J Korean Med Sci.
2014 Oct;29(10):1372-1378. 10.3346/jkms.2014.29.10.1372.
The Effect of Probiotics for Preventing Radiation-Induced Morphological Changes in Intestinal Mucosa of Rats
- Affiliations
-
- 1Department of Radiation Oncology, Medical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. rokwt@hanmail.net
- 2Department of Radiation Oncology, Inje University College of Medicine, Busan, Korea.
- 3Department of Radiation Oncology, Dong-A University School of Medicine, Busan, Korea.
- KMID: 2129627
- DOI: http://doi.org/10.3346/jkms.2014.29.10.1372
Abstract
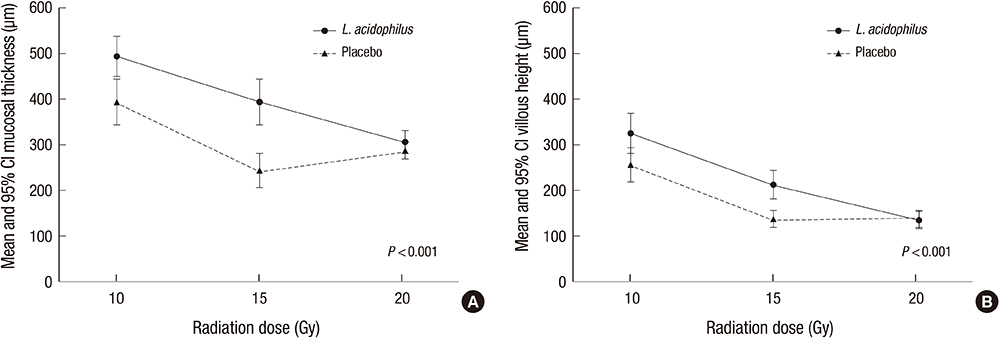
- Radiation therapy is an important treatment modality for abdominal or pelvic cancer, but there is a common and serious complication such as radiation-induced enteritis. Probiotics is reported to have positive effects against radiation-induced enteropathy. In this study, morphological changes of bowel mucosa were analyzed in rats to presume the effect of probiotics on radiation-induced enteritis and its correlation with radiation dose. A total of 48 adult male Sprague-Dawley rats were randomly assigned to two groups and received a solution containing 1.0x108 colony-forming units of Lactiobacillus acidophilus or water once daily for 10 days. Each of two groups was divided into three subgroups and abdomino-pelvic area of each subgroup was irradiated with 10, 15, and 20 Gy, respectively on the seventh day of feeding the solutions. All rats were sacrificed 3 days after irradiation and the mucosal thickness and villus height of jejunum, ileum and colon were measured. The morphological parameters of the small intestine represented significant differences between two solution groups irradiated 10 or 15 Gy, except for villus height of jejunum in 15 Gy-subgroup (P=0.065). There was no significant morphometric difference between two groups irradiated with 20 Gy of radiation. Probiotics appear to be effective for the morphological shortening of small intestinal mucosa damaged by radiation less than or equal to 15 Gy.
Keyword
MeSH Terms
-
Animals
Colon/pathology
Disease Models, Animal
Enteritis/pathology/prevention & control
Ileum/pathology
Intestinal Mucosa/microbiology/*radiation effects
Intestine, Small
Jejunum/pathology
Lactobacillus acidophilus/*metabolism
Male
Probiotics/administration & dosage/*pharmacology
Radiation Injuries, Experimental/*prevention & control/therapy
Radiation Protection/*methods
Random Allocation
Rats
Rats, Sprague-Dawley
Figure
Reference
-
1. Andreyev HJ, Vlavianos P, Blake P, Dearnaley D, Norman AR, Tait D. Gastrointestinal symptoms after pelvic radiotherapy: role for the gastroenterologist? Int J Radiat Oncol Biol Phys. 2005; 62:1464–1471.2. Abayomi J, Kirwan J, Hackett A. The prevalence of chronic radiation enteritis following radiotherapy for cervical or endometrial cancer and its impact on quality of life. Eur J Oncol Nurs. 2009; 13:262–267.3. Kim TG, Huh SJ, Park W. Endoscopic findings of rectal mucosal damage after pelvic radiotherapy for cervical carcinoma: correlation of rectal mucosal damage with radiation dose and clinical symptoms. Radiat Oncol J. 2013; 31:81–87.4. McGough C, Baldwin C, Frost G, Andreyev HJ. Role of nutritional intervention in patients treated with radiotherapy for pelvic malignancy. Br J Cancer. 2004; 90:2278–2287.5. Andreyev J. Gastrointestinal complications of pelvic radiotherapy: are they of any importance? Gut. 2005; 54:1051–1054.6. Guerrero Urbano MT, Henrys AJ, Adams EJ, Norman AR, Bedford JL, Harrington KJ, Nutting CM, Dearnaley DP, Tait DM. Intensity-modulated radiotherapy in patients with locally advanced rectal cancer reduces volume of bowel treated to high dose levels. Int J Radiat Oncol Biol Phys. 2006; 65:907–916.7. Delia P, Sansotta G, Donato V, Frosina P, Messina G, De Renzis C, Famularo G. Use of probiotics for prevention of radiation-induced diarrhea. World J Gastroenterol. 