Ann Rehabil Med.
2015 Oct;39(5):778-785. 10.5535/arm.2015.39.5.778.
Improved Dysphagia After Decannulation of Tracheostomy in Patients With Brain Injuries
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea. saintc@naver.com
- KMID: 2148209
- DOI: http://doi.org/10.5535/arm.2015.39.5.778
Abstract
OBJECTIVE
To investigate improved dysphagia after the decannulation of a tracheostomy in patients with brain injuries.
METHODS
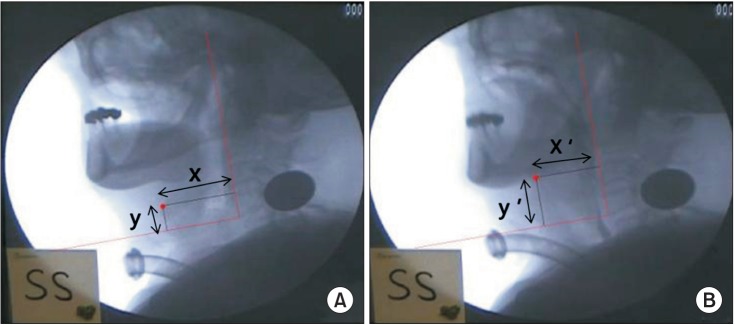
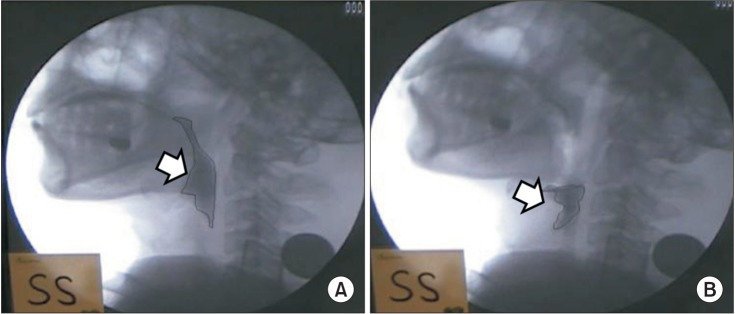
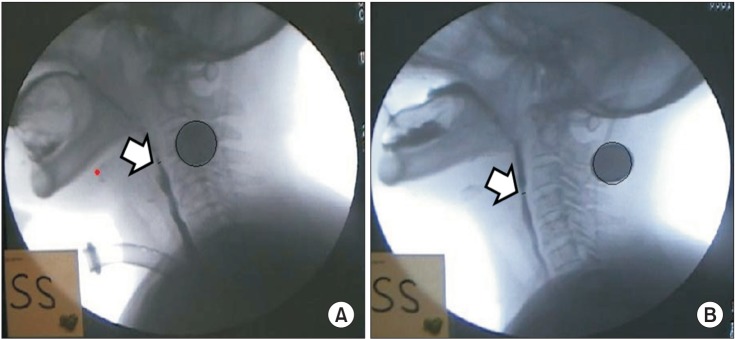
The subjects of this study are patients with brain injuries who were admitted to the Department of Rehabilitation Medicine in Myongji Hospital and who underwent a decannulation between 2012 and 2014. A video fluoroscopic swallowing study (VFSS) was performed in order to investigate whether the patients' dysphagia had improved. We measured the following 5 parameters: laryngeal elevation, pharyngeal transit time, post-swallow pharyngeal remnant, upper esophageal width, and semisolid aspiration. We analyzed the patients' results from VFSS performed one month before and one month after decannulation. All VFSS images were recorded using a camcorder running at 30 frames per second. An AutoCAD 2D screen was used to measure laryngeal elevation, post-swallow pharyngeal remnant, and upper esophageal width.
RESULTS
In this study, a number of dysphagia symptoms improved after decannulation. Laryngeal elevation, pharyngeal transit time, and semisolid aspiration showed no statistically significant differences (p>0.05), however after decannulation, the post-swallow pharyngeal remnant (pre 37.41%+/-24.80%, post 21.02%+/-11.75%; p<0.001) and upper esophageal width (pre 3.57+/-1.93 mm, post 4.53+/-2.05 mm; p<0.001) showed statistically significant differences.
