Healthc Inform Res.
2015 Oct;21(4):299-306. 10.4258/hir.2015.21.4.299.
Evaluation of Mobile Health Applications Developed by a Tertiary Hospital as a Tool for Quality Improvement Breakthrough
- Affiliations
-
- 1Department of Biomedical Informatics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. rufiji@gmail.com
- 2Department of Breast and Endocrine Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Ubiquitous Health Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Medical Information Office, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 5Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 6Department of Biomedical Engineering, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 7Department of Endocrinology/Metabolism, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 8Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 9Division of General Medicine and Primary Care, Department of Medicine, Brigham and Women's Hospital, Boston, MA, USA.
- KMID: 2166880
- DOI: http://doi.org/10.4258/hir.2015.21.4.299
Abstract
OBJECTIVES
To evaluate the mobile health applications (apps) developed by a single tertiary hospital in Korea with a particular focus on quality and patient safety.
METHODS
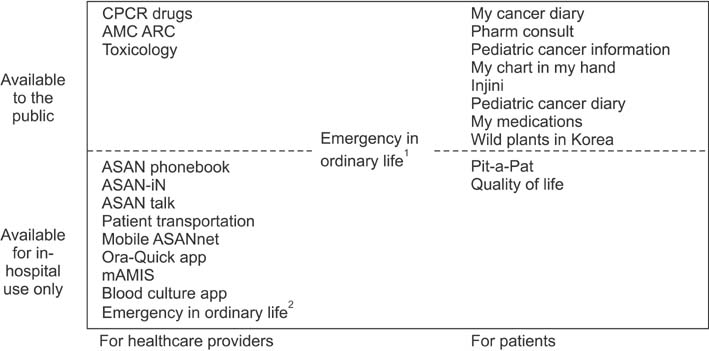
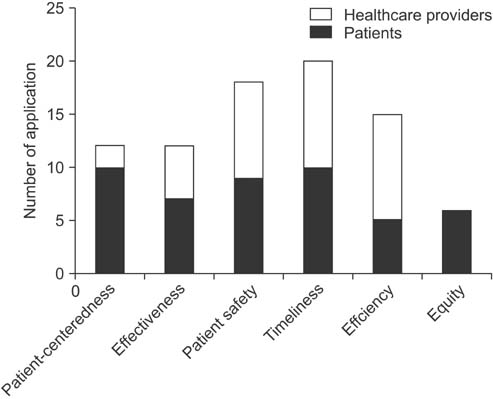
Twenty-three mobile health apps developed by Asan Medical Center were selected for analysis after exclusion of the apps without any relationship with healthcare or clinical workflow, the apps for individual usage, and the mobile Web apps. Two clinical informaticians independently evaluated the apps with respect to the six aims for quality improvement suggested by the United States Institute of Medicine. All discrepancies were resolved after discussion by the two reviewers. The six aims observed in the apps were reviewed and compared by target users.
RESULTS
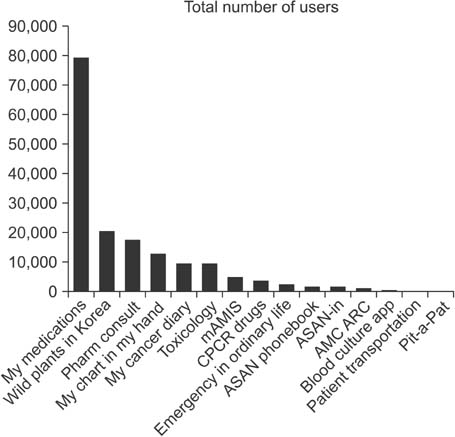
Eleven apps targeted patients, the other 12 were designed for healthcare providers. Among the apps for patients, one app also had functions for healthcare providers. 'My cancer diary' and 'My chart in my hand' apps matched all the six aims. Of the six aims, Timeliness was the most frequently observed (20 apps), and Equity was the least observed (6 apps). Timeliness (10/11 vs. 10/12) and Patient safety (10/11 vs. 9/12) were frequently observed in both groups. In the apps for patients, Patient-centeredness (10/11 vs. 2/12) and Equity (6/11 vs. 0/12) were more frequent but Efficiency (5/11 vs. 10/12) was less frequent.
CONCLUSIONS
Most of the six aims were observed in the apps, but the extent of coverage varied. Further studies, evaluating the extent to which they improve quality are needed.
MeSH Terms
Figure
Cited by 2 articles
-
Future of the Smartphone for Patients and Healthcare Providers
Jae-Ho Lee
Healthc Inform Res. 2016;22(1):1-2. doi: 10.4258/hir.2016.22.1.1.Evaluating the Landscape of Personal Health Records in Korea: Results of the National Health Informatization Survey
Kyehwa Lee, Yura Lee, Jae-Ho Lee
Healthc Inform Res. 2023;29(4):386-393. doi: 10.4258/hir.2023.29.4.386.
Reference
-
1. Lee Y, Chang H. Ubiquitous health in Korea: progress, barriers, and prospects. Healthc Inform Res. 2012; 18(4):242–251.
