J Korean Ophthalmol Soc.
2016 May;57(5):857-861. 10.3341/jkos.2016.57.5.857.
Ocular Syphilis Presenting as both Optic Neuritis and Chorioretinitis in both Eyes
- Affiliations
-
- 1Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. mmk@med.yu.ac.kr
- KMID: 2212733
- DOI: http://doi.org/10.3341/jkos.2016.57.5.857
Abstract
- PURPOSE
To report a patient with ocular syphilis, who showed variable ocular manifestations, including optic neuritis and chorioretinitis in both eyes over a short time period.
CASE SUMMARY
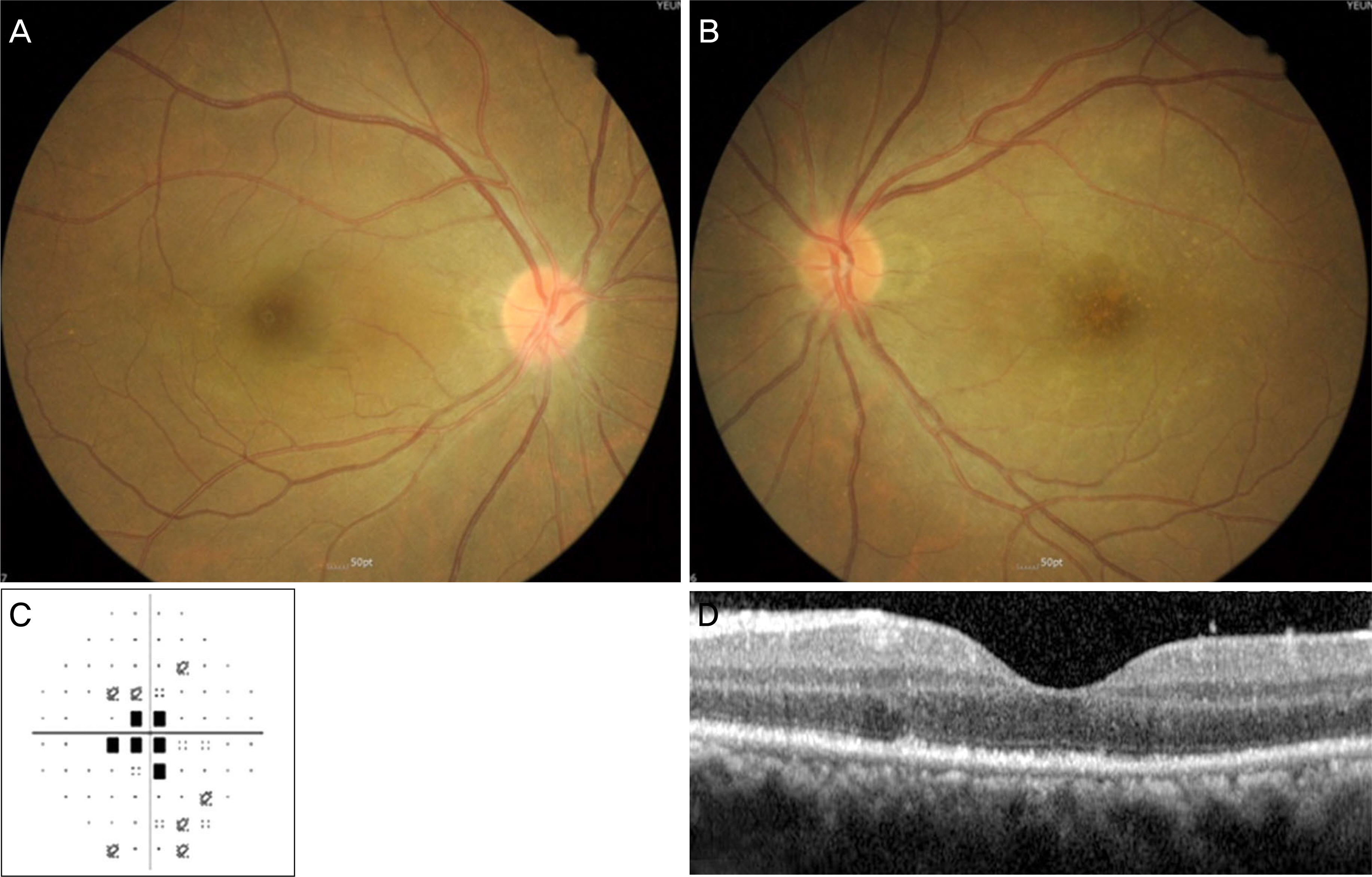
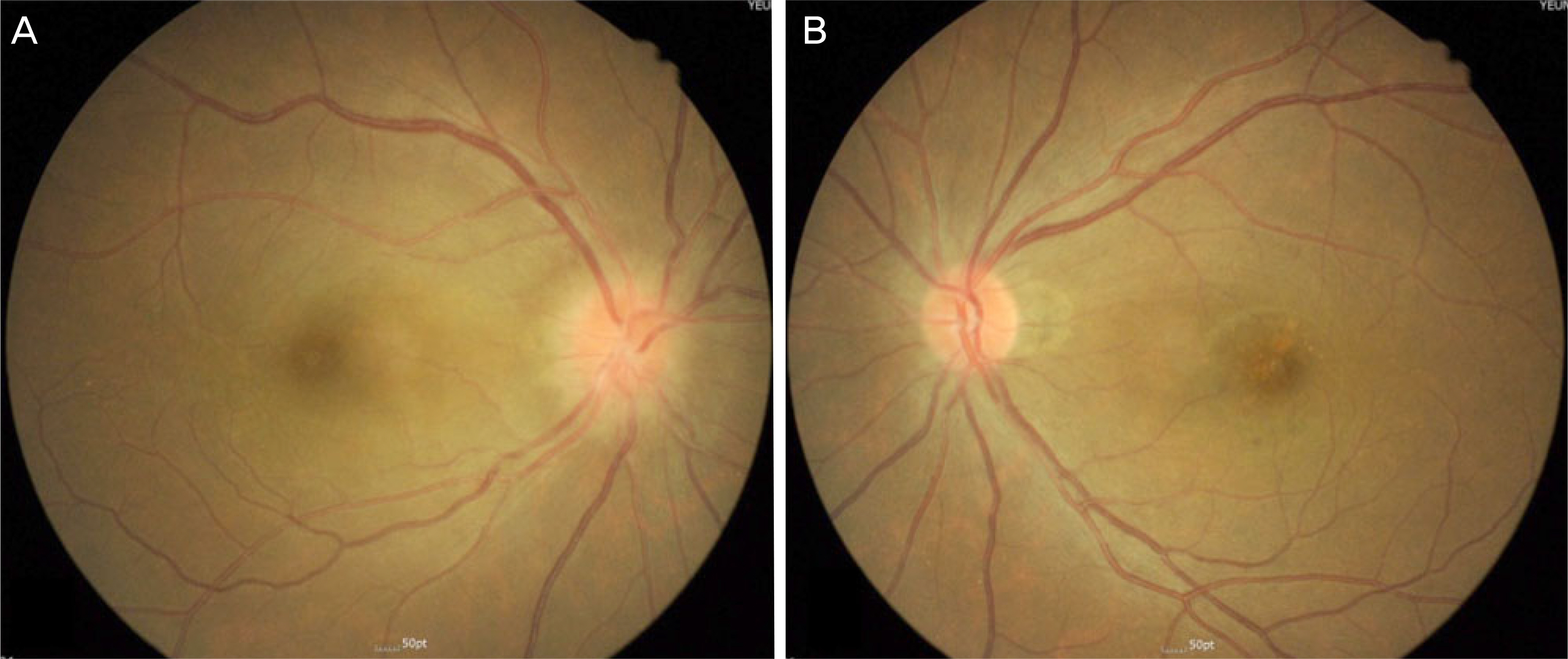
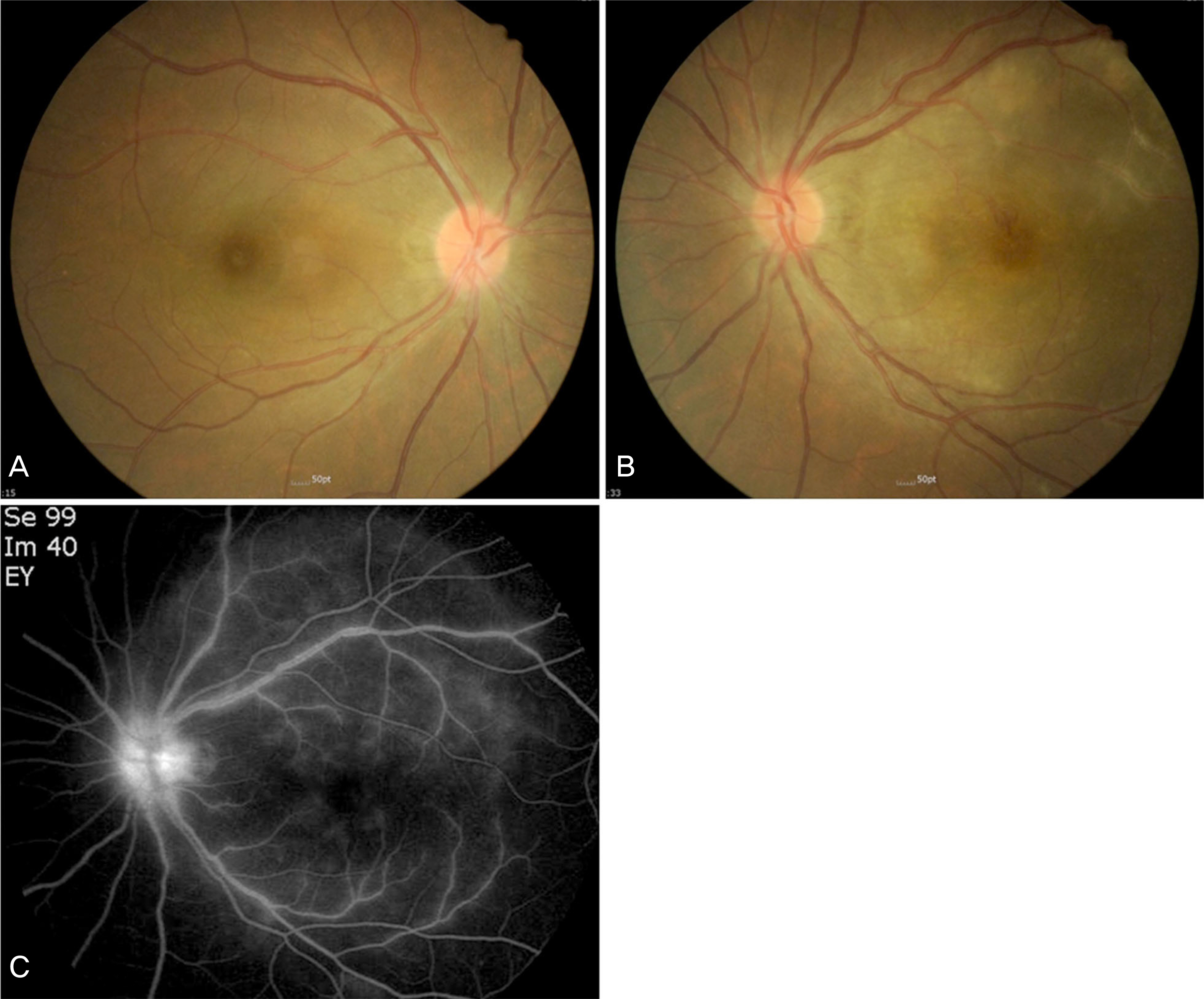
A 44-year-male visited our clinic for central scotoma in the left eye. The visual acuity was 20/25 in the right eye and 20/40 in the left eye. The fundus of the left eye showed a slightly hyperemic optic disc and multiple yellowish deposits. One week later, visual acuity and fundus lesion improved to 20/20 without a definitive treatment. However, 1 month later, he reported a new deterioration of vision in his right eye to 20/40. The right eye had a relative afferent pupillary defect and the fundus examination showed a blurred optic disc margin. Serological work-up was recommended but the patient refused. He returned 3 weeks later with an improvement in the right eye vision (20/25) and a worsening in the left eye (20/200). The examination revealed an improvement of the previously blurred disc margin in the right eye and newly developed chorioretinitis with vasculitis in the left eye. A serological test was performed. The venereal diseases research laboratory titer was 1:32. The fluorescent treponemal antigen absorbance test as positive for IgG and IgM. He was diagnosed with ocular syphilis and referred to the infectious disease department. He was treated with antibiotics. Six months later, the visual acuity was 20/20 in both eyes and the previous fundus lesions had disappeared.
