Restor Dent Endod.
2015 May;40(2):104-112. 10.5395/rde.2015.40.2.104.
Effect of intracanal medicaments used in endodontic regeneration procedures on microhardness and chemical structure of dentin
- Affiliations
-
- 1Department of Restorative Dentistry, Division of Dental Biomaterials, Indiana University School of Dentistry, Indianapolis, IN, USA. gyassen@iupui.edu
- 2Department of Biostatistics, Indiana University School of Medicine, Indianapolis, IN, USA.
- KMID: 2148859
- DOI: http://doi.org/10.5395/rde.2015.40.2.104
Abstract
OBJECTIVES
This study was performed to investigate the effects of different intracanal medicaments on chemical structure and microhardness of dentin.
MATERIALS AND METHODS
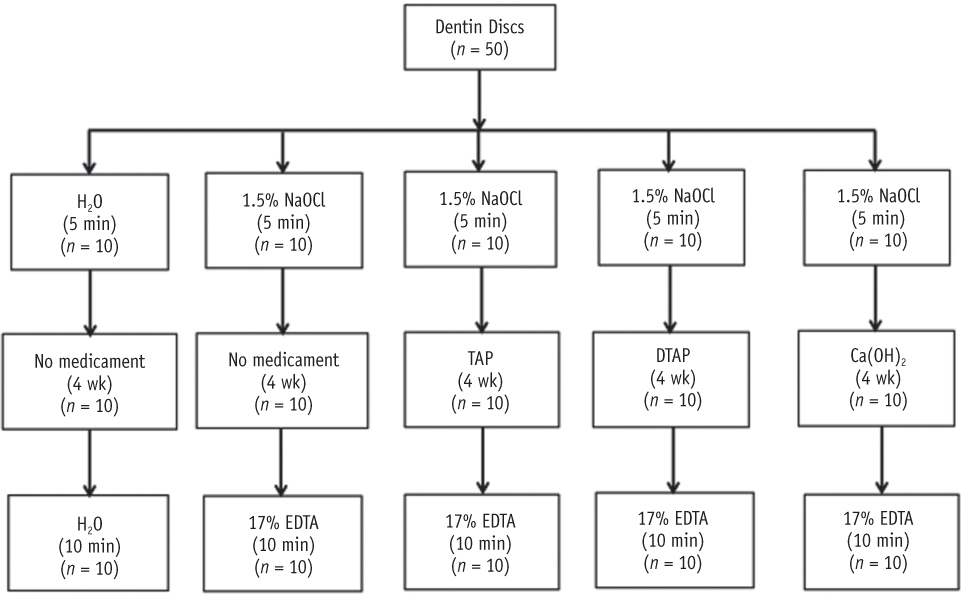
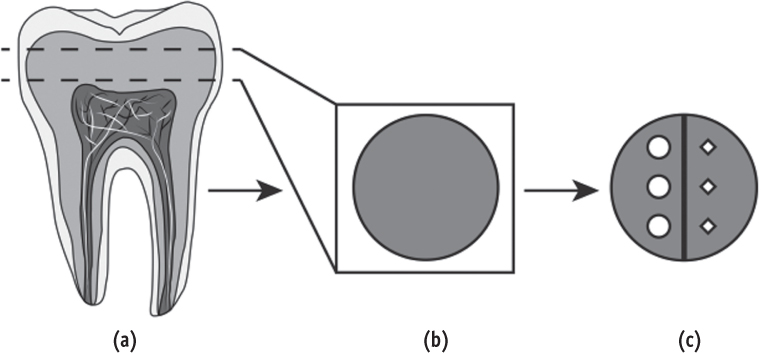
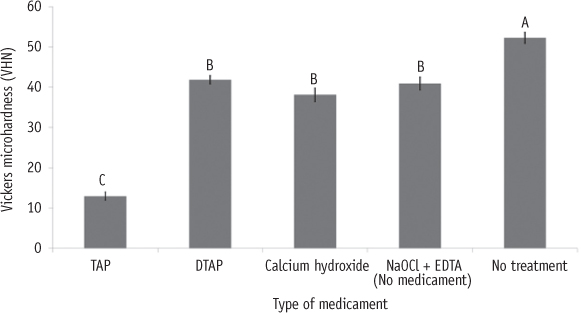
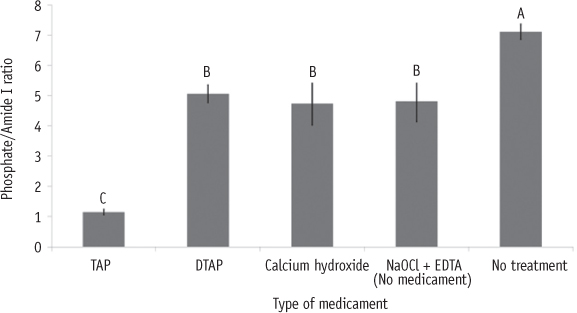
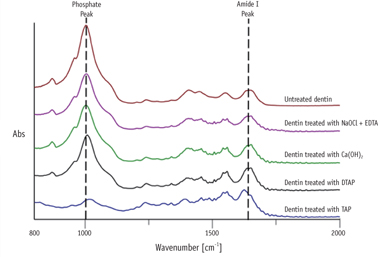
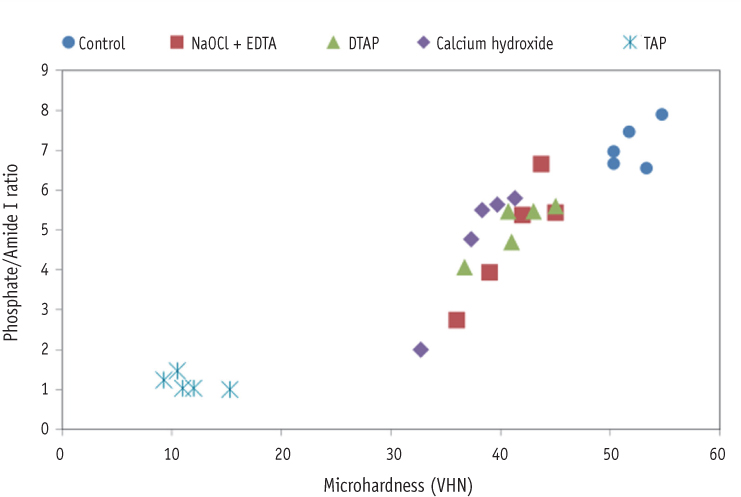
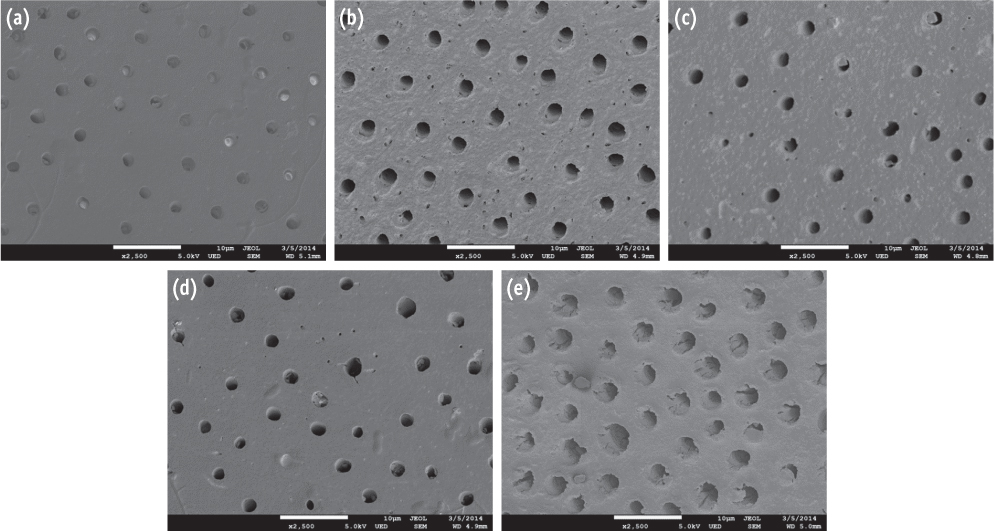
Fifty human dentin discs were obtained from intact third molars and randomly assigned into two control groups and three treatment groups. The first control group received no treatment. The second control group (no medicament group) was irrigated with sodium hypochlorite (NaOCl), stored in humid environment for four weeks and then irrigated with ethylenediaminetetraacetic acid (EDTA). The three treatment groups were irrigated with NaOCl, treated for four weeks with either 1 g/mL triple antibiotic paste (TAP), 1 mg/mL methylcellulose-based triple antibiotic paste (DTAP), or calcium hydroxide [Ca(OH)2] and finally irrigated with EDTA. After treatment, one half of each dentin disc was subjected to Vickers microhardness (n = 10 per group) and the other half was used to evaluate the chemical structure (phosphate/amide I ratio) of treated dentin utilizing attenuated total reflection Fourier transform infrared spectroscopy (n = 5 per group). One-way ANOVA followed by Fisher's least significant difference were used for statistical analyses.
