J Gynecol Oncol.
2008 Dec;19(4):246-250. 10.3802/jgo.2008.19.4.246.
Comparison of modified Cherney incision and vertical midline incision for management of early stage cervical cancer
- Affiliations
-
- 1Women's Cancer Clinic, Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea. ytkchoi@yuhs.ac
- 2Department of Gynecologic Oncology, Kwandong University College of Medicine, Goyang, Korea.
- KMID: 2173414
- DOI: http://doi.org/10.3802/jgo.2008.19.4.246
Abstract
OBJECTIVE
The aim of this study was to compare operative feasibility and surgical outcome of the modified Cherney incision and vertical midline incision in patients undergoing radical hysterectomy and pelvic lymphadenectomy.
METHODS
Between March 2005 and December 2007, retrospective data of 78 patients (n=17; modified Cherney incision, n=61; vertical midline incision) with early stage cervical cancer who received radical hysterectomy and pelvic lymphadenectomy were reviewed.
RESULTS
Baseline characteristics of patients who underwent modified Cherney incision and vertical midline incision were similar except for age (mean+/-SD: 32.3+/-3.4 yr vs. 52.5+/-8.4 yr, p<0.001). Patients who received modified Cherney incision had earlier initiation of soft diet (mean+/-SD: 46.5+/-19.5 hr vs. 56.4+/-25.4 hr, p<0.016) and shorter hospital stay compared to those who received vertical midline incision (mean+/-SD: 18.0+/-4.8 days vs. 21.7+/-3.7 days, p<0.042). There was no difference in the number of dissected pelvic lymph nodes, hemoglobin change, postoperative pain, postoperative ileus, Foley indwelling duration, and perioperative complications.
CONCLUSION
Excluding the selection bias for age, there was no significant difference of the clinical outcome between the modified Cherney incision group and the vertical midline incision group. Modified Cherney incision can be cosmetically performed in young age women obtaining equal number of lymph nodes without increased operative morbidity compared to vertical midline incision.
MeSH Terms
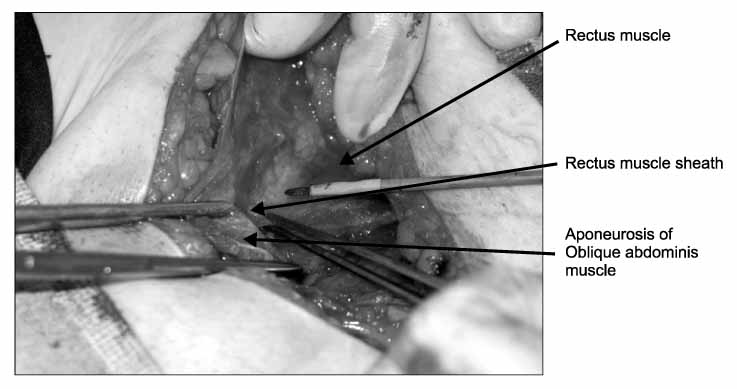
Figure
Reference
-
1. Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007. 57:43–66.2. Cherney LS. New transverse low abdominal incision. Cal West Med. 1943. 59:215–218.3. Burch JC, Lavely HT, Bradley CF. A clinical evaluation of Cherney's incision. Ann Surg. 1948. 127:830–835.4. Berek JS, Hacker NF. Practical gynecologic oncology. 1994. Baltimore: William & Wilkins;249.5. Delgado G, Bundy BN, Fowler WC Jr, Stehman FB, Sevin B, Creasman WT, et al. A prospective surgical pathological study of stage I squamous carcinoma of the cervix: A Gynecologic Oncology Group Study. Gynecol Oncol. 1989. 35:314–320.6. Choi HJ, Roh JW, Seo SS, Lee S, Kim JY, Kim SK, et al. Comparison of the accuracy of magnetic resonance imaging and positron emission tomography/computed tomography in the presurgical detection of lymph node metastases in patients with uterine cervical carcinoma: A prospective study. Cancer. 2006. 106:914–922.7. Mann WJ Jr, Orr JW Jr, Shingleton HM, Austin JM Jr, Hatch KD, Taylor PT, et al. Perioperative influences on infectious morbidity in radical hysterectomy. Gynecol Oncol. 1981. 11:207–212.8. Photopulos GJ, Zwaag RV. Class II radical hysterectomy shows less morbidity and good treatment efficacy compared to class III. Gynecol Oncol. 1991. 40:21–24.9. Helmkamp BF, Krebs HB. The Maylard incision in gynecologic surgery. Am J Obstet Gynecol. 1990. 163:1554–1557.10. Orr JW Jr, Orr PJ, Bolen DD, Holimon JL. Radical hysterectomy: Does the type of incision matter? Am J Obstet Gynecol. 1995. 173:399–405.11. Park JM, Lim JI, Park DJ, Park HK, Jeong DH, Kim KT. A comparison of the Pfannenstiel incision and vertical midline incision for radical hysterectomy and pelvic lymphadenectomy. Korean J Obstet Gynecol. 2003. 46:2441–2445.12. De Lia JE, Michelin DP, Johnson SC, Kajdacsy-Balla A. Cherney versus midline vertical incision for myomectomy or hysterectomy of a significantly enlarged uterus. Am J Obstet Gynecol. 1995. 173:1714–1717.13. Tobin GR, Day TG. Vaginal and pelvic reconstruction with distally based rectus abdominis myocutaneous flaps. Plast Reconstr Surg. 1988. 81:62–73.14. Gleeson NC. A modification of the Cherney incision in gynaecological oncology surgery. Br J Obstet Gynaecol. 1995. 102:925–926.15. Trott E, Welgoss J, Trott AA. The Cherney incision for removal of a large pelvic mass: A case report. Del Med J. 1994. 66:213–215.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of the Pfannenstiel Incision and Vertical Midline Incision for Radical Hysterectomy and Pelvic Lymphadenectomy
- Studies on the Intrasinusal Pyelolithotomy: II. Clinical observation on intrasinusal pyelolithotomy
- Nephropexy by Posterior Vertical Incision
- Posterior Vertical Approach for Sacrococcygeal Teratomas in Children
- Clinical Experience of Ureterolithotomy by Posterior Vertical Incision