J Korean Neurosurg Soc.
2014 Apr;55(4):200-204. 10.3340/jkns.2014.55.4.200.
Sensory Complications in Patients after Scalp Mass Excision and Its Anatomical Considerations
- Affiliations
-
- 1Department of Neurosurgery, Chuncheon Sacred Heart Hospital, College of Medicine, Hallym University, Chuncheon, Korea. choihyukjai@yahoo.co.kr
- KMID: 2191092
- DOI: http://doi.org/10.3340/jkns.2014.55.4.200
Abstract
OBJECTIVE
To evaluate the incidence of postsurgical sensory complications in patients with scalp masses and classify the locations of them from a surgical standpoint according to anatomical considerations.
METHODS
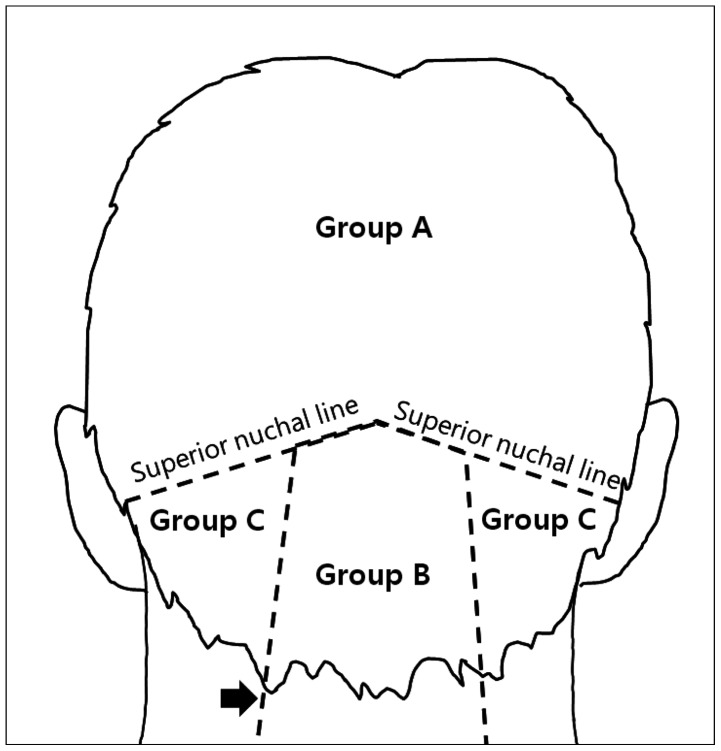
A total of 121 patients who underwent surgery for scalp mass were included in this study. The authors reviewed medical records and preoperative radiologic images. We investigated the complications related to sensory changes after procedure. Enrolled patients have been divided into three groups. Group A included patients with tumors above the superior nuchal line (SNL), Group B with tumors within the trapezius muscle area and patients who had tumors on the lateral trapezius muscle area were assigned to Group C. We compared the incidence related to postoperative sensory complications and summarized their additional treatments for these with clinical outcome.
RESULTS
There were 12 patients (10%) with sensory complications related on the mass excision site (Group A: 1 patient, Group B: 2 patients, Group C: 9 patients). Six patients were affected with lesser occipital nerve (LON), 2 patients on greater occipital nerve (GON) and 4 patients on GON and LON. Over 6 months after surgery, two of the twelve patients with sensory complications did not have complete recovered pain in spite of proper medications and local chemical neurolysis with 1.0% lidocaine and dexamethasone.
CONCLUSION
Occipital neuropathy should be considered as a complication related excision of scalp mass. The sensory complications are more frequent in Group C because of the anatomical characteristics of the occipital nerves and there were no statistical difference for other variables.
Keyword
MeSH Terms
Figure
Reference
-
1. Ahn NU, Ahn UM, Ipsen B, An HS. Mechanical neck pain and cervicogenic headache. Neurosurgery. 2007; 60(1 Supp1 1):S21–S27. PMID: 17204881.2. Arai T, Ishikawa K, Saito T, Hashimoto Y, Asai T, Okuda Y. Distance from the external occipital protuberance to the occipital artery for occipital nerve block. J Anesth. 2013; 27:801–802. PMID: 23475441.
Article3. Biousse V, D'Anglejan-Chatillon J, Massiou H, Bousser MG. Head pain in non-traumatic carotid artery dissection: a series of 65 patients. Cephalalgia. 1994; 14:33–36. PMID: 8200023.
Article4. Choi HJ, Oh IH, Choi SK, Lim YJ. Clinical outcomes of pulsed radiofrequency neuromodulation for the treatment of occipital neuralgia. J Korean Neurosurg Soc. 2012; 51:281–285. PMID: 22792425.
