J Cerebrovasc Endovasc Neurosurg.
2014 Mar;16(1):26-31. 10.7461/jcen.2014.16.1.26.
Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm
- Affiliations
-
- 1Department of Neurological Surgery, University of Virginia, Charlottesville, VA, United States. kcl3j@hscmail.mcc.virginia.edu
- KMID: 2055281
- DOI: http://doi.org/10.7461/jcen.2014.16.1.26
Abstract
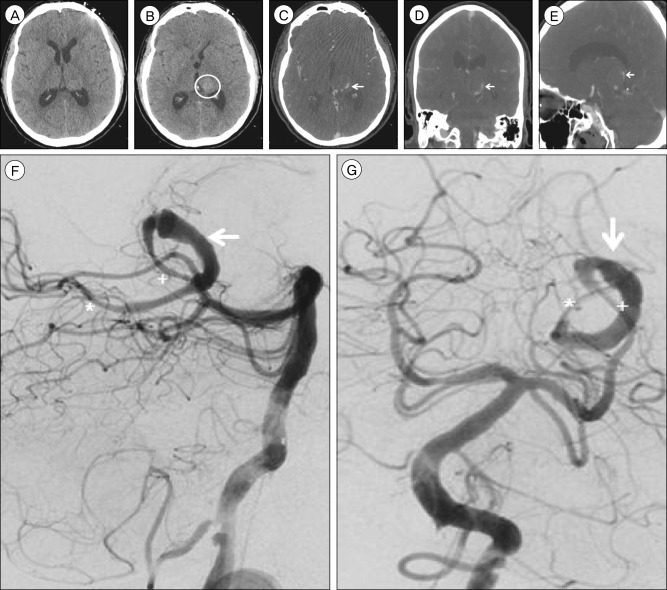
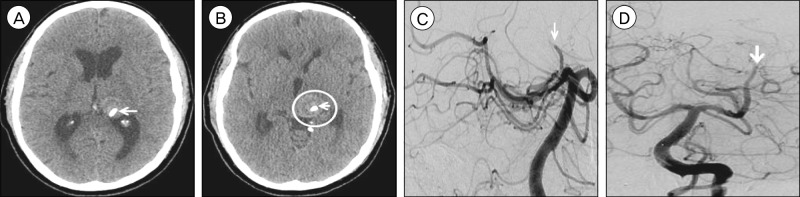
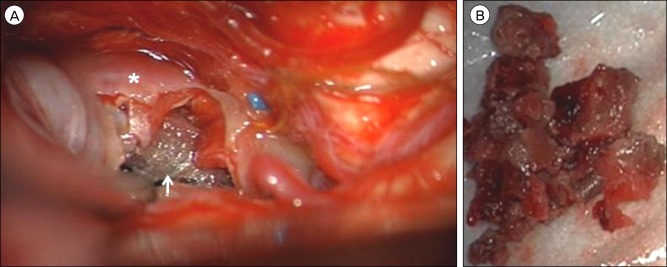
- Treatment of giant posterior circulation aneurysms, via endovascular or microsurgical approaches, carries a high risk of morbidity and mortality. While flow-diverting stents (FDSs) represent a potent therapy for endovascular reconstruction of complex aneurysms, they are also associated with novel complications for which effective salvage techniques are lacking. We present a unique complication from failed treatment with a FDS. A 51 year-old male presented with increasing headaches secondary to a giant, fusiform aneurysm of the left posterior cerebral artery, which was largely thrombosed. Due to progressive enlargement of the aneurysm corresponding to worsening clinical symptoms, the lesion was treated with two Pipeline embolization devices (ev3, Plymouth, MN, United States). Three months after Pipeline embolization device treatment, complete posterior cerebral artery occlusion was observed at the origin of the proximal stent. Despite the lack of arterial inflow, the aneurysm dome continued to grow, resulting in obstructive hydrocephalus. Therefore microsurgical intervention was undertaken to trap and excise the aneurysm. The patient's postoperative course was complicated by multiple venous infarcts, ultimately resulting in death. Successful microsurgical obliteration of aneurysms previously treated with FDSs is extremely difficult. A combination of judicious preoperative planning and meticulous intraoperative surgical technique are requisite for effective management of these complicated cases.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Endovascular Management of Intracranial Aneurysms: Advances in Stenting Techniques and Technology
Dale Ding
J Cerebrovasc Endovasc Neurosurg. 2015;17(4):331-333. doi: 10.7461/jcen.2015.17.4.331.Delayed Ischemic Stroke after Flow Diversion of Large Posterior Communicating Artery Aneurysm
Si On Kim, Yeon Gu Chung, Yu Sam Won, Myung Ho Rho
J Cerebrovasc Endovasc Neurosurg. 2016;18(1):19-26. doi: 10.7461/jcen.2016.18.1.19.
