J Korean Med Assoc.
2012 Jun;55(6):551-561. 10.5124/jkma.2012.55.6.551.
Clinical applications and limitations of a special formula for diarrhea in children
- Affiliations
-
- 1Department of Pediatrics, Dankook University College of Medicine, Cheonan, Korea. pdlks@dankook.ac.kr
- 2Department of Pediatrics, Konkuk University School of Medicine, Chungju, Korea.
- KMID: 2015654
- DOI: http://doi.org/10.5124/jkma.2012.55.6.551
Abstract
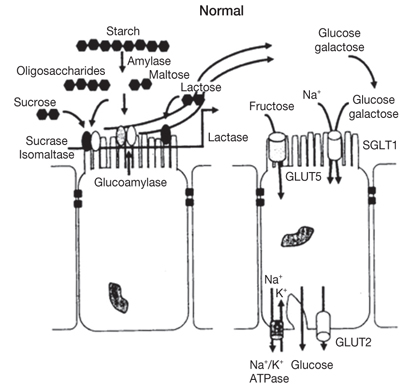
- Diarrheal disorders in childhood are the second most common cause of child deaths worldwide. Nutritional rehabilitation is the most important factor among treatments when diarrheal disorders develop and has a general beneficial effect on the patient's condition, intestinal function, and immune response. Breast milk is the most nutritious food for treating acute and chronic diarrhea in infants. Until now, many infant formulas have been developed, and particularly, special formulas for treating acute or chronic diarrhea are commonly used. Lactose-free formulas, soy based formulas, and hydrolyzed and amino acid-based formula are typical formulas. In general, replacement with specialized lactose-free formulations is unnecessary in children with persistent diarrhea, and it has been reported that infants that are not severely compromised have food allergy and intestinal failure. However, a general knowledge does not always applied to all populations because the genetic, economic or environmental factors are different. Physicians should know about the components and characteristics of special formulas in order to coach parents to use these formulas properly.
Keyword
Figure
Cited by 2 articles
-
How to Do in Persistent Diarrhea of Children?: Concepts and Treatments of Chronic Diarrhea
Kun Song Lee, Dong Soo Kang, Jeesuk Yu, Young Pyo Chang, Woo Sung Park
Pediatr Gastroenterol Hepatol Nutr. 2012;15(4):229-236. doi: 10.5223/pghn.2012.15.4.229.Acute and chronic diarrhea in children: back to the basics again
Jin-Bok Hwang
J Korean Med Assoc. 2012;55(6):513-515. doi: 10.5124/jkma.2012.55.6.513.
Reference
-
1. Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE. Nelson textbook of pediatics. 2011. 19th ed. Philadelphia: Saunders Co..2. Guarino A, Albano F, Ashkenazi S, Gendrel D, Hoekstra JH, Shamir R, Szajewska H. European Society for Paediatric Gastroenterology, Hepatology, and Nutrition. European Society for Paediatric Infectious Diseases. European Society for Paediatric Gastroenterology, Hepatology, and Nutrition/European Society for Paediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe. J Pediatr Gastroenterol Nutr. 2008. 46:Suppl 2. S81–S122.3. Kim YH, Lee SG, Kim SH, Song YJ, Chung JY, Park MJ. Nutritional status of Korean toddlers: from the Korean National Health and Nutrition Examination Survey 2007-2009. Korean J Pediatr Gastroenterol Nutr. 2011. 14:161–170.
Article4. Choe YH, Moon KR, Weo JW, Sim JG, Yoo KW, Jeong BJ, Hong YM. Nationwide survey on current status of formula feeding in infants. J Korean Pediatr Soc. 2000. 43:878–888.5. Martinez JA, Ballew MP. Infant formulas. Pediatr Rev. 2011. 32:179–189.
Article6. Lee SJ. Special infant formula. J Korean Pediatr Soc. 1996. 39:180–186.7. Hwang JB. Clinical approaches for diarrheal disorders in infancy and early childhood. 1999. Daegu: Choongwae Publishing.8. Chu MA, Choe BH. Nutritional support for acute diarrhea in children: focused on age-appropriate diet therapy after rehydration. Korean J Pediatr Gastroenterol Nutr. 2009. 12:Suppl 1. S53–S61.
Article9. Guarino A, Albano F, Ashkenazi S, Gendrel D, Hoekstra JH, Shamir R, Szajewska H. ESPGHAN/ESPID Evidence-Based Guidelines for the Management of Acute Gastroenteritis in Children in Europe Expert Working Group. European Society for Paediatric Gastroenterology, Hepatology, and Nutrition/European Society for Paediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: executive summary. J Pediatr Gastroenterol Nutr. 2008. 46:619–621.
