J Korean Soc Surg Hand.
2013 Sep;18(3):111-117. 10.12790/jkssh.2013.18.3.111.
Headless Autocompression Screw Fixation of Scaphoid Fractures Using Open Dorsal Approach
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei Univeristy College of Medicine, Seoul, Korea. kangho56@yuhs.ac
- KMID: 2194140
- DOI: http://doi.org/10.12790/jkssh.2013.18.3.111
Abstract
- PURPOSE
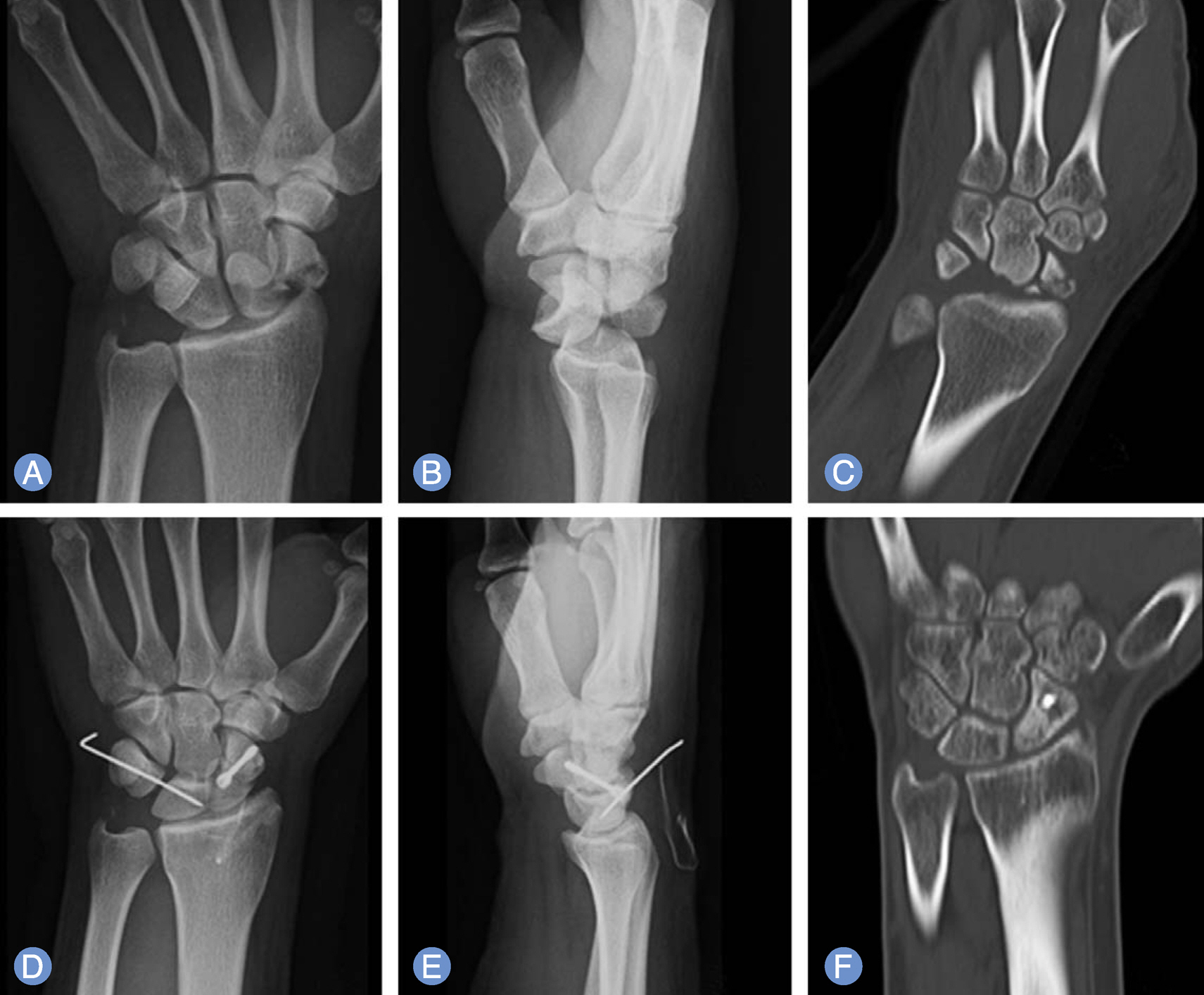
We present the clinical and radiological results of open reduction and internal fixation for scaphoid fracture with retrograde headless screw fixation via dorsal approach.