2007; 13:912–915.8. Demirer S, Aydintug S, Aslim B, Kepenekci I, Sengül N, Evirgen O, Gerceker D, Andrieu MN, Ulusoy C, Karahüseyinoglu S. Effects of probiotics on radiation-induced intestinal injury in rats. Nutrition. 2006; 22:179–186.9. Seal M, Naito Y, Barreto R, Lorenzetti A, Safran P, Marotta F. Experimental radiotherapy-induced enteritis: a probiotic interventional study. J Dig Dis. 2007; 8:143–147.10. Chitapanarux I, Chitapanarux T, Traisathit P, Kudumpee S, Tharavichitkul E, Lorvidhaya V. Randomized controlled trial of live lactobacillus acidophilus plus bifidobacterium bifidum in prophylaxis of diarrhea during radiotherapy in cervical cancer patients. Radiat Oncol. 2010; 5:31.11. Giralt J, Regadera JP, Verges R, Romero J, de la Fuente I, Biete A, Villoria J, Cobo JM, Guarner F. Effects of probiotic Lactobacillus casei DN-114 001 in prevention of radiation-induced diarrhea: results from multicenter, randomized, placebo-controlled nutritional trial. Int J Radiat Oncol Biol Phys. 2008; 71:1213–1219.12. Urbancsek H, Kazar T, Mezes I, Neumann K. Results of a double-blind, randomized study to evaluate the efficacy and safety of Antibiophilus in patients with radiation-induced diarrhoea. Eur J Gastroenterol Hepatol. 2001; 13:391–396.13. MacNaughton WK. Review article: new insights into the pathogenesis of radiation-induced intestinal dysfunction. Aliment Pharmacol Ther. 2000; 14:523–528.14. Driák D, Osterreicher J, Vávrová J, Reháková Z, Vilasová Z. Morphological changes of rat jejunum after whole body gamma-irradiation and their impact in biodosimetry. Physiol Res. 2008; 57:475–479.15. Rubio CA, Jalnas M. Dose-time-dependent histological changes following irradiation of the small intestine of rats. Dig Dis Sci. 1996; 41:392–401.16. Liong MT. Safety of probiotics: translocation and infection. Nutr Rev. 2008; 66:192–202.17. Gomes AMP, Malcata FX. Bifidobacterium spp. and Lactobacillus acidophilus: biological, biochemical, technological and therapeutical properties relevant for use as probiotics. Trends Food Sci Technol. 1999; 10:139–157.18. Marteau P, Shanahan F. Basic aspects and pharmacology of probiotics: an overview of pharmacokinetics, mechanisms of action and side-effects. Best Pract Res Clin Gastroenterol. 2003; 17:725–740.19. Heyman M, Ménard S. Probiotic microorganisms: how they affect intestinal pathophysiology. Cell Mol Life Sci. 2002; 59:1151–1165.20. Kang S, Chun M, Jin YM, Cho MS, Oh YT, Ahn BO, Oh TY. A rat model for radiation-induced proctitis. J Korean Med Sci. 2000; 15:682–689.21. Kiszel Z, Spiethoff A, Trott KR. Large bowel stenosis in rats after fractionated local irradiation. Radiother Oncol. 1984; 2:247–254.22. Johnson RJ, Carrington BM. Pelvic radiation disease. Clin Radiol. 1992; 45:4–12.23. Empey LR, Papp JD, Jewell LD, Fedorak RN. Mucosal protective effects of vitamin E and misoprostol during acute radiation-induced enteritis in rats. Dig Dis Sci. 1992; 37:205–214.24. Guarner F, Malagelada JR. Gut flora in health and disease. Lancet. 2003; 361:512–519.25. Kaur IP, Kuhad A, Garg A, Chopra K. Probiotics: delineation of prophylactic and therapeutic benefits. J Med Food. 2009; 12:219–235.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The reversibility of the effect of red kidney bean on the small intestinal mucosa of rat
- Effect of Probiotics on Intestinal Infections
- The dietary therapy and use of probiotics in the treatment of pediatric acute diarrhea
- An Experimental Study of the Effect of Cis-Dichlorodiammineplatinum(II) and Radiation on the Stomach of the Rats
- The Use of Probiotics in Preterm Infants