J Korean Neurotraumatol Soc.
2010 Jun;6(1):18-22. 10.13004/jknts.2010.6.1.18.
Primary Traumatic Brainstem Hematomas: Consideration for the Causal Relation
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University College of Medicine, Buheon Hospital, Bucheon, Korea. sunchulh@sch.ac.kr
- KMID: 2192355
- DOI: http://doi.org/10.13004/jknts.2010.6.1.18
Abstract
OBJECTIVE
Traumatic primary brainstem hematomas are thought to be a rare phenomenon. The study is to report five cases with review of literatures and to discuss how to write the medical certificates.
METHODS
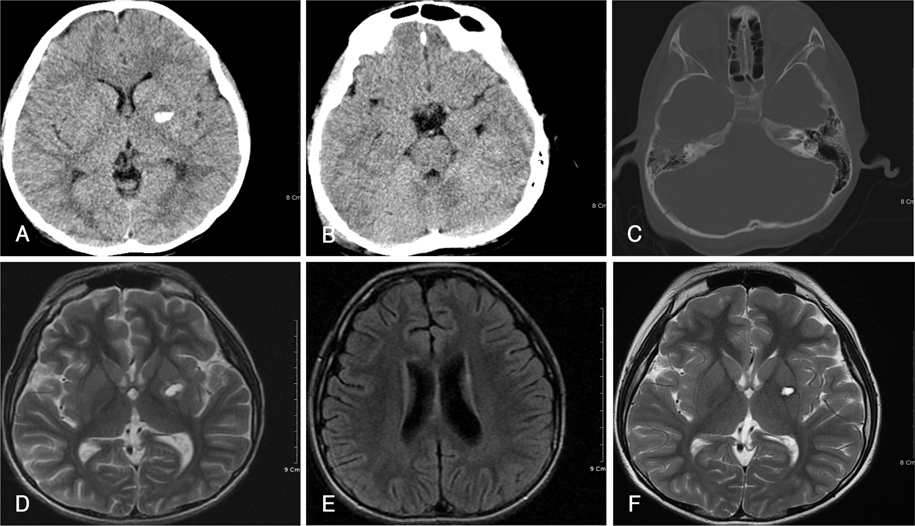
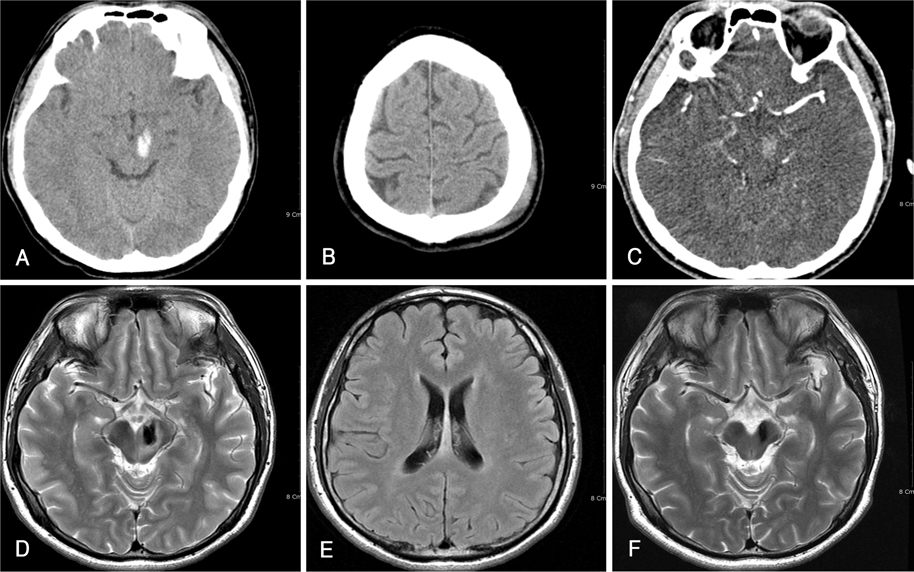
Five cases were retrospectively reviewed, who had not associated intracranial lesions except the hematoma in the brain stem. All cases were analyzed with external wounds, skull fracture, MRI findings, and outcome.
RESULTS
The hematomas occurred in 1 in pons, 2 in midbrain, 1 in thalamus, and 1 in putamen. All of the cases complained of decreased consciousness and denied any neurological symptoms before trauma. Skull fracture was involved only in 2 cases. The finding of MRI revealed signal changes on the corpus callosum compatible with diffuse axonal injury only in 2 cases. Three cases took twice of MRI, which confirmed the hematoma absorbed. The recovery was uneventful and all of them returned to their jobs.