Article5. Conroy E, Laing A, Kenneally R, Poynton AR. C1 lateral mass screw-induced occipital neuralgia: a report of two cases. Eur Spine J. 2010; 19:474–476. PMID: 19856190.
Article6. Diamond MP, Freeman ML. Clinical implications of postsurgical adhesions. Hum Reprod Update. 2001; 7:567–576. PMID: 11727865.
Article7. Ducic I, Moriarty M, Al-Attar A. Anatomical variations of the occipital nerves: implications for the treatment of chronic headaches. Plast Reconstr Surg. 2009; 123:859–863. discussion 864. PMID: 19319048.
Article8. Gille O, Lavignolle B, Vital JM. Surgical treatment of greater occipital neuralgia by neurolysis of the greater occipital nerve and sectioning of the inferior oblique muscle. Spine (Phila Pa 1976). 2004; 29:828–832. PMID: 15087807.
Article9. Gunnarsson T, Massicotte EM, Govender PV, Raja Rampersaud Y, Fehlings MG. The use of C1 lateral mass screws in complex cervical spine surgery: indications, techniques, and outcome in a prospective consecutive series of 25 cases. J Spinal Disord Tech. 2007; 20:308–316. PMID: 17538356.
Article10. Haldeman S, Dagenais S. Cervicogenic headaches: a critical review. Spine J. 2001; 1:31–46. PMID: 14588366.11. Hammond SR, Danta G. Occipital neuralgia. Clin Exp Neurol. 1978; 15:258–270. PMID: 756019.12. International Headache Society Headache Classification Subcommittee. The International Classification of Headache Disorders. ed 2. Oxford: Blackwell Pub;2004.13. Jeon SJ, Park SH, Ryu KS, Cho BM, Oh SM. Clinical and radiological analysis of scalp masses. J Korean Neurosurg Soc. 2002; 32:559–563.14. Jung SJ, Moon SK, Kim TY, Eom KS. A case of occipital neuralgia in the greater and lesser occipital nerves treated with neurectomy by using transcranial Doppler sonography: technical aspects. Korean J Pain. 2011; 24:48–52. PMID: 21390179.
Article15. Jürgens TP, Müller P, Seedorf H, Regelsberger J, May A. Occipital nerve block is effective in craniofacial neuralgias but not in idiopathic persistent facial pain. J Headache Pain. 2012; 13:199–213. PMID: 22383125.
Article16. Lucchesi C, Puglioli M, Gori S. Occipital neuralgia: a symptomatic case caused by an abnormal left vertebral artery. Neurol Sci. 2013; 34:243–245. PMID: 22311642.
Article17. Mosser SW, Guyuron B, Janis JE, Rohrich RJ. The anatomy of the greater occipital nerve: implications for the etiology of migraine headaches. Plast Reconstr Surg. 2004; 113:693–697. discussion 698-700. PMID: 14758238.
Article18. Park TS, Kim YS. Neuropraxia of the cutaneous nerve of the cervical plexus after shoulder arthroscopy. Arthroscopy. 2005; 21:631. PMID: 15891736.
Article19. Rhee WT, You SH, Kim SK, Lee SY. Troublesome occipital neuralgia developed by c1-c2 harms construct. J Korean Neurosurg Soc. 2008; 43:111–113. PMID: 19096615.
Article20. Shavell VI, Saed GM, Diamond MP. Review: cellular metabolism: contribution to postoperative adhesion development. Reprod Sci. 2009; 16:627–634. PMID: 19293132.
Article21. Tahir M, Corbett S. Lesser occipital nerve neurotmesis following shoulder arthroscopy. J Shoulder Elbow Surg. 2013; 22:e4–e6. PMID: 23352479.
Article22. Trabold O, Wagner S, Wicke C, Scheuenstuhl H, Hussain MZ, Rosen N, et al. Lactate and oxygen constitute a fundamental regulatory mechanism in wound healing. Wound Repair Regen. 2003; 11:504–509. PMID: 14617293.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Excision of a Cirsoid Aneurysm of the Scalp after Proximal Ligation of the Main Feeder: Case Report
- Surgical Technique Applying Mosquito Forceps to Galeotomies for Scalp Reconstruction
- Clinical and Radiological Analysis of Scalp Masses
- Successful replantation of an avulsed frontal scalp through microvascular anastomoses of only one artery and one vein: a case report
- Simplified V-Shape Incision Technique for Saving Hair Follicles