Yonsei Med J.
2015 Mar;56(2):482-489. 10.3349/ymj.2015.56.2.482.
What Number of Oocytes Is Appropriate for Defining Poor Ovarian Response?
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Korea. blasto@snubh.org
- 2Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2070028
- DOI: http://doi.org/10.3349/ymj.2015.56.2.482
Abstract
- PURPOSE
This study attempted to derive an objective and sophisticated definition of poor ovarian response (POR).
MATERIALS AND METHODS
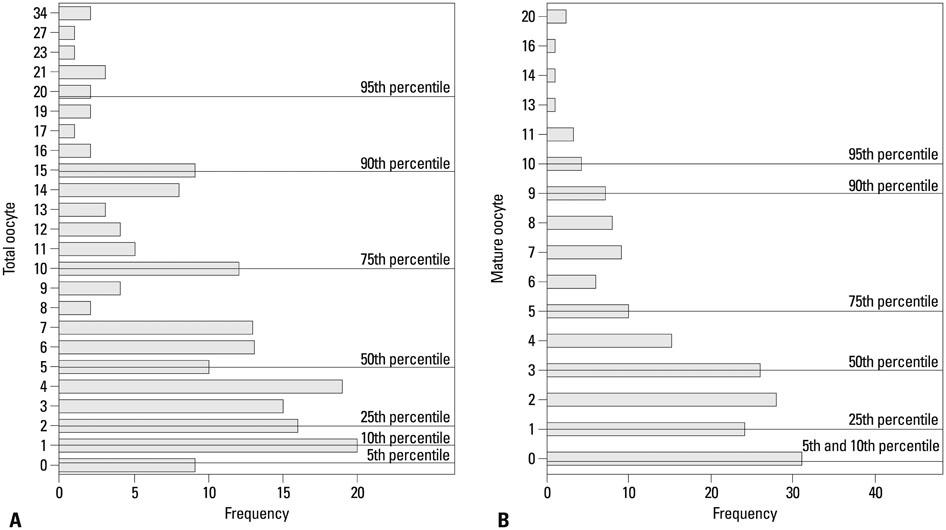
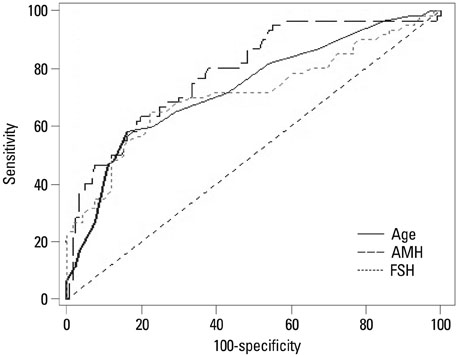
A total of 176 consecutive in vitro fertilization (IVF) cycles (137 patients) with conventional ovarian stimulation during 2009 to 2012 were studied by retrospective analysis. Optimal oocyte number (total or mature) was determined by statistics-based (distribution of oocyte number) and prognosis-based approaches (prediction for IVF outcome). Receiver operating characteristics curve analysis was used to show what number of oocytes could predict IVF pregnancy and whether clinical and laboratory variables could predict newly defined POR.
RESULTS
The 25th percentile of the distribution corresponded to total oocytes < or =2 and mature oocyte < or =1. The cut-off values for the prediction of IVF outcomes were total oocytes >5 and mature oocyte >1. Considering the incidence of POR (34.1%), a reasonable definition of POR was decided as total oocytes < or =2 or mature oocyte < or =1. For the prediction of this new definition, the extreme cut-off value (by setting a false positive rate of 5%) of serum anti-Mullerian hormone (AMH) was < or =0.76 ng/mL, which was better than serum follicle stimulating hormone or age. A new simple definition of POR was derived as total oocytes < or =2 or mature oocyte < or =1 in a previous cycle or a serum AMH level of < or =0.76 ng/mL. When this simple criterion was re-applied to our data, the predictive performance was similar to the Bologna criteria.
CONCLUSION
We here propose a new definition of POR, which is simple and supported by statistical and prognostic analyses.
MeSH Terms
-
Adult
Anti-Mullerian Hormone/blood
Female
Fertilization in Vitro
Follicle Stimulating Hormone/blood
Humans
Infertility, Female/blood/*therapy
*Oocytes
*Ovulation Induction
Pregnancy
Prognosis
ROC Curve
Retrospective Studies
*Sperm Injections, Intracytoplasmic
Treatment Outcome
Anti-Mullerian Hormone
Follicle Stimulating Hormone
Figure
Reference
-
1. Pandian Z, McTavish AR, Aucott L, Hamilton MP, Bhattacharya S. Interventions for 'poor responders' to controlled ovarian hyper stimulation (COH) in in-vitro fertilisation (IVF). Cochrane Database Syst Rev. 2010; 20:CD004379.
