Ann Rehabil Med.
2015 Aug;39(4):517-523. 10.5535/arm.2015.39.4.517.
The Effects of the VFSS Timing After Nasogastric Tube Removal on Swallowing Function of the Patients With Dysphagia
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Kwangju Christian Hospital, Gwangju, Korea. starhoon3@hanmail.net
- KMID: 2148221
- DOI: http://doi.org/10.5535/arm.2015.39.4.517
Abstract
OBJECTIVE
To evaluate the effects of the videofluoroscopic swallowing study (VFSS) timing after the nasogastric tube (NGT) removal on swallowing function of the patients with dysphagia.
METHODS
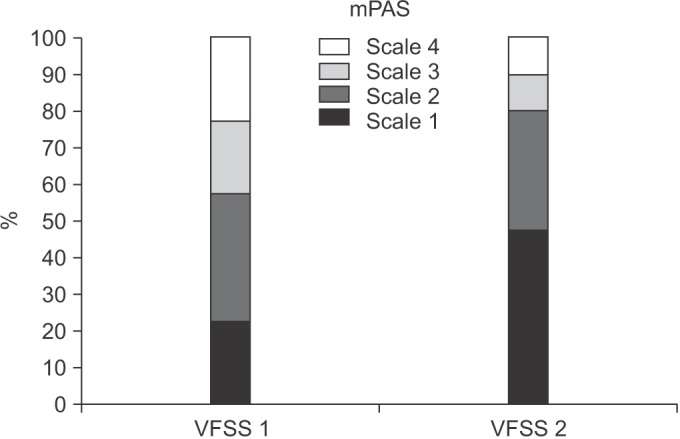
This study was conducted on 40 NGT-fed patients with dysphagia. To assess the patients' swallowing function, VFSS was performed twice using a 5-mL 35% diluted barium solution. For the initial examination, VFSS was performed immediately after the NGT removal (VFSS 1). For the second examination, VFSS was performed five hours after the NGT removal (VFSS 2). We used the functional dysphagia scale (FDS) to assess swallowing function. In the FDS, a significant difference in the four items in the oral phase, seven items in the pharyngeal phase, and total scores were assessed (p<0.05). We also used modified penetration-aspiration scale (mPAS) to compare the two examinations (p<0.05).
RESULTS
A paired t-test was performed to confirm the statistical significance of the two examinations (p<0.05). The overall swallowing function was assessed as better in VFSS 2 than in VFSS 1. In the FDS, significant differences in the residue in valleculae (p=0.002), the residue in pyriform sinuses (p=0.001), the coating of pharyngeal wall after swallow (p=0.001), and the total scores (p<0.001) were found between the two examinations. Also, in the mPAS that assessed the degree of penetration-aspiration, a significant difference was found between the two examinations (p<0.001).
CONCLUSION
The results of this study confirmed that the timing of the VFSS after the NGT removal affects the swallowing function. Thus, to accurately assess the swallowing function, VFSS must be performed in NGT-fed patients after they have rested for a certain period following the removal of their NGT.
Keyword
Figure
Reference
-
1. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter. Stroke. 1996; 27:1200–1204.2. Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW. Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil. 1995; 76:310–316. PMID: 7717830.
Article3. Palmer JB, Pelletier CA, Matsuo K. Rehabilitation of patients with swallowing disorders. In : Braddom RL, editor. Physical medicine and rehabilitation. 4th ed. Philadelphia: Saunders;2011. p. 581–597.4. Jung SH, Lee KJ, Hong JB, Han TR. Validation of clinical dysphagia scale: based on videofluoroscopic swallowing study. J Korean Acad Rehabil Med. 2005; 29:343–350.5. Eyal H. Evaluation and treatment of swallowing disorders (dysphagia): the American model as an opportunity for improving patient care and cost containment in Israel's healthcare system. Harefuah. 1997; 132:775–778.6. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article7. American Speech-Language-Hearing Association. National Outcomes Measurement System. Adult speech language pathology training manual. Rockville: American Speech-Language-Hearing Association;1998.8. Paik NJ, Kim IS, Kim JH, Oh BM, Han TR. Clinical validity of the functional dysphagia scale based on videofluoroscopic swallowing study. J Korean Acad Rehabil Med. 2005; 29:43–49.9. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article10. Kim JY, Koh ES, Kim HR, Chun SM, Lee SU, Jung SH. The diagnostic usefulness of the fiberoptic endoscopic evaluation of swallowing. J Korean Acad Rehabil Med. 2011; 35:14–22.11. Wang TG, Wu MC, Chang YC, Hsiao TY, Lien IN. The effect of nasogastric tubes on swallowing function in persons with dysphagia following stroke. Arch Phys Med Rehabil. 2006; 87:1270–1273. PMID: 16935066.
Article12. Cook IJ, Dodds WJ, Dantas RO, Kern MK, Massey BT, Shaker R, et al. Timing of videofluoroscopic, manometric events, and bolus transit during the oral and pharyngeal phases of swallowing. Dysphagia. 1989; 4:8–15.
Article13. Perlman AL, Palmer PM, McCulloch TM, Vandaele DJ. Electromyographic activity from human laryngeal, pharyngeal, and submental muscles during swallowing. J Appl Physiol. 1999; 86:1663–1669. PMID: 10233133.14. Gomes CA Jr, Lustosa SA, Matos D, Andriolo RB, Waisberg DR, Waisberg J. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst Rev. 2012; 3:CD008096. PMID: 22419328.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Nasogastric Tube on Swallowing Function in Stroke Patients with Dysphagia
- The Influence of Nasogastric Tubes on Swallowing Function in Stroke Patient with Dysphagia
- The Relationship between Degree of Dysphagia and the Timing and Frequency of Videofluoroscopic Swallowing Studies in Patients with Acute Stroke
- Self-Knotting of Nasogastric Tube in a Stroke Patient with Dysphagia: A Case Report
- Gastroesophageal Reflux during Nasogastric Tube Feeding versus Oroesophageal Tube Feeding in Stroke Patients: A 24 Hour Esophageal pH-monitoring