Article10. Kleinman RE. American Academy of Pediatrics Commmittee on Nutrition. Pediatric nutrition handbook. 2009. 6th ed. Elk Grove Village: American Academy of Pediatrics.11. Kleinman RE, Goulet OJ, Mieli-Vergani G, Sanderson IR, Sherman P, Shneider BL. Walker's pediatric gastrointestinal disease: physiology, diagnosis, management. 2008. 5th ed. Hamilton: BC Decker Inc..12. Lasekan JB, Jacobs J, Reisinger KS, Montalto MB, Frantz MP, Blatter MM. Lactose-free milk protein-based infant formula: impact on growth and gastrointestinal tolerance in infants. Clin Pediatr (Phila). 2011. 50:330–337.
Article13. Dalgic N, Sancar M, Bayraktar B, Pullu M, Hasim O. Probiotic, zinc and lactose-free formula in children with rotavirus diarrhea: are they effective? Pediatr Int. 2011. 53:677–682.
Article14. Brown KH, Peerson JM, Fontaine O. Use of nonhuman milks in the dietary management of young children with acute diarrhea: a meta-analysis of clinical trials. Pediatrics. 1994. 93:17–27.
Article15. Rao P, Rao N, Jordinson M, Scott C, Hinchcliffe C, Campbell D. Comparison of quick point-of-care test for small-bowel hypolactasia with biochemical lactase assay in children. J Pediatr Gastroenterol Nutr. 2012. 54:401–403.
Article16. Simakachorn N, Tongpenyai Y, Tongtan O, Varavithya W. Randomized, double-blind clinical trial of a lactose-free and a lactose-containing formula in dietary management of acute childhood diarrhea. J Med Assoc Thai. 2004. 87:641–649.17. Xu JH, Huang Y. Efficiency of lactose-free formula feeding as an adjunctive therapy in infants with acute diarrhea. Zhongguo Dang Dai Er Ke Za Zhi. 2009. 11:532–536.18. Leake RD, Schroeder KC, Benton DA, Oh W. Soy-based formula in the treatment of infantile diarrhea. Am J Dis Child. 1974. 127:374–376.19. Chang SY, Park HS, Lee KS. Clinical trials of lactose free soy-protein formula for infantile diarrhea. J Korean Pediatr Soc. 1982. 25:58–65.20. Dinsdale EC, Ward WE. Early exposure to soy isoflavones and effects on reproductive health: a review of human and animal studies. Nutrients. 2010. 2:1156–1187.
Article21. Bhatia J, Greer F. American Academy of Pediatrics Committee on Nutrition. Use of soy protein-based formulas in infant feeding. Pediatrics. 2008. 121:1062–1068.
Article22. Hill DJ, Murch SH, Rafferty K, Wallis P, Green CJ. The efficacy of amino acid-based formulas in relieving the symptoms of cow's milk allergy: a systematic review. Clin Exp Allergy. 2007. 37:808–822.
Article23. Lee KS. The diagnosis of food allergy in a pediatric gastroenterology: focusing on non-IgE-mediated allergic diseases. Korean J Pediatr Gastroenterol Nutr. 2010. 13:Suppl 1. S32–S43.
Article24. De Greef E, Mahler T, Janssen A, Cuypers H, Veereman-Wauters G. The influence of neocate in paediatric short bowel syndrome on PN weaning. J Nutr Metab. 2010. [Epub]. DOI: 10.1155/2010/297575.
Article25. Bines J, Francis D, Hill D. Reducing parenteral requirement in children with short bowel syndrome: impact of an amino acid-based complete infant formula. J Pediatr Gastroenterol Nutr. 1998. 26:123–128.
Article26. De Mattos AP, Ribeiro TC, Mendes PS, Valois SS, Mendes CM, Ribeiro HC Jr. Comparison of yogurt, soybean, casein, and amino acid-based diets in children with persistent diarrhea. Nutr Res. 2009. 29:462–469.
Article27. Koletzko B, Cooper P, Makrides M, Garza C, Uauy R, Wang W. Pediatric nutrition in practice. 2008. Basel: Karger.28. Gastanaduy A, Cordano A, Graham GG. Acceptability, tolerance, and nutritional value of a rice-based infant formula. J Pediatr Gastroenterol Nutr. 1990. 11:240–246.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Low Lactose Special Formula (MF-1)for the Treatment of Acute Diarrhea in Infants
- Types of Special Infant Formulas Marketed in Korea and Their Indications
- Nutritional Support for Acute Diarrhea in Children:Focused on Age-appropriate Diet Therapy after Rehydration
- Clinical Trials of Lactose Free Soyprotein Formula for Infantile Diarrhea
- How to Do in Persistent Diarrhea of Children?: Concepts and Treatments of Chronic Diarrhea