J Korean Med Sci.
2012 Dec;27(12):1563-1568. 10.3346/jkms.2012.27.12.1563.
Incidence and Risk Factors of Ventriculoperitoneal Shunt Infections in Children: A Study of 333 Consecutive Shunts in 6 Years
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea. eunchoi@snu.ac.kr
- 2Division of Pediatric Neurosurgery, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2157983
- DOI: http://doi.org/10.3346/jkms.2012.27.12.1563
Abstract
- The major aims of this study were to estimate the infection rate and recognize the risk factor for ventriculoperitoneal (VP) shunt infections in children. To analyze shunt infection rate and identify risk factors, a retrospective cohort analysis of 333 consecutive VP shunt series was performed at Seoul National University Children's Hospital in Korea between January 2005 and February 2011. Overall, 35 shunts (10.5%) were infected, which represented an infection rate of 0.075 infection cases per shunt per year. VP shunt infection occurred at a median of 1 month (range, 6 days to 8 months) after insertion. An independent risk factor for shunt infection was undergoing an operation before the first year of life (relative risk 2.31; 95% confidence interval, 1.19-4.48). The most common causative microorganism was coagulase-negative staphylococci in 16 (45.7%) followed by Staphylococcus aureus in 8 (22.9%). Methicillin resistance rate was 83.3% among coagulase-negative staphylococci and S. aureus. In this study, cerebrospinal fluid shunt infection rate was 10.5%. Infection was frequently caused by methicillin-resistant coagulase-negative staphylococci and S. aureus within two months after shunt surgery. Vancomycin may be considered as the preoperative prophylaxis for shunt surgery in a situation where methicillin resistance rate is very high.
Keyword
MeSH Terms
-
Anti-Bacterial Agents/therapeutic use
Bacterial Infections/drug therapy/*epidemiology/microbiology
Child
Child, Preschool
Cohort Studies
Humans
Hydrocephalus/surgery
Incidence
Infant
Infant, Newborn
Male
Methicillin-Resistant Staphylococcus aureus/isolation & purification
Retrospective Studies
Risk Factors
Staphylococcus/isolation & purification
Surgical Wound Infection/drug therapy/*epidemiology/etiology
Vancomycin/therapeutic use
Ventriculoperitoneal Shunt/*adverse effects
Anti-Bacterial Agents
Vancomycin
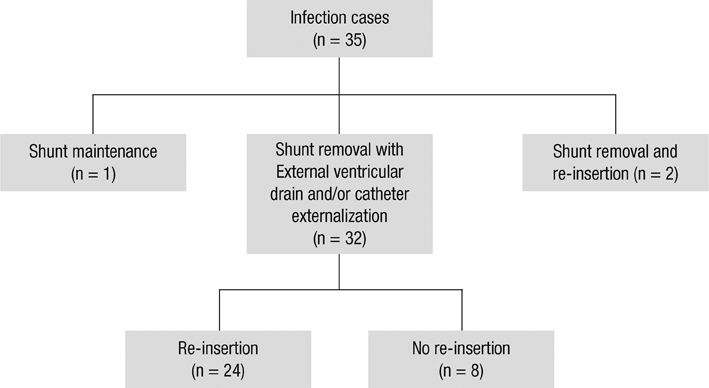
Figure
Reference
-
1. Hirsch JF. Surgery of hydrocephalus: past, present and future. Acta Neurochir (Wien). 1992. 116:155–160.2. Davis SE, Levy ML, McComb JG, Masri-Lavine L. Does age or other factors influence the incidence of ventriculoperitoneal shunt infections? Pediatr Neurosurg. 1999. 30:253–257.3. Dallacasa P, Dappozzo A, Galassi E, Sandri F, Cocchi G, Masi M. Cerebrospinal fluid shunt infections in infants. Childs Nerv Syst. 1995. 11:643–648.4. Odio C, McCracken GH Jr, Nelson JD. CSF shunt infections in pediatrics. A seven-year experience. Am J Dis Child. 1984. 138:1103–1108.5. Kulkarni AV, Drake JM, Lamberti-Pasculli M. Cerebrospinal fluid shunt infection: a prospective study of risk factors. J Neurosurg. 2001. 94:195–201.6. McClinton D, Carraccio C, Englander R. Predictors of ventriculoperitoneal shunt pathology. Pediatr Infect Dis J. 2001. 