CONCLUSION
When decannulation is performed on patients with brain injuries who do not require a ventilator and who are able to independently excrete sputum, improved esophageal dysphagia can be expected.
MeSH Terms
Figure
Cited by 2 articles
-
Effect of Vallecular Ballooning in Stroke Patients With Dysphagia
Yong Kyun Kim, Sang-heon Lee, Jang-won Lee
Ann Rehabil Med. 2017;41(2):231-238. doi: 10.5535/arm.2017.41.2.231.Effects of Capping of the Tracheostomy Tube in Stroke Patients With Dysphagia
Yong kyun Kim, Sang-heon Lee, Jang-won Lee
Ann Rehabil Med. 2017;41(3):426-433. doi: 10.5535/arm.2017.41.3.426.
Reference
-
1. Stelfox HT, Crimi C, Berra L, Noto A, Schmidt U, Bigatello LM, et al. Determinants of tracheostomy decannulation: an international survey. Crit Care. 2008; 12:R26. PMID: 18302759.
Article2. Frutos-Vivar F, Esteban A, Apezteguia C, Anzueto A, Nightingale P, Gonzalez M, et al. Outcome of mechanically ventilated patients who require a tracheostomy. Crit Care Med. 2005; 33:290–298. PMID: 15699830.
Article3. Kollef MH, Ahrens TS, Shannon W. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 1999; 27:1714–1720. PMID: 10507588.
Article4. Fischler L, Erhart S, Kleger GR, Frutiger A. Prevalence of tracheostomy in ICU patients. A nation-wide survey in Switzerland. Intensive Care Med. 2000; 26:1428–1433. PMID: 11126252.
Article5. Bosel J. Tracheostomy in stroke patients. Curr Treat Options Neurol. 2014; 16:274. PMID: 24357462.
Article6. Goldenberg D, Ari EG, Golz A, Danino J, Netzer A, Joachims HZ. Tracheotomy complications: a retrospective study of 1130 cases. Otolaryngol Head Neck Surg. 2000; 123:495–500. PMID: 11020193.
Article7. Epstein SK. Late complications of tracheostomy. Respir Care. 2005; 50:542–549. PMID: 15807919.8. Norwood S, Vallina VL, Short K, Saigusa M, Fernandez LG, McLarty JW. Incidence of tracheal stenosis and other late complications after percutaneous tracheostomy. Ann Surg. 2000; 232:233–241. PMID: 10903603.
Article9. Ceriana P, Carlucci A, Schreiber A, Fracchia C, Cazzani C, Dichiarante M, et al. Changes of swallowing function after tracheostomy: a videofluoroscopy study. Minerva Anestesiol. 2015; 81:389–397. PMID: 25220547.10. Braddom RL. Physical medicine and rehabilitation. 4th ed. Philadelphia: Saunders;2011. p. 579–597.11. Garuti G, Reverberi C, Briganti A, Massobrio M, Lombardi F, Lusuardi M. Swallowing disorders in tracheostomised patients: a multidisciplinary/multiprofessional approach in decannulation protocols. Multidiscip Respir Med. 2014; 9:36. PMID: 25006457.
Article12. Wise SP, Murray EA, Gerfen CR. The frontal cortexbasal ganglia system in primates. Crit Rev Neurobiol. 1996; 10:317–356. PMID: 8978985.
Article13. Nam HS, Beom J, Oh BM, Han TR. Kinematic effects of hyolaryngeal electrical stimulation therapy on hyoid excursion and laryngeal elevation. Dysphagia. 2013; 28:548–556. PMID: 23605128.
Article14. Kim JC, Kim JS, Jung JH, Kim YK. The effect of balloon dilatation through video-fluoroscopic swallowing study (VFSS) in stroke patients with cricopharyngeal dysfunction. J Korean Acad Rehabil Med. 2011; 35:23–26.15. Wada S, Tohara H, Iida T, Inoue M, Sato M, Ueda K. Jaw-opening exercise for insufficient opening of upper esophageal sphincter. Arch Phys Med Rehabil. 2012; 93:1995–1999. PMID: 22579648.
