertebral artery as a complication of intracranial aneurysm clipping. Case report. J Neurosurg. 1990; 73:962–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Basilar Artery Mycotic Aneurysm Associated With Aspergillus Endogenous Endophthalmitis
- A Case of Intracranial Mycotic Aneurysm due to Aspergillus species
- A case of mycotic aneurysm of the aorta caused by Klebsiella pneumoniae accompanied by endophthalmitis
- Infected Thoracic Aortic Aneurysm Concurrent with Endophthalmitis by Candida albicans: a Case Report
- A Case of Aspergillus Endocarditis Presenting as Endophthalmitis