RESULTS
Dentin discs treated with different intracanal medicaments and those treated with NaOCl + EDTA showed significant reduction in microhardness (p < 0.0001) and phosphate/amide I ratio (p < 0.05) compared to no treatment control dentin. Furthermore, dentin discs treated with TAP had significantly lower microhardness (p < 0.0001) and phosphate/amide I ratio (p < 0.0001) compared to all other groups.
CONCLUSIONS
The use of DTAP or Ca(OH)2 medicaments during endodontic regeneration may cause significantly less microhardness reduction and superficial demineralization of dentin compared to the use of TAP.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Triple antibiotic paste: momentous roles and applications in endodontics: a review
Ardavan Parhizkar, Hanieh Nojehdehian, Saeed Asgary
Restor Dent Endod. 2018;43(3):. doi: 10.5395/rde.2018.43.e28.Retention of BioAggregate and MTA as coronal plugs after intracanal medication for regenerative endodontic procedures: an ex vivo study
Suzan Abdul Wanees Amin, Shaimaa Ismail Gawdat
Restor Dent Endod. 2018;43(3):. doi: 10.5395/rde.2018.43.e18.Effect of hydrogel-based antibiotic intracanal medicaments on crown discoloration
Rayan B. Yaghmoor, Jeffrey A. Platt, Kenneth J. Spolnik, Tien Min Gabriel Chu, Ghaeth H. Yassen
Restor Dent Endod. 2021;46(4):e52. doi: 10.5395/rde.2021.46.e52.
Reference
-
1. Yassen GH, Chin J, Mohammedsharif AG, Alsoufy SS, Othman SS, Eckert G. The effect of frequency of calcium hydroxide dressing change and various pre- and inter-operative factors on the endodontic treatment of traumatized immature permanent incisors. Dent Traumatol. 2012; 28:296–301.
Article2. El-Meligy OA, Avery DR. Comparison of apexification with mineral trioxide aggregate and calcium hydroxide. Pediatr Dent. 2006; 28:248–253.3. Trope M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent Clin North Am. 2010; 54:313–324.
Article4. Andreasen JO, Munksgaard EC, Bakland LK. Comparison of fracture resistance in root canals of immature sheep teeth after filling with calcium hydroxide or MTA. Dent Traumatol. 2006; 22:154–156.
Article5. Yassen GH, Platt JA. The effect of nonsetting calcium hydroxide on root fracture and mechanical properties of radicular dentine: a systematic review. Int Endod J. 2013; 46:112–118.
Article6. Diogenes A, Henry MA, Teixeira FB, Hargreaves KM. An update on clinical regenerative endodontics. Endod Top. 2013; 28:2–23.
Article7. Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod. 2012; 38:1330–1336.
Article8. Nosrat A, Homayounfar N, Oloomi K. Drawbacks and unfavorable outcomes of regenerative endodontic treatments of necrotic immature teeth: a literature review and report of a case. J Endod. 2012; 38:1428–1434.
Article9. Nosrat A, Li KL, Vir K, Hicks ML, Fouad AF. Is pulp regeneration necessary for root maturation? J Endod. 2013; 39:1291–1295.
Article10. American Association of Endodontists: Considerations for Regenerative Procedures. updated 2014 Aug 12. Available from: http://www.aae.org/clinical-resources/regenerative-endodontics/considerations-for-regenerative-procedures.aspx.11. Galler KM, D'Souza RN, Federlin M, Cavender AC, Hartgerink JD, Hecker S, Schmalz G. Dentin conditioning codetermines cell fate in regenerative endodontics. J Endod. 2011; 37:1536–1541.
Article12. Schmalz G, Smith AJ. Pulp development, repair, and regeneration: challenges of the transition from traditional dentistry to biologically based therapies. J Endod. 2014; 40:Supplement 4. S2–S5.
Article13. Lovelace TW, Henry MA, Hargreaves KM, Diogenes A. Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedure. J Endod. 2011; 37:133–138.
Article14. Zhang K, Kim YK, Cadenaro M, Bryan TE, Sidow SJ, Loushine RJ, Ling JQ, Pashley DH, Tay FR. Effects of different exposure times and concentrations of sodium hypochlorite/ethylenediaminetetraacetic acid on the structural integrity of mineralized dentin. J Endod. 2010; 36:105–109.
