J Korean Neurosurg Soc.
2013 Jan;53(1):26-30. 10.3340/jkns.2013.53.1.26.
Short Segment Fixation for Thoracolumbar Burst Fracture Accompanying Osteopenia : A Comparative Study
- Affiliations
-
- 1Department of Neurosurgery, Heori Sarang Hospital, Daejeon, Korea.
- 2Department of Neurosurgery, College of Medicine, Chosun University, Gwangju, Korea. chosunns@chosun.ac.kr
- KMID: 2066981
- DOI: http://doi.org/10.3340/jkns.2013.53.1.26
Abstract
OBJECTIVE
The purpose of this study was to compare the results of three types of short segment screw fixation for thoracolumbar burst fracture accompanying osteopenia.
METHODS
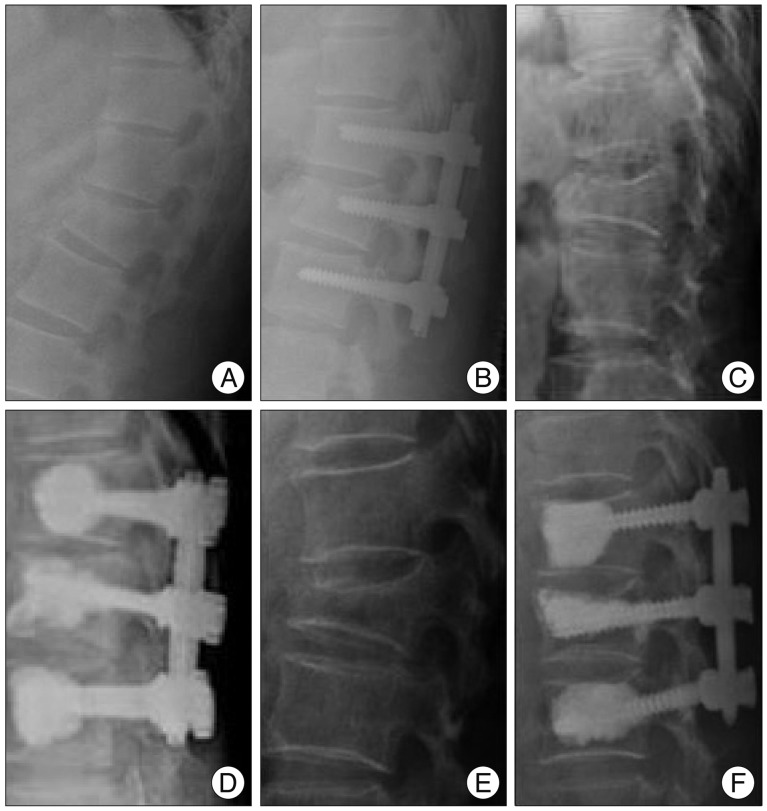
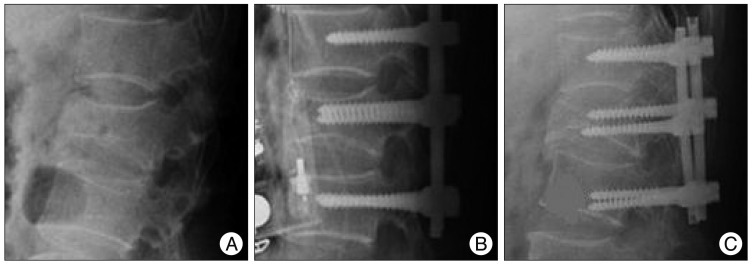
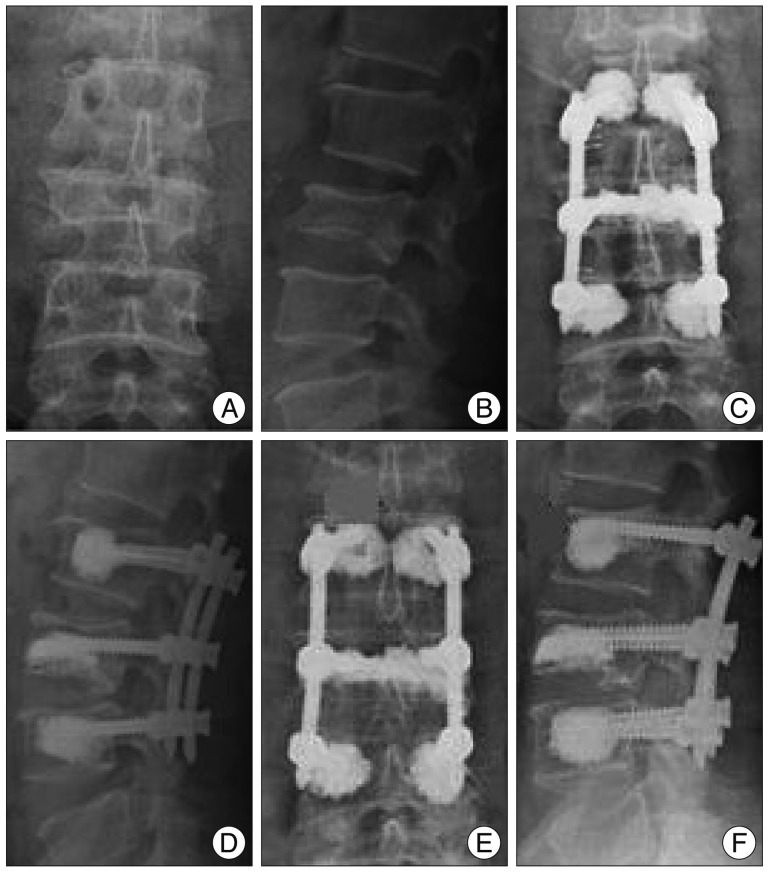
The records of 70 patients who underwent short segment screw fixation for a thoracolumbar burst fracture accompanying osteopenia (-2.5< mean T score by bone mineral densitometry <-1.0) from January 2005 to January 2008 were reviewed. Patients were divided into three groups based on whether or not bone fusion and bone cement augmentation procedure 1) Group I (n=26) : short segment fixation with posterolateral bone fusion; 2) Group II (n=23) : bone cement augmented short segment fixation with posterolateral bone fusion; 3) Group III (n=21) : bone cement augmented, short segment percutaneous screw fixation without bone fusion. Clinical outcomes were assessed using a visual analogue scale and modified MacNab's criteria. Radiological findings, including kyphotic angle and vertebral height, and procedure-related complications, such as screw loosening or pull-out, were analyzed.
RESULTS
No significant difference in radiographic or clinical outcomes was noted between patients managed using the three different techniques at last follow up. However, Group I showed more correction loss of kyphotic deformities and vertebral height loss at final follow-up, and Group I had higher screw loosening and implant failure rates than Group II or III.
CONCLUSION
Bone cement augmented procedure can be an efficient and safe surgical techniques in terms of achieving better outcomes with minimal complications for thoracolumbar burst fracture accompanying osteopenia.
Keyword
Figure
Cited by 2 articles
-
Implant Removal after Percutaneous Short Segment Fixation for Thoracolumbar Burst Fracture : Does It Preserve Motion?