METHODS
This study carried out a survey targeting 15 patients who have a retrograde headless screw fixation on nonunion of scaphoid fracture without previous operation, 2 patients who have a retrograde headless screw fixation on nonunion of scaphoid fracture with previous operation and 8 patients who have a trans-scaphoid perilunate dislocation. We figured out a mechanism of injury, and clinical symptom, radiologic findings. The surgery was done with open dorsal approach which is retrograde headless screw fixation internally, with or without bone graft. We analyzed the result by Maudsley method, in terms of bone union, duration for union, radiologic finding, clinical outcomes.
RESULTS
After surgery, 22 of 25 patients had union result on fracture and other 3 patients had nonunion result. It took 12 weeks to achieve bone union on average. Based on radiograhs, we had one case of partial avascular necrosis of proximal fragment without clinical symptoms. We had one case of each scaphoid nonunion without previous operation, with operation and trans-scaphoid perilunate dislocation had arthritic change and non-symptomatic nonunion result. In terms of clinical outcome, 22 patients showed satisfactory results and 3 patients had slight limitation of range of motion.
CONCLUSION
Retrograde headless screw fixation with or without bone graft for the treatment of scaphoid fracture is recommendable.
Keyword
MeSH Terms
Figure
Reference
-
1. Cooney WP 3rd, Dobyns JH, Linscheid RL. Nonunion of the scaphoid: analysis of the results from bone grafting. J Hand Surg Am. 1980; 5:343–54.
Article2. Gelberman RH, Wolock BS, Siegel DB. Fractures and non-unions of the carpal scaphoid. J Bone Joint Surg Am. 1989; 71:1560–5.
Article3. Bunker TD, McNamee PB, Scott TD. The Herbert screw for scaphoid fractures. A multicentre study. J Bone Joint Surg Br. 1987; 69:631–4.
Article4. Jiranek WA, Ruby LK, Millender LB, Bankoff MS, Newberg AH. Long-term results after Russe bone-grafting: the effect of malunion of the scaphoid. J Bone Joint Surg Am. 1992; 74:1217–28.5. Leslie IJ, Dickson RA. The fractured carpal scaphoid. Natural history and factors influencing outcome. J Bone Joint Surg Br. 1981; 63:225–30.
Article6. Filan SL, Herbert TJ. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg Br. 1996; 78:519–29.
Article7. Barton NJ. Experience with scaphoid grafting. J Hand Surg Br. 1997; 22:153–60.
Article8. DeMaagd RL, Engber WD. Retrograde Herbert screw fixation for treatment of proximal pole scaphoid nonunions. J Hand Surg Am. 1989; 14:996–1003.
Article9. Green DP, O'Brien ET. Open reduction of carpal dislocations: indications and operative techniques. J Hand Surg Am. 1978; 3:250–65.
Article10. Inoue G, Tanaka Y, Nakamura R. Treatment of trans-scaphoid perilunate dislocations by internal fixation with the Herbert screw. J Hand Surg Br. 1990; 15:449–54.
Article11. Moneim MS, Hofammann KE 3rd, Omer GE. Transscaphoid perilunate fracture-dislocation. Result of open reduction and pin fixation. Clin Orthop Relat Res. 1984; (190):227–35.12. Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984; 66:114–23.
Article13. Maudsley RH, Chen SC. Screw fixation in the management of the fractured carpal scaphoid. J Bone Joint Surg Br. 1972; 54:432–41.