Article2. Shin SY, Lee JH. Mobile health: a new breakthrough for u-health. Telecommun Rev. 2013; 23(3):8.3. Silva BM, Rodrigues JJ, de la Torre Diez I, Lopez-Coronado M, Saleem K. Mobile-health: a review of current state in 2015. J Biomed Inform. 2015; 56:265–272.
Article4. Ricciardi L, Mostashari F, Murphy J, Daniel JG, Siminerio EP. A national action plan to support consumer engagement via e-health. Health Aff (Millwood). 2013; 32(2):376–384.
Article5. Aitken M, Gauntlett C. Patient apps for improved healthcare: from novelty to mainstream. Parsippany (NJ): IMS Institute for Healthcare Informatics;2013.6. Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med. 2013; 10(1):e1001363.
Article7. World Health Organization. mHealth: new horizons for health through mobile technologies. Geneva, Switzerland: World Health Organization;2011.8. Powell AC, Landman AB, Bates DW. In search of a few good apps. JAMA. 2014; 311(18):1851–1852.
Article9. Park JY, Lee G, Shin SY, Kim JH, Han HW, Kwon TW, et al. Lessons learned from the development of health applications in a tertiary hospital. Telemed J E Health. 2014; 20(3):215–222.
Article10. Terry M. Medical Apps for Smartphones. Telemed J E Health. 2010; 16(1):17–22.
Article11. Case MA, Burwick HA, Volpp KG, Patel MS. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA. 2015; 313(6):625–626.
Article12. Miguez-Burbano MJ, Ergon E. Use of wearable monitoring devices to change health behavior. JAMA. 2015; 313(18):1865.
Article13. Park YR, Lee Y, Lee G, Lee JH, Shin SY. Smartphone applications with sensors used in a tertiary hospitalcurrent status and future challenges. Sensors (Basel). 2015; 15(5):9854–9869.
Article14. Lee J. Smart health: concepts and status of ubiquitous health with smartphone. In : Proceedings of 2011 International Conference on ICT Convergence (ICTC); 2011 Sep 28-30; Seoul, Korea. p. 388–389.15. Muhlestein JB. QTC intervals can be assessed with the AliveCor heart monitor in patients on dofetilide for atrial fibrillation. J Electrocardiol. 2015; 48(1):10–11.
Article16. Ceja E, Osmani V, Mayora O. Automatic stress detection in working environments from smartphones' accelerometer data: a first step. IEEE J Biomed Health Inform. 2015; 06. 16. DOI: 10.1109/JBHI.2015.2446195. [Epub].17. Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ. Feasibility of popular m-health technologies for activity tracking among individuals with serious mental illness. Telemed J E Health. 2015; 21(3):213–216.
Article18. Zvornicanin E, Zvornicanin J, Hadziefendic B. The Use of Smart phones in Ophthalmology. Acta Inform Med. 2014; 22(3):206–209.
Article19. Infantino J. Patient engagement, interoperability needed for mobile health to succeed [Internet]. Oakland (CA): iHealthBeat.com;2014. cited at 2015 Aug 3. Available from: http://www.ihealthbeat.org/insight/2014/patient-engagement-interoperability-needed-for-mobile-health-to-succeed.20. Yuan S, Ma W, Kanthawala S, Peng W. Keep using my health apps: discover users' perception of health and fitness apps with the UTAUT2 model. Telemed J E Health. 2015; 21(9):735–741.
Article21. Bidmon S, Terlutter R, Rottl J. What explains usage of mobile physician-rating apps? Results from a web-based questionnaire. J Med Internet Res. 2014; 16(6):e148.
Article22. Ritter S. Apple's research kit development framework for iPhone apps enables innovative approaches to medical research data collection. J Clin Trials. 2015; 5(2):e120.
Article23. Tomlinson M, Rotheram-Borus MJ, Swartz L, Tsai AC. Scaling up mHealth: where is the evidence? PLoS Med. 2013; 10(2):e1001382.
Article24. Mistry H. Systematic review of studies of the costeffectiveness of telemedicine and telecare: changes in the economic evidence over twenty years. J Telemed Telecare. 2012; 18(1):1–6.
Article25. Jang D, Shin SY, Seo DW, Joo S, Huh SJ. A smartphone-based system for the automated management of pointof-care test results in hospitals. Telemed J E Health. 2015; 21(4):301–305.
Article26. Institute of Medicine, Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academy Press;2001.27. Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006; 144(10):742–752.
Article28. Restuccia JD, Cohen AB, Horwitt JN, Shwartz M. Hospital implementation of health information technology and quality of care: are they related? BMC Med Inform Decis Mak. 2012; 12:109.
Article29. Lee J. The impact of health information technology on disparity of process of care. Int J Equity Health. 2015; 14(1):34.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Qualitative assessment of atopic dermatitis-related mobile applications in Korea
- Quality Evaluation of Online Health Information Related to Young Child
- Development and Evaluation of a Self-management Mobile App for Adults with Osteoarthritis
- Quality evaluation of pregnancy-related mobile applications in South Korea: a descriptive study
- The Perception of Laymen and Experts Toward Mobile Applications for Self-monitoring of Diet Based on in-depth Interviews and Focus Group Interviews