Clin Endosc.
2013 Sep;46(5):436-440.
Tissue Acquisition in Gastric Epithelial Tumor Prior to Endoscopic Resection
- Affiliations
-
- 1Center for Gastric Cancer, National Cancer Center, Goyang, Korea. glse@chol.com
Abstract
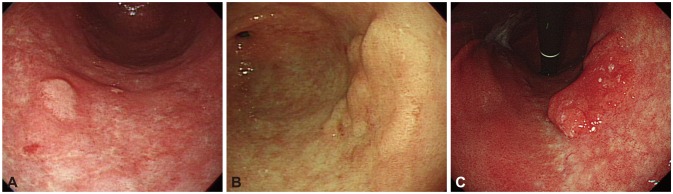
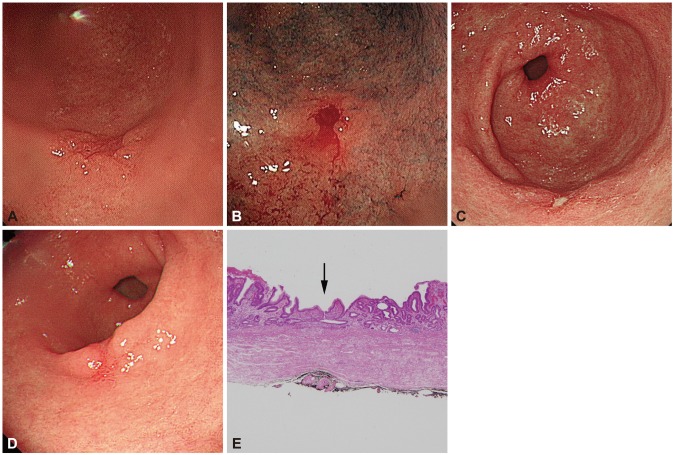
- Endoscopic forceps biopsy is essential before planning an endoscopic resection of upper gastrointestinal epithelial tumors. However, forceps biopsy is limited by its superficiality and frequency of sampling errors. Histologic discrepancies between endoscopic forceps biopsies and resected specimens are frequent. Factors associated with such histologic discrepancies are tumor size, macroscopic type, surface color, and the type of medical facility. Precise targeting of biopsies is recommended to achieve an accurate diagnosis, curative endoscopic resection, and a satisfactory oncologic outcome. Multiple deep forceps biopsies can induce mucosal ulceration in early gastric cancer. Endoscopic resection for early gastric cancer with ulcerative findings is associated with piecemeal resection, incomplete resection, and a risk for procedure-related complications such as bleeding and perforation. Such active ulcers caused by forceps biopsy and following submucosal fibrosis might also be mistaken as an indication for more aggressive procedures, such as gastrectomy with D2 lymph node dissection. Proton pump inhibitors might be prescribed to facilitate the healing of biopsy-induced ulcers if an active ulcer is predicted after deep biopsy. It is unknown which time interval from biopsy to endoscopic resection is appropriate for a safe procedure and a good oncologic outcome. Further investigations are needed to conclude the appropriate time interval.
MeSH Terms
Figure
Reference
-
1. Cho SJ, Choi IJ, Kim CG, et al. Risk of high-grade dysplasia or carcinoma in gastric biopsy-proven low-grade dysplasia: an analysis using the Vienna classification. Endoscopy. 2011; 43:465–471. PMID: 21425043.
Article2. Lee CK, Chung IK, Lee SH, et al. Is endoscopic forceps biopsy enough for a definitive diagnosis of gastric epithelial neoplasia? J Gastroenterol Hepatol. 2010; 25:1507–1513. PMID: 20796147.
Article3. Sung HY, Cheung DY, Cho SH, et al. Polyps in the gastrointestinal tract: discrepancy between endoscopic forceps biopsies and resected specimens. Eur J Gastroenterol Hepatol. 2009; 21:190–195. PMID: 19092673.
Article4. Lee SB, Kang HY, Kim KI, Ahn DH. The diagnostic accuracy of endoscopic biopsy for gastric dysplasia. J Gastric Cancer. 2010; 10:175–181. PMID: 22076183.
Article5. Jung MK, Jeon SW, Park SY, et al. Endoscopic characteristics of gastric adenomas suggesting carcinomatous transformation. Surg Endosc. 2008; 22:2705–2711. PMID: 18401651.
Article6. Nam KW, Song KS, Lee HY, et al. Spectrum of final pathological diagnosis of gastric adenoma after endoscopic resection. World J Gastroenterol. 2011; 17:5177–5183. PMID: 22215942.
Article7. Takao M, Kakushima N, Takizawa K, et al. Discrepancies in histologic diagnoses of early gastric cancer between biopsy and endoscopic mucosal resection specimens. Gastric Cancer. 2012; 15:91–96. PMID: 21814828.
Article8. Kim JH, Kim SH, Park WH, et al. Predictable factors of histologic discrepancy of gastric cancer between the endoscopic forceps biopsy and endoscopic treatment specimen. Korean J Gastroenterol. 2012; 59:354–359. PMID: 22617529.
Article9. Yoon WJ, Lee DH, Jung YJ, et al. Histologic characteristics of gastric polyps in Korea: emphasis on discrepancy between endoscopic forceps biopsy and endoscopic mucosal resection specimen. World J Gastroenterol. 2006; 12:4029–4032. PMID: 16810753.
Article10. Graham DY, Schwartz JT, Cain GD, Gyorkey F. Prospective evaluation of biopsy number in the diagnosis of esophageal and gastric carcinoma. Gastroenterology. 1982; 82:228–231. PMID: 7054024.
Article11. Faigel DO, Eisen GM, Baron TH, et al. Tissue sampling and analysis. Gastrointest Endosc. 2003; 57:811–816. PMID: 12776025.
Article12. Ohnita K, Isomoto H, Yamaguchi N, et al. Factors related to the curability of early gastric cancer with endoscopic submucosal dissection. Surg Endosc. 2009; 23:2713–2719. PMID: 19357917.
Article13. Oka S, Tanaka S, Kaneko I, et al. Endoscopic submucosal dissection for residual/local recurrence of early gastric cancer after endoscopic mucosal resection. Endoscopy. 2006; 38:996–1000. PMID: 17058164.
Article14. Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000; 3:219–225. PMID: 11984739.
Article15. Han KS, Sohn DK, Choi DH, et al. Prolongation of the period between biopsy and EMR can influence the nonlifting sign in endoscopically resectable colorectal cancers. Gastrointest Endosc. 2008; 67:97–102. PMID: 18155430.
Article16. Uno Y, Munakata A. The non-lifting sign of invasive colon cancer. Gastrointest Endosc. 1994; 40:485–489. PMID: 7926542.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Strategy after Incomplete Endoscopic Resection of Early Gastric Cancer
- Successful Endoscopic Resection of Gastric Mucosa-Associated Lymphoid Tissue Lymphoma Unresponsive to Helicobacter pylori Eradication Therapy
- Pathologic Diagnosis of Gastric Epithelial Neoplasia
- Negative Histology after Endoscopic Resection: A Pathologist's Aspect
- Endoscopic Management of Gastric Subepithelial Tumor