Article2. Frydman R. Poor responders: still a problem. Fertil Steril. 2011; 96:1057.
Article3. Polyzos NP, Devroey P. A systematic review of randomized trials for the treatment of poor ovarian responders: is there any light at the end of the tunnel? Fertil Steril. 2011; 96:1058–1061.4. Practice Committee of the American Society for Reproductive Medicine. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril. 2012; 98:1407–1415.5. Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of 'poor response' to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011; 26:1616–1624.
Article6. Polyzos NP, Tournaye H, Devroey P. AMH for predicting poor ovarian responders in GnRH antagonist cycles. Hum Reprod. 2012; 27:1876–1877.
Article7. Polyzos NP, De Vos M, Corona R, Vloeberghs V, Ortega-Hrepich C, Stoop D, et al. Addition of highly purified HMG after corifollitropin alfa in antagonist-treated poor ovarian responders: a pilot study. Hum Reprod. 2013; 28:1254–1260.
Article8. Younis JS. The Bologna criteria for poor ovarian response; has the job been accomplished? Hum Reprod. 2012; 27:1874–1875.
Article9. Sallam HN, Ezzeldin F, Agameya AF, Abdel-Rahman AF, El-Garem Y. The definition of 'poor response': Bologna criteria. Hum Reprod. 2012; 27:626–627.
Article10. Lee JE, Lee JR, Jee BC, Suh CS, Kim KC, Lee WD, et al. Clinical application of anti-Müllerian hormone as a predictor of controlled ovarian hyperstimulation outcome. Clin Exp Reprod Med. 2012; 39:176–181.
Article11. Sallam HN, Ezzeldin F, Agameya AF, Rahman AF, El-Garem Y. Defining poor responders in assisted reproduction. Int J Fertil Womens Med. 2005; 50:115–120.12. McAvey B, Zapantis A, Jindal SK, Lieman HJ, Polotsky AJ. How many eggs are needed to produce an assisted reproductive technology baby: is more always better? Fertil Steril. 2011; 96:332–335.
Article13. La Marca A, Argento C, Sighinolfi G, Grisendi V, Carbone M, D'Ippolito G, et al. Possibilities and limits of ovarian reserve testing in ART. Curr Pharm Biotechnol. 2012; 13:398–408.
Article14. Ledger WL. Clinical utility of measurement of anti-mullerian hormone in reproductive endocrinology. J Clin Endocrinol Metab. 2010; 95:5144–5154.
Article15. van Rooij IA, Broekmans FJ, te Velde ER, Fauser BC, Bancsi LF, de Jong FH, et al. Serum anti-Müllerian hormone levels: a novel measure of ovarian reserve. Hum Reprod. 2002; 17:3065–3071.16. Nelson SM, Yates RW, Fleming R. Serum anti-Müllerian hormone and FSH: prediction of live birth and extremes of response in stimulated cycles--implications for individualization of therapy. Hum Reprod. 2007; 22:2414–2421.
Article17. Muttukrishna S, Suharjono H, McGarrigle H, Sathanandan M. Inhibin B and anti-Mullerian hormone: markers of ovarian response in IVF/ICSI patients? BJOG. 2004; 111:1248–1253.
Article18. Kwee J, Schats R, McDonnell J, Themmen A, de Jong F, Lambalk C. Evaluation of anti-Müllerian hormone as a test for the prediction of ovarian reserve. Fertil Steril. 2008; 90:737–743.
Article19. La Marca A, Malmusi S, Giulini S, Tamaro LF, Orvieto R, Levratti P, et al. Anti-Müllerian hormone plasma levels in spontaneous menstrual cycle and during treatment with FSH to induce ovulation. Hum Reprod. 2004; 19:2738–2741.
Article20. Fiçicioglu C, Kutlu T, Baglam E, Bakacak Z. Early follicular antimüllerian hormone as an indicator of ovarian reserve. Fertil Steril. 2006; 85:592–596.
Article21. Ebner T, Sommergruber M, Moser M, Shebl O, Schreier-Lechner E, Tews G. Basal level of anti-Müllerian hormone is associated with oocyte quality in stimulated cycles. Hum Reprod. 2006; 21:2022–2026.