Article16. Kang JY, Choi KH, Yun GJ, Kim MY, Ryu JS. Does removal of tracheostomy affect dysphagia? A kinematic analysis. Dysphagia. 2012; 27:498–503. PMID: 22327860.
Article17. Drulia TC, Ludlow CL. Relative efficacy of swallowing versus non-swallowing tasks in dysphagia rehabilitation: current evidence and future directions. Curr Phys Med Rehabil Rep. 2013; 1:242–256. PMID: 24470988.
Article18. Gross RD, Mahlmann J, Grayhack JP. Physiologic effects of open and closed tracheostomy tubes on the pharyngeal swallow. Ann Otol Rhinol Laryngol. 2003; 112:143–152. PMID: 12597287.
Article19. Gross RD, Steinhauer KM, Zajac DJ, Weissler MC. Direct measurement of subglottic air pressure while swallowing. Laryngoscope. 2006; 116:753–761. PMID: 16652083.
Article20. Gross RD, Mahlmann J, Grayhack JP. Physiologic effects of open and closed tracheostomy tubes on the pharyngeal swallow. Ann Otol Rhinol Laryngol. 2003; 112:143–152. PMID: 12597287.
Article21. Eibling DE, Gross RD. Subglottic air pressure: a key component of swallowing efficiency. Ann Otol Rhinol Laryngol. 1996; 105:253–258. PMID: 8604883.
Article22. Terk AR, Leder SB, Burrell MI. Hyoid bone and laryngeal movement dependent upon presence of a tracheotomy tube. Dysphagia. 2007; 22:89–93. PMID: 17287926.
Article23. Feldman SA, Deal CW, Urquhart W. Disturbance of swallowing after tracheostomy. Lancet. 1966; 1:954–955. PMID: 4160518.
Article24. Donzelli J, Brady S, Wesling M, Theisen M. Effects of the removal of the tracheotomy tube on swallowing during the fiberoptic endoscopic exam of the swallow (FEES). Dysphagia. 2005; 20:283–289. PMID: 16633873.
Article25. Leder SB, Ross DA. Confirmation of no causal relationship between tracheotomy and aspiration status: a direct replication study. Dysphagia. 2010; 25:35–39. PMID: 19653040.
Article26. Adams V, Mathisen B, Baines S, Lazarus C, Callister R. Reliability of measurements of tongue and hand strength and endurance using the Iowa Oral Performance Instrument with elderly adults. Disabil Rehabil. 2015; 37:389–395. PMID: 24854105.
Article27. Ertekin C, Aydogdu I. Electromyography of human cricopharyngeal muscle of the upper esophageal sphincter. Muscle Nerve. 2002; 26:729–739. PMID: 12451598.
Article28. Cook IJ, Dodds WJ, Dantas RO, Massey B, Kern MK, Lang IM, et al. Opening mechanisms of the human upper esophageal sphincter. Am J Physiol. 1989; 257(5 Pt 1):G748–G759. PMID: 2596608.
Article29. Kuhn MA, Belafsky PC. Management of cricopharyngeus muscle dysfunction. Otolaryngol Clin North Am. 2013; 46:1087–1099. PMID: 24262961.
Article30. Rehman HU, Knox J. There is a need for a regular review of swallowing ability in patients after PEG insertion to identify patients with delayed recovery of swallowing. Dysphagia. 2000; 15:48. PMID: 10594259.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dysphagia and Decannulation Following Tracheostomy in Children
- The Effects of Tracheostomy for the Functional Outcomes of Severe Traumatic Brain Injury Patients
- Extremely Severe Dysphagia Secondary to Tracheostomy: A Case Report
- Effect of Passy-Muir Speaking Valve in Brain-injured Patients with Dysphagia: Two cases report
- Factors Affecting Wound Healing after Decannulation of Tracheostomy Tube