CONCLUSIONS
Ocular syphilis should be considered in patients with atypical and variable clinical course.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Lafond RE. Lukehart SA. Biological basis for syphilis. Clin-Microbiol Rev. 2006; 19:29–49.
Article2. Peeling RW. Hook EW 3rd. The pathogenesis of syphilis: the Great Mimicker, revisited. J Pathol. 2006; 208:224–32.
Article3. Shen J. Feng L. Li Y. Ocular syphilis: an alarming infectious eye disease. Int J Clin Exp Med. 2015; 8:7770–7. eCollection 2015.4. Chen ZQ. Zhang GC. Gong XD, et al. Syphilis in China: results of a national surveillance programme. Lancet. 2007; 369:132–8.
Article5. Chao JR. Khurana RN. Fawzi AA, et al. Syphilis: Reemergence of an old adversary. Ophthalmology. 2006; 113:2074–9. Epub 2006 Aug28.
Article6. Hyun SH. Lee DY. Nam DH. A case of episcleritis as a manifestation of neurosyphilis. J Korean Ophthalmol Soc. 2013; 54:1800–2.
Article7. Lee HJ. Kim MJ. Cha DM, et al. A case of ocular syphilis presenting as bilateral optic neuritis. J Korean Ophthalmol Soc. 2014; 55:1115–20.
Article8. Kim JA. Park KH. Woo SJ. Acase of syphilitic outer retinitis mimicking acute zonal occult outer retinopathy. Korean J Ophthalmol. 2014; 28:497–9.9. Kim EH. Lee JE A case of vitritis as the primary manifestation without retinitis in ocular syphilis with AIDS. J Korean Ophthalmol Soc. 2006; 47:1177–82.10. Eandi CM. Neri P. Adelman RA, et al. Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina. 2012; 32:1915–41.11. Lee SY. Cheng V. Rodger D. Rao N. Clinical and laboratory characteristics of ocular syphilis: a new face in the era of HIV coinfection. J Ophthalmic Inflamm Infect. 2015; 5:26.
Article12. Park JH. Joe SG. Yoon YH. Delayed diagnosis of ocular syphilis that manifested as retinal vasculitis and acute posterior multifocal placoid epitheliopathy. Indian J Ophthalmol. 2013; 61:676–8.
Article13. Li SY. Birnbaum AD. Tessler HH. Goldstein DA. Posterior syphilitic uveitis: clinical characteristics, co-infection with HIV, response to treatment. Jpn J Ophthalmol. 2011; 55:486–94.
Article14. Cho YW. Kim CR. Han YS, et al. Clinical manifestations of ocular syphilis combined with neurosyphilis. J Korean Ophthalmol Soc. 2014; 55:602–7.
Article15. Aranda S. Amer R. Sequential spontaneous resolution of acute syphilitic posterior placoid chorioretinitis. Eur J Ophthalmol. 2015; 25:263–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ocular Syphilis Presenting as Bilateral Optic Neuritis
- A Case of Neurosyphilis with Acute Optic Neuritis and Trochlear Nerve Palsy in Human Immunodeficiency Virus Infected Male
- Presumed Ocular Toxoplasmosis Presenting as Isolated Unilateral Papillitis
- Clinical Manifestations of Idiopathic Optic Perineuritis in Korea
- Clinical Manifestations of Optic Neuritis