Article22. Hazout A, Bouchard P, Seifer DB, Aussage P, Junca AM, Cohen-Bacrie P. Serum antimüllerian hormone/müllerian-inhibiting substance appears to be a more discriminatory marker of assisted reproductive technology outcome than follicle-stimulating hormone, inhibin B, or estradiol. Fertil Steril. 2004; 82:1323–1329.
Article23. Elgindy EA, El-Haieg DO, El-Sebaey A. Anti-Müllerian hormone: correlation of early follicular, ovulatory and midluteal levels with ovarian response and cycle outcome in intracytoplasmic sperm injection patients. Fertil Steril. 2008; 89:1670–1676.
Article24. Gnoth C, Schuring AN, Friol K, Tigges J, Mallmann P, Godehardt E. Relevance of anti-Mullerian hormone measurement in a routine IVF program. Hum Reprod. 2008; 23:1359–1365.
Article25. Bancsi LF, Broekmans FJ, Mol BW, Habbema JD, te Velde ER. Performance of basal follicle-stimulating hormone in the prediction of poor ovarian response and failure to become pregnant after in vitro fertilization: a meta-analysis. Fertil Steril. 2003; 79:1091–1100.
Article26. Bancsi LF, Broekmans FJ, Looman CW, Habbema JD, te Velde ER. Predicting poor ovarian response in IVF: use of repeat basal FSH measurement. J Reprod Med. 2004; 49:187–194.27. Buyuk E, Seifer DB, Younger J, Grazi RV, Lieman H. Random anti-Müllerian hormone (AMH) is a predictor of ovarian response in women with elevated baseline early follicular follicle-stimulating hormone levels. Fertil Steril. 2011; 95:2369–2372.
Article28. Silberstein T, MacLaughlin DT, Shai I, Trimarchi JR, Lambert-Messerlian G, Seifer DB, et al. Mullerian inhibiting substance levels at the time of HCG administration in IVF cycles predict both ovarian reserve and embryo morphology. Hum Reprod. 2006; 21:159–163.
Article29. Buyuk E, Seifer DB, Illions E, Grazi RV, Lieman H. Elevated body mass index is associated with lower serum anti-mullerian hormone levels in infertile women with diminished ovarian reserve but not with normal ovarian reserve. Fertil Steril. 2011; 95:2364–2368.
Article30. Merhi ZO, Minkoff H, Feldman J, Macura J, Rodriguez C, Seifer DB. Relationship of bariatric surgery to Müllerian-inhibiting substance levels. Fertil Steril. 2008; 90:221–224.
Article31. Dennis NA, Houghton LA, Jones GT, van Rij AM, Morgan K, McLennan IS. The level of serum anti-Müllerian hormone correlates with vitamin D status in men and women but not in boys. J Clin Endocrinol Metab. 2012; 97:2450–2455.
Article32. Merhi Z, Buyuk E, Berger DS, Zapantis A, Israel DD, Chua S Jr, et al. Leptin suppresses anti-Mullerian hormone gene expression through the JAK2/STAT3 pathway in luteinized granulosa cells of women undergoing IVF. Hum Reprod. 2013; 28:1661–1669.
Article33. Jayaprakasan K, Campbell B, Hopkisson J, Johnson I, Raine-Fenning N. A prospective, comparative analysis of anti-Müllerian hormone, inhibin-B, and three-dimensional ultrasound determinants of ovarian reserve in the prediction of poor response to controlled ovarian stimulation. Fertil Steril. 2010; 93:855–864.
Article34. Merhi Z, Zapantis A, Berger DS, Jindal SK. Determining an anti-Mullerian hormone cutoff level to predict clinical pregnancy following in vitro fertilization in women with severely diminished ovarian reserve. J Assist Reprod Genet. 2013; 30:1361–1365.
Article35. Gleicher N, Weghofer A, Barad DH. Anti-Müllerian hormone (AMH) defines, independent of age, low versus good live-birth chances in women with severely diminished ovarian reserve. Fertil Steril. 2010; 94:2824–2827.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of mild ovarian stimulation with conventional ovarian stimulation in poor responders
- Effect of a Baseline Ovarian Cyst on the Outcome of in Vitro Fertilization-embryo Transfer
- Serum anti-Mullerian hormone is a better predictor of ovarian response than FSH and age in IVF patients with endometriosis
- Serum anti-Mullerian hormone levels as a predictor of the ovarian response and IVF outcomes
- Correlation of Basal AMH & Ovarian Response in IVF Cycles; Predictive Value of AMH