Ann Rehabil Med.
2013 Apr;37(2):229-234. 10.5535/arm.2013.37.2.229.
Clinical Outcomes of Extracorporeal Shock Wave Therapy in Patients With Secondary Lymphedema: A Pilot Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Ewha Womans University School of Medicine, Seoul, Korea. hoyabbun5050@hanmail.net
- KMID: 2165775
- DOI: http://doi.org/10.5535/arm.2013.37.2.229
Abstract
OBJECTIVE
To investigate the clinical effect of extracorporeal shock wave therapy (ESWT) in patients with secondary lymphedema after breast cancer treatment.
METHODS
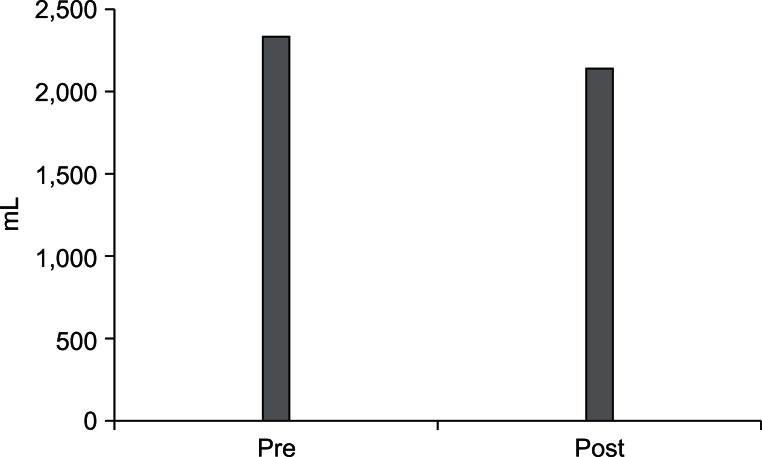
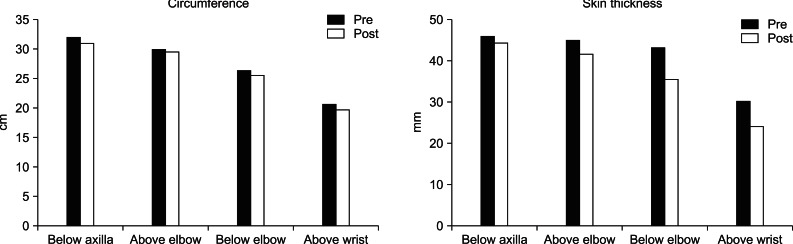
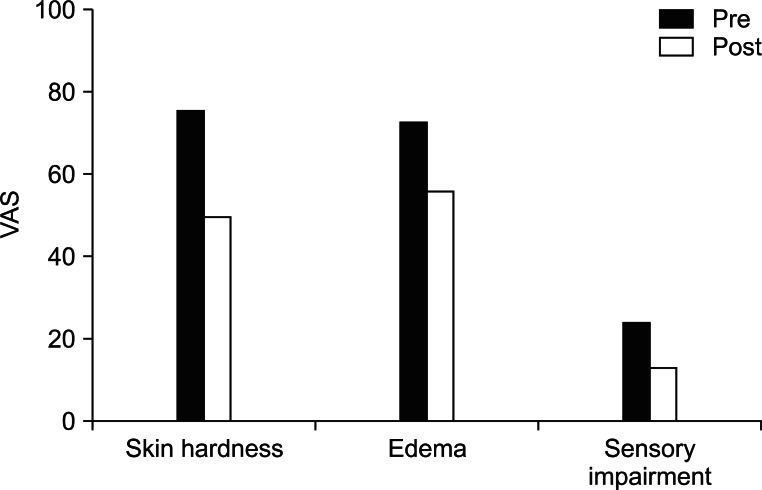
In a prospective clinical trial, ESWT was performed consecutively 4 times over two weeks in 7 patients who were diagnosed with stage 3 secondary lymphedema after breast cancer treatment. Each patient was treated with four sessions of ESWT (0.056-0.068 mJ/mm2, 2,000 impulses). The parameters were the circumference of the arm, thickness of the skin and volume of the arm. We measured these parameters with baseline values before ESWT and repeated the evaluation after each ESWT treatment. Subjective data on skin thickness, edema and sensory impairment were obtained using a visual analogue scale (VAS).