Article15. Grigoratos D, Knowles J, Ng YL, Gulabivala K. Effect of exposing dentine to sodium hypochlorite and calcium hydroxide on its flexural strength and elastic modulus. Int Endod J. 2001; 34:113–119.
Article16. Eldeniz AU, Erdemir A, Belli S. Effect of EDTA and citric acid solutions on the microhardness and the roughness of human root canal dentin. J Endod. 2005; 31:107–110.
Article17. De-Deus G, Paciornik S, Mauricio MH. Evaluation of the effect of EDTA, EDTAC and citric acid on the microhardness of root dentine. Int Endod J. 2006; 39:401–407.
Article18. Yassen GH, Vail MM, Chu TG, Platt JA. The effect of medicaments used in endodontic regeneration on root fracture and microhardness of radicular dentine. Int Endod J. 2013; 46:688–695.
Article19. Hu X, Peng Y, Sum CP, Ling J. Effects of concentrations and exposure times of sodium hypochlorite on dentin deproteination: attenuated total reflection Fourier transform infrared spectroscopy study. J Endod. 2010; 36:2008–2011.
Article20. Zhang K, Tay FR, Kim YK, Mitchell JK, Kim JR, Carrilho M, Pashley DH, Ling JQ. The effect of initial irrigation with two different sodium hypochlorite concentrations on the erosion of instrumented radicular dentin. Dent Mater. 2010; 26:514–523.
Article21. Yassen GH, Chu TM, Eckert G, Platt JA. Effect of medicaments used in endodontic regeneration technique on the chemical structure of human immature radicular dentin: an in vitro study. J Endod. 2013; 39:269–273.
Article22. Ruparel NB, Teixeira FB, Ferraz CC, Diogenes A. Direct effect of intracanal medicaments on survival of stem cells of the apical papilla. J Endod. 2012; 38:1372–1375.
Article23. Geisler TM. Clinical considerations for regenerative endodontic procedures. Dent Clin North Am. 2012; 56:603–626.
Article24. Ari H, Erdemir A, Belli S. Evaluation of the effect of endodontic irrigation solutions on the microhardness and the roughness of root canal dentin. J Endod. 2004; 30:792–795.
Article25. Kinney JH, Marshall SJ, Marshall GW. The mechanical properties of human dentin: a critical review and reevaluation of the dental literature. Crit Rev Oral Biol Med. 2003; 14:13–29.
Article26. Althumairy RI, Teixeira FB, Diogenes A. Effect of dentin conditioning with intracanal medicaments on survival of stem cells of apical papilla. J Endod. 2014; 40:521–525.
Article27. Sabrah AH, Yassen GH, Gregory RL. Effectiveness of antibiotic medicaments against biofilm formation of Enterococcus faecalis and Porphyromonas gingivalis. J Endod. 2013; 39:1385–1389.
Article28. Minabe M, Takeuchi K, Kumada H, Umemoto T. The effect of root conditioning with minocycline HCl in removing endotoxin from the roots of periodontallyinvolved teeth. J Periodontol. 1994; 65:387–392.
Article29. Featherstone JD, ten Cate JM, Shariati M, Arends J. Comparison of artificial caries-like lesions by quantitative microradiography and microhardness profiles. Caries Res. 1983; 17:385–391.
Article30. Ozdemir HO, Buzoglu HD, Calt S, Cehreli ZC, Varol E, Temel A. Chemical and ultramorphologic effects of ethylenediaminetetraacetic acid and sodium hypochlorite in young and old root canal dentin. J Endod. 2012; 38:204–208.
Article31. Zehnder M. Root canal irrigants. J Endod. 2006; 32:389–398.
Article32. Caiado AC, de Goes MF, de Souza-Filho FJ, Rueggeberg FA. The effect of acid etchant type and dentin location on tubular density and dimension. J Prosthet Dent. 2010; 103:352–361.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Intracanal Medicaments on Push-out Bond Strength of Calcium Silicate-based Materials
- A review of the regenerative endodontic treatment procedure
- Influence of microhardness and fluoride content of tooth structure by fluoride-containing restorative materials
- Endodontic biofilms: contemporary and future treatment options
- Antimicrobial effect of calcium hydroxide as an intracanal medicament in root canal treatment: a literature review - Part I. In vitro studies