20:593–597.7. Wang KC, Lee HJ, Sung JN, Cho BK. Cerebrospinal fluid shunt infection in children: efficiency of management protocol, rate of persistent shunt colonization, and significance of 'off-antibiotics' trial. Childs Nerv Syst. 1999. 15:38–43.8. Lee JY, Wang KC, Cho BK. Functioning periods and complications of 246 cerebrospinal fluid shunting procedures in 208 children. J Korean Med Sci. 1995. 10:275–280.9. Rotim K, Miklic P, Paladino J, Melada A, Marcikic M, Scap M. Reducing the incidence of infection in pediatric cerebrospinal fluid shunt operations. Childs Nerv Syst. 1997. 13:584–587.10. Enger PØ, Svendsen F, Sommerfelt K, Wester K. Shunt revisions in children: can they be avoided? Experiences from a population-based study. Pediatr Neurosurg. 2005. 41:300–304.11. Kontny U, Höfling B, Gutjahr P, Voth D, Schwarz M, Schmitt HJ. CSF shunt infections in children. Infection. 1993. 21:89–92.12. McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ. Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis. 2003. 36:858–862.13. Stamos JK, Kaufman BA, Yogev R. Ventriculoperitoneal shunt infections with gram-negative bacteria. Neurosurgery. 1993. 33:858–862.14. Shah SS, Sinkowitz-Cochran RL, Keyserling HL, Jarvis WR. Vancomycin use in pediatric neurosurgery patients. Am J Infect Control. 1999. 27:482–487.15. Tacconelli E, Cataldo MA, Albanese A, Tumbarello M, Arduini E, Spanu T, Fadda G, Anile C, Maira G, Federico G, et al. Vancomycin versus cefazolin prophylaxis for cerebrospinal shunt placement in a hospital with a high prevalence of meticillin-resistant Staphylococcus aureus. J Hosp Infect. 2008. 69:337–344.16. Zafar N, Wallace CM, Kieffer P, Schroeder P, Schootman M, Hamvas A. Improving survival of vulnerable infants increases neonatal intensive care unit nosocomial infection rate. Arch Pediatr Adolesc Med. 2001. 155:1098–1104.17. Tulipan N, Cleves MA. Effect of an intraoperative double-gloving strategy on the incidence of cerebrospinal fluid shunt infection. J Neurosurg. 2006. 104:5–8.18. Kestle JR, Garton HJ, Whitehead WE, Drake JM, Kulkarni AV, Cochrane DD, Muszynski C, Walker ML. Management of shunt infections: a multicenter pilot study. J Neurosurg. 2006. 105:177–181.19. Kulkarni AV, Rabin D, Lamberti-Pasculli M, Drake JM. Repeat cerebrospinal fluid shunt infection in children. Pediatr Neurosurg. 2001. 35:66–71.20. Sciubba DM, Stuart RM, McGirt MJ, Woodworth GF, Samdani A, Carson B, Jallo GI. Effect of antibiotic-impregnated shunt catheters in decreasing the incidence of shunt infection in the treatment of hydrocephalus. J Neurosurg. 2005. 103:131–136.21. Kan P, Kestle J. Lack of efficacy of antibiotic-impregnated shunt systems in preventing shunt infections in children. Childs Nerv Syst. 2007. 23:773–777.22. Ritz R, Roser F, Morgalla M, Dietz K, Tatagiba M, Will BE. Do antibiotic-impregnated shunts in hydrocephalus therapy reduce the risk of infection? An observational study in 258 patients. BMC Infect Dis. 2007. 7:38.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Ventriculoperitoneal Shunt Placement in Hydrocephalus
- Risk factors associated with slit ventricle syndrome after ventriculoperitoneal shunt surgery
- A Retrospective Analysis of Ventriculoperitoneal Shunt Revision Cases of a Single Institute
- Abdominal Cerebrospinal Pseudocyst: a Complication of Ventriculoperitoneal Shunt in a Child
- Pneumothorax during Ventriculoperitoneal Shunt Operation: A case report