J Korean Med Assoc.
2012 Jun;55(6):539-545. 10.5124/jkma.2012.55.6.539.
Toward an objective definition of diarrhea for differential diagnosis of chronic diarrhea in infants and toddlers
- Affiliations
-
- 1Department of Pediatrics, Keimyung University School of Medicine, Daegu, Korea. pedgi@kmu.ac.kr
- KMID: 2015652
- DOI: http://doi.org/10.5124/jkma.2012.55.6.539
Abstract
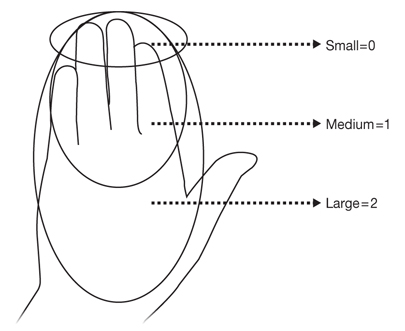
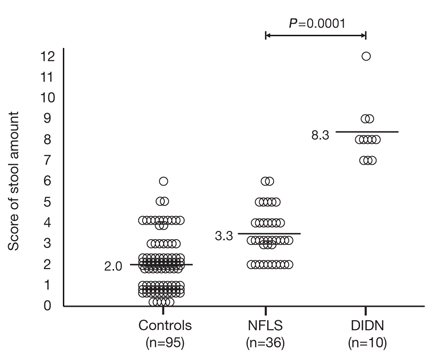
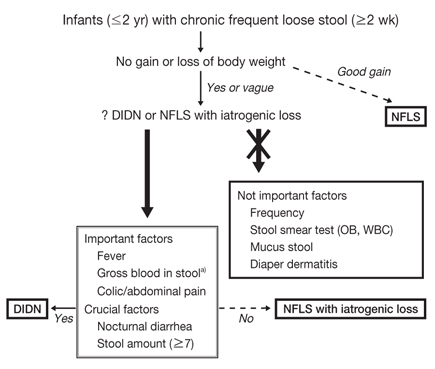
- Among infants and toddlers with chronic frequent loose stool, normal frequent and loose stool (NFLS) is more common than diarrheal illness with dehydration and nutritional deficiency (DIDN). To identify more objective factors for differentiating between NFLS and DIDN is important. The frequency, mucus content, and microbiological findings of stools, as well as diaper dermatitis are not important factors to significantly differentiate the groups. Instead, a failure to gain weight, fever, colic/abdominal pain, gross blood in stool (except allergic proctocolitis), nocturnal stool, and the score of the stool quantity are important factors to significantly differentiate the groups. A failure to gain weight is also observed even in NFLS, which may come from iatrogenic diet manipulation with nutritionally deficient food. The most objective differential factors are nocturnal stool and the score of stool amount (> or =7 points/day). The use of these objective factors could lessen parental anxiety and distress, iatrogenic undernutrition of patients, and socioeconomic loss due to improper medical investigations or inappropriate management of NFLS.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Acute and chronic diarrhea in children: back to the basics again
Jin-Bok Hwang
J Korean Med Assoc. 2012;55(6):513-515. doi: 10.5124/jkma.2012.55.6.513.
Reference
-
1. Weaver LT. Bowel habit from birth to old age. J Pediatr Gastroenterol Nutr. 1988. 7:637–640.
Article2. Baldassano RN, Liacouras CA. Chronic diarrhea: a practical approach for the pediatrician. Pediatr Clin North Am. 1991. 38:667–686.
Article3. Rhoads JM, Powell DW. Walker WA, Durie PR, Hamilton JR, Walker-Smith JA, Watkins JB, editors. Diarrhea. Pediatric gastrointestinal disease: pathophysiology, diagnosis, management. 1996. 2nd ed. St. Louis: Mosby;62–78.4. Scaillon M, Cadranel S. Hyman PE, Di Lorenzo C, editors. Transit tests. Pediatric gastrointestinal motility disorders. 1994. New York: Academy Professional Information Services;265–276.5. Hwang JB, Kang KJ, Lee JJ, Kim AS. What is the objective differential factor of diarrhea in infancy?: Normal state versus diarrheal illness in infants with chronic frequent and loose stool. Korean J Pediatr. 2010. 53:1006–1011.
Article6. Maloney J, Nowak-Wegrzyn A. Educational clinical case series for pediatric allergy and immunology: allergic proctocolitis, food protein-induced enterocolitis syndrome and allergic eosinophilic gastroenteritis with protein-losing gastroenteropathy as manifestations of non-IgE-mediated cow's milk allergy. Pediatr Allergy Immunol. 2007. 18:360–367.
Article7. Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, Staiano A. Childhood functional gastrointestinal disorders. Gut. 1999. 45:Suppl 2. II60–II68.
Article8. Liu LJ, Yang YJ, Kuo PH, Wang SM, Liu CC. Diagnostic value of bacterial stool cultures and viral antigen tests based on clinical manifestations of acute gastroenteritis in pediatric patients. Eur J Clin Microbiol Infect Dis. 2005. 24:559–561.
Article9. Heyman MB. Committee on Nutrition. Lactose intolerance in infants, children, and adolescents. Pediatrics. 2006. 118:1279–1286.
Article10. Hwang JB, Park MH, Kang YN, Kim SP, Suh SI, Kam S. Advanced criteria for clinicopathological diagnosis of food protein-induced proctocolitis. J Korean Med Sci. 2007. 22:213–217.
Article11. Kleinman RE. Chronic nonspecific diarrhea of childhood. Nestle Nutr Workshop Ser Pediatr Program. 2005. 56:73–79.
Article12. Brook I. Pseudomembranous colitis in children. J Gastroenterol Hepatol. 2005. 20:182–186.
Article13. Misra S, Sabui TK, Pal NK. A randomized controlled trial to evaluate the efficacy of lactobacillus GG in infantile diarrhea. J Pediatr. 2009. 155:129–132.
Article14. Kim JY, Hwang SJ, Park HK, Lee H, Kim NS. Analysis of online breast-feeding consultation on the website of the Korean Pediatric Society. Korean J Pediatr. 2008. 51:1152–1157.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gaps between Infant Diarrheal Disease and Frequent Loose Stool
- The Comparison of Clinical Characteristics in Three Types of Viral Acute Diarrhea in Infants and Toddlers and the Effect of Lactobacillus acidophilus on Rotaviral Diarrhea
- How to Do in Persistent Diarrhea of Children?: Concepts and Treatments of Chronic Diarrhea
- The New Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers
- Diagnosis and Management of Chronic Diarrhea