Article14. Matti H. Technik and resilte, meiner pseudoarthosen-operation. Z Chir. 1975; 63:1442–53.15. Berger RA. The anatomy of the scaphoid. Hand Clin. 2001; 17:525–32.
Article16. Ruby LK, Stinson J, Belsky MR. The natural history of scaphoid non-union: a review of fifty-five cases. J Bone Joint Surg Am. 1985; 67:428–32.
Article17. Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg Am. 1980; 5:508–13.
Article18. Taleisnik J, Kelly PJ. The extraosseous and intraosseous blood supply of the scaphoid bone. J Bone Joint Surg Am. 1966; 48:1125–37.
Article19. dos Reis FB, Koeberle G, Leite NM, Katchburian MV. Internal fixation of scaphoid injuries using the Herbert screw through a dorsal approach. J Hand Surg Am. 1993; 18:792–7.20. Sukul DM, Johannes EJ, Marti RK. Corticocancellous grafting and an AO/ASIF lag screw for nonunion of the scaphoid: a retrospective analysis. J Bone Joint Surg Br. 1990; 72:835–8.
Article21. Botte MJ, Mortensen WW, Gelberman RH, Rhoades CE, Gellman H. Internal vascularity of the scaphoid in cadavers after insertion of the Herbert screw. J Hand Surg Am. 1988; 13:216–20.
Article22. Green DP. The effect of avascular necrosis on Russe bone grafting for scaphoid nonunion. J Hand Surg Am. 1985; 10:597–605.
Article23. Fernandez DL, Eggli S. Non-union of the scaphoid. Revascularization of the proximal pole with implantation of a vascular bundle and bone-grafting. J Bone Joint Surg Am. 1995; 77:883–93.
Article24. Robbins RR, Ridge O, Carter PR. Iliac crest bone grafting and Herbert screw fixation of nonunions of the scaphoid with avascular proximal poles. J Hand Surg Am. 1995; 20:818–31.
Article25. Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg Br. 2002; 27:498–502.
Article26. Apergis E, Maris J, Theodoratos G, Pavlakis D, Antoniou N. Perilunate dislocations and fracture-dislocations. Closed and early open reduction compared in 28 cases. Acta Orthop Scand Suppl. 1997; 275:55–9.27. Kardashian G, Christoforou DC, Lee SK. Perilunate dislocations. Bull NYU Hosp Jt Dis. 2011; 69:87–96.28. Trumble T. Carpal fracture-dislocations. Rosemont: American Academy of Orthopaedic Surgeons;2002.29. Moneim MS. Management of greater arc carpal fractures. Hand Clin. 1988; 4:457–67.
Article30. Ritt MJ, Bishop AT, Berger RA, Linscheid RL, Berglund LJ, An KN. Lunotriquetral ligament properties: a comparison of three anatomic subregions. J Hand Surg Am. 1998; 23:425–31.
Article31. Budoff JE. Treatment of acute lunate and perilunate dislocations. J Hand Surg Am. 2008; 33:1424–32.
Article32. Bedi A, Jebson PJ, Hayden RJ, Jacobson JA, Martus JE. Internal fixation of acute, nondisplaced scaphoid waist fractures via a limited dorsal approach: an assessment of radiographic and functional outcomes. J Hand Surg Am. 2007; 32:326–33.
Article33. Trumble T, Nyland W. Scaphoid nonunions. Pitfalls and pearls. Hand Clin. 2001; 17:611–24.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Scaphoid Nonunion: Herbert Screw Fixation through Dorsal Approach
- Minimal Invasive Fixation Methods for the Metacarpal Fracture
- Modified Volar Percutaneous Screw Fixation for the Scaphoid Fractures: Trans-trapezial Approach
- Treatment of Acute Scaphoid Fracture by Percutaneus Acutrak Screw Insertion
- Preservation of Scaphoid in Scaphoid Nonunion Advanced Collapse Stage II and III