RESULTS
The mean volume of the affected arm after four consecutive ESWT was significantly reduced from 2,332 to 2,144 mL (p<0.05). The circumference and thickness of the skin fold of the affected arm were significantly decreased after the fourth ESWT (p<0.05). The three VAS scores were significantly improved after the fourth ESWT. Almost all patients were satisfied with this treatment and felt softer texture in their affected arm after treatment.
CONCLUSION
ESWT is an effective modality in the treatment of stage 3 lymphedema after breast cancer treatment. ESWT reduced the circumference and the thickness of arms with lymphedema and satisfied almost all patients with lymphedema. Therefore, this treatment provides clinically favorable outcome to patients with breast cancer-related lymphedema.
MeSH Terms
Figure
Cited by 2 articles
-
Computed Tomography as an Objective Measurement Tool for Secondary Lymphedema Treated With Extracorporeal Shock Wave Therapy
So-Yeon Kim, Hasuk Bae, Hye Min Ji
Ann Rehabil Med. 2015;39(3):488-493. doi: 10.5535/arm.2015.39.3.488.Effects of Extracorporeal Shockwave Therapy on Improvements in Lymphedema, Quality of Life, and Fibrous Tissue in Breast Cancer-Related Lymphedema
Kyeong Woo Lee, Sang Beom Kim, Jong Hwa Lee, Young Sam Kim
Ann Rehabil Med. 2020;44(5):386-392. doi: 10.5535/arm.19213.
Reference
-
1. Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema: a comprehensive review. Ann Plast Surg. 2007; 59:464–472. PMID: 17901744.2. Hinrichs CS, Watroba NL, Rezaishiraz H, Giese W, Hurd T, Fassl KA, et al. Lymphedema secondary to postmastectomy radiation: incidence and risk factors. Ann Surg Oncol. 2004; 11:573–580. PMID: 15172932.
Article3. Querci della Rovere G, Ahmad I, Singh P, Ashley S, Daniels IR, Mortimer P. An audit of the incidence of arm lymphoedema after prophylactic level I/II axillary dissection without division of the pectoralis minor muscle. Ann R Coll Surg Engl. 2003; 85:158–161. PMID: 12831486.
Article4. Kim KS, Ko HY. Upper extremity lymphedema secondary to breast cancer. J Korean Acad Rehabil Med. 1992; 16:94–100.5. Casley-Smith JR, Casley-Smith JR. Treatment of lymphedema by complex physical therapy, with and without oral and topical benzopyrones: what should therapists and patients expect. Lymphology. 1996; 29:76–82. PMID: 8823730.6. Williams AF, Vadgama A, Franks PJ, Mortimer PS. A randomized controlled crossover study of manual lymphatic drainage therapy in women with breast cancer-related lymphoedema. Eur J Cancer Care (Engl). 2002; 11:254–261. PMID: 12492462.
Article7. Ko DS, Lerner R, Klose G, Cosimi AB. Effective treatment of lymphedema of the extremities. Arch Surg. 1998; 133:452–458. PMID: 9565129.
Article8. Devoogdt N, Van Kampen M, Geraerts I, Coremans T, Christiaens MR. Different physical treatment modalities for lymphoedema developing after axillary lymph node dissection for breast cancer: a review. Eur J Obstet Gynecol Reprod Biol. 2010; 149:3–9. PMID: 20018422.