Hyeun Sung Kim, Seok Won Kim, Chang Il Ju, Hui Sun Wang, Sung Myung Lee, Dong Min Kim
J Korean Neurosurg Soc. 2014;55(2):73-77. doi: 10.3340/jkns.2014.55.2.73.Bone Cement-Augmented Percutaneous Short Segment Fixation: An Effective Treatment for Kummell's Disease?
Seon Joo Park, Hyeun Sung Kim, Seok Ki Lee, Seok Won Kim
J Korean Neurosurg Soc. 2015;58(1):54-59. doi: 10.3340/jkns.2015.58.1.54.
Reference
-
1. Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery. 2003; 53:1354–1360. discussion 1360-1361. PMID: 14633301.
Article2. Hakalo J, Wroński J. [Complications of a transpedicular stabilization of thoraco-lumbar burst fractures]. Neurol Neurochir Pol. 2006; 40:134–139. PMID: 16628510.3. Kim HY, Kim HS, Kim SW, Ju CI, Lee SM, Park HJ. Short segment screw fixation without fusion for unstable thoracolumbar and lumbar burst fracture : a prospective study on selective consecutive patients. J Korean Neurosurg Soc. 2012; 51:203–207. PMID: 22737299.
Article4. Lee YS, Sung JK. Long-term follow-up results of short-segment posterior screw fixation for thoracolumbar burst fractures. J Korean Neurosurg Soc. 2005; 37:416–421.5. Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures : a consecutive 41/2-year series. Spine (Phila Pa 1976). 2000; 25:1157–1170. PMID: 10788862.
Article6. Sanderson PL, Fraser RD, Hall DJ, Cain CM, Osti OL, Potter GR. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999; 8:495–500. PMID: 10664310.
Article7. Soshi S, Shiba R, Kondo H, Murota K. An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine (Phila Pa 1976). 1991; 16:1335–1341. PMID: 1750009.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short Segment versus Long Segment Pedicle Screws Fixation in Management of Thoracolumbar Burst Fractures: Meta-Analysis
- Comparison of Short Segment and Long Segment Posterior Instrumentation of Thoracolumbar and Lumbar Bursting Fractures at Load Sharing Score 7 or Above
- Long-term Follow-up Results of Short-segment Posterior Screw Fixation for Thoracolumbar Burst Fractures
- Decision of Posterior Fixation Level by Load-Sharing Classification in Thoracolumbar and Lumbar Burst Fracture
- Bone Cement-Augmented Short Segment Fixation with Percutaneous Screws for Thoracolumbar Burst Fractures Accompanied by Severe Osteoporosis