CONCLUSION
Primary brainstem hematomas are not always accompanied with skull fracture or diffuse axonal injury in MRI. Even though it occurs extremely rare, the cause of the hematomas can be described as a trauma in the medical certificates based on the history and the radiological images.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Nail Gun Induced Open Head Injury: A Case Report
Hyun Ho Oh, Young Kim, Sung Choon Park, Young Soo Ha, Kyu Chang Lee
Korean J Neurotrauma. 2014;10(2):139-141. doi: 10.13004/kjnt.2014.10.2.139.
Reference
-
1. Bhatoe HS. Primary brainstem injury: benign course and improved survival. Acta Neurochir (Wien). 1999; 141:515–519.
Article2. Clifton GL, McCormick WF, Grossman RG. Neuropathology of early and late deaths after head injury. Neurosurgery. 1981; 8:309–314.
Article3. Eo W, Lee HK, Cho BK, Sim BS. CT findings of primary brainstem injury: case report. J Korean Neurosurg Soc. 1981; 10:205–210.4. Gennarelli TA, Thibault LE, Adams JH, Graham DI, Thompson CJ, Marcincin RP. Diffuse axonal injury and traumatic coma in the primate. Ann Neurol. 1982; 12:564–574.
Article5. Gentry LR, Godersky JC, Thompson B. MR imaging of head trauma: review of the distribution and radiopathologic features of traumatic lesions. AJR Am J Roentgenol. 1988; 150:663–672.
Article6. Lee JS, Lee MS, Kim YG, Kim DH. Unusual movement disorders in a patient with traumatic mesencephalic Hemorrhage. J Korean Neurol Assoc. 1993; 11:261–264.7. Hashimoto T, Nakamura N, Richard KE, Frowein RA. Primary brain stem lesions caused by closed head injuries. Neurosurg Rev. 1993; 16:291–298.
Article8. Lee KS, Bae HG, Yun IG. A design for differentiation of traumatic and spontaneous intracerebral hemorrhages. J Korean Med Assoc. 1988; 31:535–542.9. Mitchell DE, Adams JH. Primary focal impact damage to the brainstem in blunt head injuries. Does it exist? Lancet. 1973; 2:215–218.10. Moon KJ. Essential points for medical certification on diseases. J Korean Med Assoc. 1983; 26:145–149.11. Kim SJ, Suh DC, Park CK, Hwang WC, Park MS. MR findings of brainstem injury. J Korean Radiol Soc. 1995; 32:237–241.
Article12. Rich JR, Gregorius FK, Hepler RS. Bilateral internuclear ophthalmoplegia after trauma. Arch Ophthalmol. 1974; 92:66–68.
Article13. Saeki N, Yamaura A, Sunami K. Brain stem contusion due to tentorial coup injury: case report and pathomechanical analysis from normal cadavers. Br J Neurosurg. 1998; 12:151–155.14. Se YB, Kim CH, Bak KH, Kim JM. Traumatic brainstem hemorrhage presenting with hemiparesis. J Korean Neurosurg Soc. 2009; 45:176–178.
Article15. Shibata Y, Matsumura A, Meguro K, Narushima K. Differentiation of mechanism and prognosis of traumatic brain stem lesions detected by magnetic resonance imaging in the acute stage. Clin Neurol Neurosurg. 2000; 102:124–128.
Article16. Thompson RK, Salcman M. Dynamic axial brain stem distortion as a mechanism in the production of brain stem hemorrhages: role of the carotid arteries. Neurosurgery. 1988; 22:629–632.
Article17. Tsai FY, Teal JS, Quinn MF, Itabashi HH, Huprich JE, Ahmadi J, et al. CT of brainstem injury. AJR Am J Roentgenol. 1980; 134:717–723.
Article18. Woischneck D, Klein S, Reissberg S, Peters B, Avenarius S, Günther G, et al. Prognosis of brain stem lesion in children with head injury. Childs Nerv Syst. 2003; 19:174–178.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computed tomography (CT) of the spontaneous resolution of traumatic epidural and subdural hematoma
- MR Findings of Brainstem Injury
- Delayed Post-traumatic Extradural Hematomas: Delayed Bleeding & Delayed Expansion
- Intracerebral Hematoma Caused by Ruptured Traumatic Pseudoaneurysm of the Middle Meningeal Artery: A Case Report
- Traumatic Intracerebellar Hematomas