Article9. Yamamoto R, Yamamoto T. Effectiveness of the treatment-phase of two-phase complex decongestive physiotherapy for the treatment of extremity lymphedema. Int J Clin Oncol. 2007; 12:463–468. PMID: 18071866.
Article10. Boris M, Weindorf S, Lasinkski S. Persistence of lymphedema reduction after noninvasive complex lymphedema therapy. Oncology (Williston Park). 1997; 11:99–109. PMID: 9115856.11. Casley-Smith JR, Morgan RG, Piller NB. Treatment of lymphedema of the arms and legs with 5,6-benzo-[alpha]-pyrone. N Engl J Med. 1993; 329:1158–1163. PMID: 8377779.
Article12. Korpan MI, Crevenna R, Fialka-Moser V. Lymphedema: a therapeutic approach in the treatment and rehabilitation of cancer patients. Am J Phys Med Rehabil. 2011; 90(5 Suppl 1):S69–S75. PMID: 21765266.13. Schaden W, Thiele R, Kolpl C, Pusch M, Nissan A, Attinger CE, et al. Shock wave therapy for acute and chronic soft tissue wounds: a feasibility study. J Surg Res. 2007; 143:1–12. PMID: 17904157.
Article14. Mariotto S, Cavalieri E, Amelio E, Ciampa AR, de Prati AC, Marlinghaus E, et al. Extracorporeal shock waves: from lithotripsy to anti-inflammatory action by no production. Nitric Oxide. 2005; 12:89–96. PMID: 15740982.
Article15. Tinazzi E, Amelio E, Marangoni E, Guerra C, Puccetti A, Codella OM, et al. Effects of shock wave therapy in the skin of patients with progressive systemic sclerosis: a pilot study. Rheumatol Int. 2011; 31:651–656. PMID: 20066427.
Article16. Serizawa F, Ito K, Matsubara M, Sato A, Shimokawa H, Satomi S. Extracorporeal shock wave therapy induces therapeutic lymphangiogenesis in a rat model of secondary lymphoedema. Eur J Vasc Endovasc Surg. 2011; 42:254–260. PMID: 21454105.
Article17. Didem K, Ufuk YS, Serdar S, Zumre A. The comparison of two different physiotherapy methods in treatment of lymphedema after breast surgery. Breast Cancer Res Treat. 2005; 93:49–54. PMID: 16184458.
Article18. Szuba A, Achalu R, Rockson SG. Decongestive lymphatic therapy for patients with breast carcinoma-associated lymphedema. A randomized, prospective study of a role for adjunctive intermittent pneumatic compression. Cancer. 2002; 95:2260–2267. PMID: 12436430.19. Lee BB, Kim YW, Kim DI, Hwang JH, Laredo J, Neville R. Supplemental surgical treatment to end stage (stage IV-V) of chronic lymphedema. Int Angiol. 2008; 27:389–395. PMID: 18974701.20. Andersen L, Hojris I, Erlandsen M, Andersen J. Treatment of breast-cancer-related lymphedema with or without manual lymphatic drainage: a randomized study. Acta Oncol. 2000; 39:399–405. PMID: 10987238.
Article21. Casley-Smith JR, Boris M, Weindorf S, Lasinski B. Treatment for lymphedema of the arm: the Casley-Smith method. A noninvasive method produces continued reduction. Cancer. 1998; 83(12 Suppl American):2843–2860. PMID: 9874410.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computed Tomography as an Objective Measurement Tool for Secondary Lymphedema Treated With Extracorporeal Shock Wave Therapy
- Feasibility of Extracorporeal Shock Wave Therapy for Complex Upper Limb Morbidity in Breast Cancer Patient
- Treatment of Nonunion of Tibia with Extracorporeal Shock Wave Therapy: A Case Report
- Extracorporeal Shock Wave Therapy for the Treatment of Refractory Plantar Fasciitis
- Effects of Extracorporeal Shock Wave Lithortripsy Experimentally Induced Cholelithiasis and Organs in the Dog