Reference
-
1. International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms - Risk of rupture and risks of surgical intervention. N Engl J Med. 1998; 12. 339(24):1725–1733. PMID: 9867550.2. Arrese I, Sarabia R, Pintado R, Delgado-Rodriguez M. Flow-diverter devices for intracranial aneurysms: Systematic review and meta-analysis. Neurosurgery. 2013; 8. 73(2):193–200. discussion 199-200. PMID: 23624409.3. Cantore G, Santoro A, Guidetti G, Delfinis CP, Colonnese C, Passacantilli E. Surgical treatment of giant intracranial aneurysms: Current viewpoint. Neurosurgery. 2008; 10. 63(4 Suppl 2):279–289. discussion 289-90. PMID: 18981833.
Article4. Dehdashti AR, Thines L, Willinsky RA, Tymianski M. Symptomatic enlargement of an occluded giant carotido-ophthalmic aneurysm after endovascular treatment: The vasa vasorum theory. Acta Neurochir (Wien). 2009; 9. 151(9):1153–1158. PMID: 19343269.
Article5. Ding D, Liu KC. Microsurgical extraction of a malfunctioned pipeline embolization device following complete deployment. J Cerebrovasc Endovasc Neurosurg. 2013; 9. 15(3):241–245. PMID: 24167807.
Article6. Drake CG. Giant intracranial aneurysms: Experience with surgical treatment in 174 patients. Clin Neurosurg. 1979; 26:12–95. PMID: 544122.
Article7. Kim YB, Lee JW, Huh SK, Kim BM, Kim DJ. Outcomes of multidisciplinary treatment for posterior cerebral artery aneurysms. Clin Neurol Neurosurg. 2013; 10. 115(10):2062–2068. PMID: 23910998.
Article8. Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, Hashimoto N, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med. 2012; 6. 366(26):2474–2482. PMID: 22738097.
Article9. Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011; 1. 32(1):34–40. PMID: 21148256.
Article10. Parkinson RJ, Eddleman CS, Batjer HH, Bendok BR. Giant intracranial aneurysms: Endovascular challenges. Neurosurgery. 2006; 11. 59(5 Suppl 3):S103–S112. discussion S3-13. PMID: 17053593.
Article11. Pistocchi S, Blanc R, Bartolini B, Piotin M. Flow diverters at and beyond the level of the circle of willis for the treatment of intracranial aneurysms. Stroke. 2012; 4. 43(4):1032–1038. PMID: 22282890.
Article12. Wajnberg E, Silva TS, Johnson AK, Lopes DK. Progressive deconstruction: A novel aneurysm treatment using the pipeline embolization device for competitive flow diversion. Neurosurgery. 2014; 3. 10(Suppl 1):E161–E166. PMID: 23787883.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm
- Microsurgical Extraction of a Malfunctioned Pipeline Embolization Device Following Complete Deployment
- Inadvertent Complication of a Pipeline Embolization Device for Treatment with Vertebral Artery Dissecting Aneurysm : Distal Tip Fracture of Delivery Wire
- Balloon Anchor Technique for Pipeline Embolization Device Deployment Across the Neck of a Giant Intracranial Aneurysm
- Dissecting Aneurysm of the Posterior Cerebral Artery Masquerading as Saccular Giant Aneurysm