J Korean Med Sci.
2010 Jun;25(6):966-969. 10.3346/jkms.2010.25.6.966.
A Case of Hypertrophic Cranial Pachymeningitis Presenting with Scleritis in a Patient with Undifferentiated Connective Tissue Disease
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Holy Family Hospital, Bucheon, Korea.
- 2Department of Anatomical Pathology, College of Medicine, The Catholic University of Korea, Holy Family Hospital, Bucheon, Korea.
- 3Division of Rheumatology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Holy Family Hospital, Bucheon, Korea. rmin6403@yahoo.co.kr
- KMID: 2150882
- DOI: http://doi.org/10.3346/jkms.2010.25.6.966
Abstract
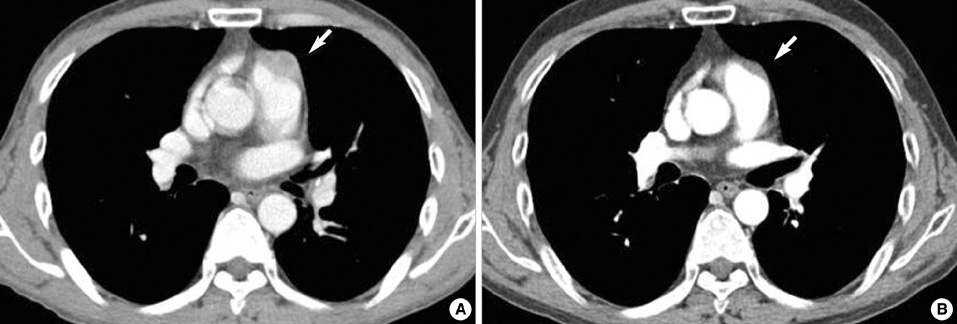
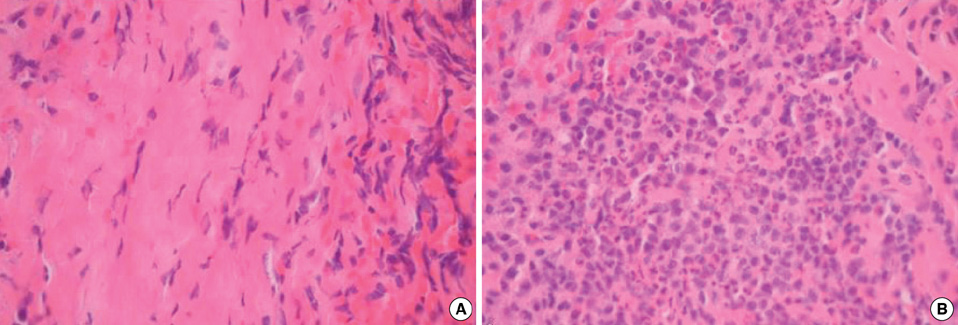
- Hypertrophic cranial pachymeningitis (HCP) is an uncommon disorder that causes a localized or diffuse thickening of the dura mater and has been reported to be infrequently associated with systemic autoimmune disorders such as Wegener's granulomatosis, rheumatoid arthritis, sarcoidosis, Behcet's disease, Sjogren syndrome, and temporal arteritis. Here, we report a case of HCP initially presented with scleritis and headache in a patient with undifferenciated connective tissue disease (UCTD). HCP was initially suspected on brain magnetic resonance imaging and defined pathologically on meningial biopsy. Immunologic studies showed the presence of anti-RNP antibody. After high dose corticosteroid therapy, the patient's symptoms and radiologic abnormalities of brain were improved. Our case suggested that HCP should be considered in the differential diagnosis of headache in a patient with UCTD presenting with scleritis.
Figure
Reference
-
1. Kupersmith MJ, Martin V, Heller G, Shah A, Mitnick HJ. Idiopathic hypertrophic pachymeningitis. Neurology. 2004. 62:686–694.2. Mosca M, Tani C, Bombardieri S. A case of undifferentiated connective tissue disease: is it a distinct clinical entity? Nat Clin Pract Rheumatol. 2008. 4:328–332.3. Smith JR, Mackensen F, Rosenbaum JT. Therapy insight: scleritis and its relationship to systemic autoimmune disease. Nat Clin Pract Rheumatol. 2007. 3:219–226.4. Lampropoulos CE, Zain M, Jan W, Nader-Sepahi A, Sabin IH, D'Cruz DP. Hypertrophic pachymeningitis and undifferentiated connective tissue disease: a case report and review of the literature. Clin Rheumatol. 2006. 25:399–401.5. Ueda S, Hayashi Y, Kono T, Norito M, Hishida E, Shraki K. A case of pachymeningitis with impaired ocular motility. Rinsho Ganka. 2006. 60:553–557.6. Starosta MA, Brandwein SR. Clinical manifestations and treatment of rheumatoid pachymeningitis. Neurology. 2007. 68:1079–1080.7. Pai S, Welsh CT, Patel S, Rumboldt Z. Idiopathic hypertrophic spinal pachymeningitis: report of two cases with typical MR imaging findings. AJNR Am J Neuroradiol. 2007. 28:590–592.8. Mamelak AN, Kelly WM, Davis RL, Rosenblum ML. Idiopathic hypertrophic cranial pachymeningitis. Report of three cases. J Neurosurg. 1993. 79:270–276.9. Im SH, Cho KT, Seo HS, Choi JS. Idiopathic hypertrophic cranial pachymeningitis presenting with headache. Headache. 2008. 48:1232–1235.10. Song JS, Lim MK, Park BH, Park W. Acute pachymeningitis mimicking subdural hematoma in a patient with polyarteritis nodosa. Rheumatol Int. 2005. 25:637–640.11. Hatano N, Behari S, Nagatani T, Kimura M, Ooka K, Saito K, Yoshida J. Idiopathic hypertrophic cranial pachymeningitis: clinicoradiological spectrum and therapeutic options. Neurosurgery. 1999. 45:1336–1344.12. Narla LD, Newman B, Spottswood SS, Narla S, Kolli R. Inflammatory pseudotumor. Radiographics. 2003. 23:719–729.13. Wang ZJ, Reddy GP, Gotway MB, Yeh BM, Hetts SW, Higgins CB. CT and MR imaging of pericardial disease. Radiographics. 2003. 23:S167–S180.14. Nishio S, Morioka T, Togawa A, Yanase T, Nawata H, Fukui M, Hasuo K. Spontaneous resolution of hypertrophic cranial pachymeningitis. Neurosurg Rev. 1995. 18:201–204.15. Choi IS, Park SC, Jung YK, Lee SS. Combined therapy of corticosteroid and azathioprine in hypertrophic cranial pachymeningitis. Eur Neurol. 2000. 44:193–198.16. Bosman T, Simonin C, Launay D, Caron S, Destee A, Defebvre L. Idiopathic hypertrophic cranial pachymeningitis treated by oral methotrexate: a case report and review of literature. Rheumatol Int. 2008. 28:713–718.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Hypertrophic Cranial Pachymeningitis Presenting with Lower Cranial Nerve Palsy Mimicking Meningioma
- Immunoglobulin G4-Related Hypertrophic Pachymeningitis Presenting with Multiple Lower Cranial Nerve Palsies
- Idiopathic Hypertrophic Cranial Pachymeningitis: Case Report
- A Case of Enucleation due to Extensive necrotizing Scleritis after Pterygium Excision in a Rheumatoid Arthritis Patient
- Idiopathic Hypertrophic Pachymeningitis in the Craniocervical Junction