Diabetes Metab J.
2019 Dec;43(6):879-892. 10.4093/dmj.2018.0202.
Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. ymchomd@snu.ac.kr
- 2Department of internal Medicine, Korea University College of Medicine, Seoul, Korea.
- KMID: 2466508
- DOI: http://doi.org/10.4093/dmj.2018.0202
Abstract
- BACKGROUND
A premeal load of protein can increase satiety and reduce energy intake. Dietary fiber also conveys metabolic benefits by modulating energy intake. We made a protein-enriched, dietary fiber-fortified bar (PFB) and aimed to investigate its effects on food intake and gut hormone secretion in healthy individuals.
METHODS
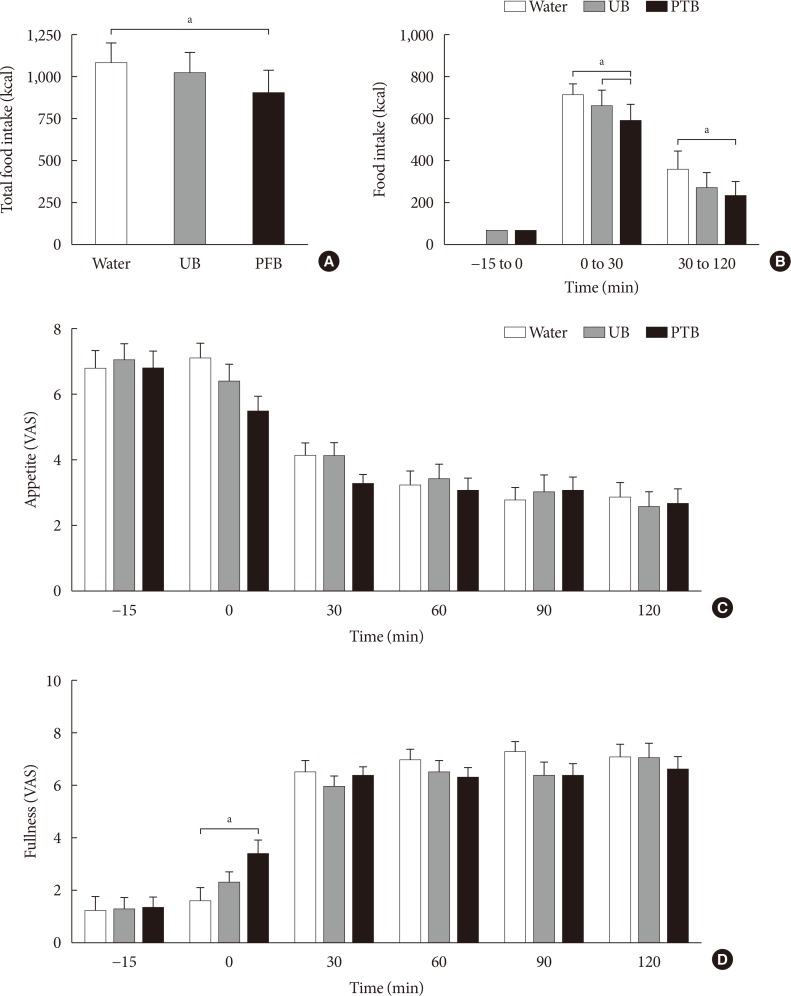
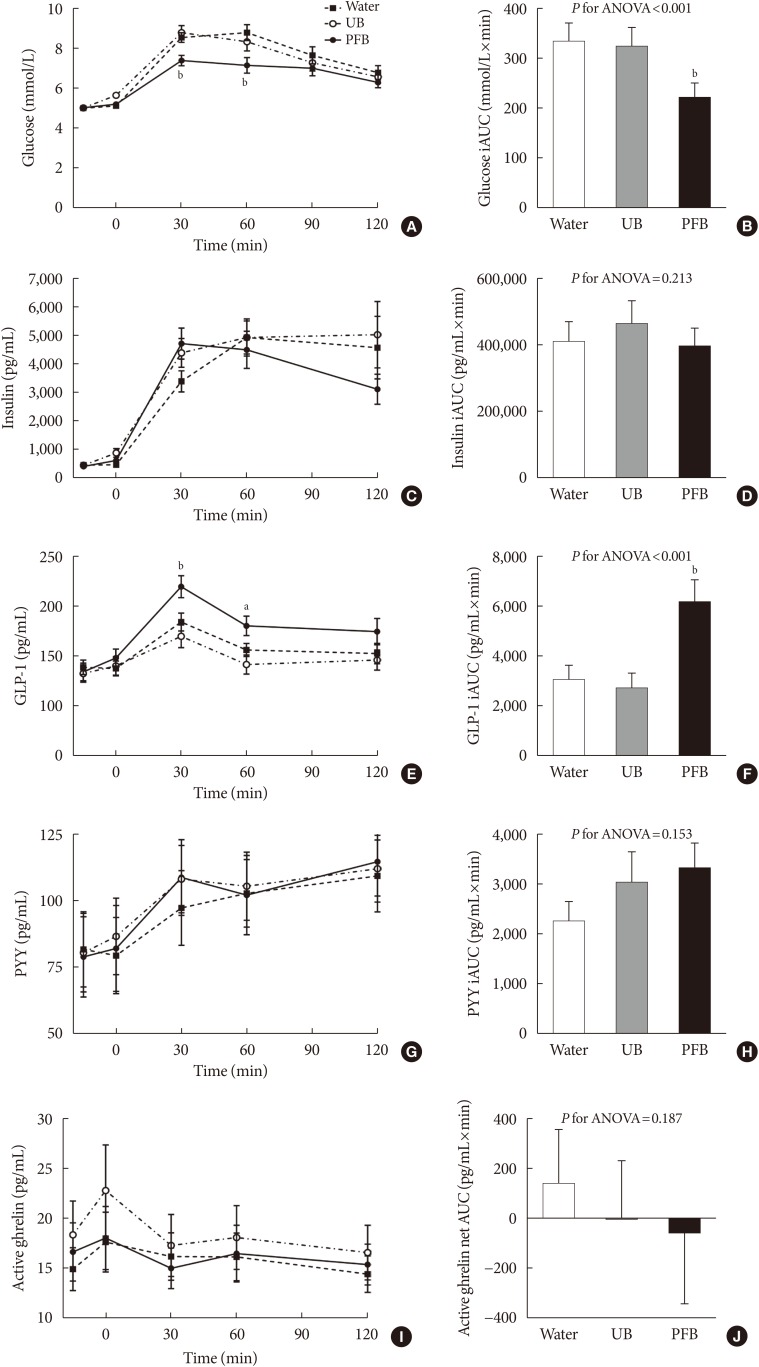
Twenty subjects with normal glucose tolerance were enrolled. On three separate visits, the subjects received, in a randomized order, one of the following: a PFB containing 73 kcal with 10.7 g of protein and 12.7 g of dietary fiber; a usual bar (UB) containing the same calories as the PFB but only 0.9 g of protein and no dietary fiber; or water (control). After 15 minutes, the subjects had ad libitum intake of a test meal. Food consumption, appetite, and plasma gut hormone levels were measured.
RESULTS
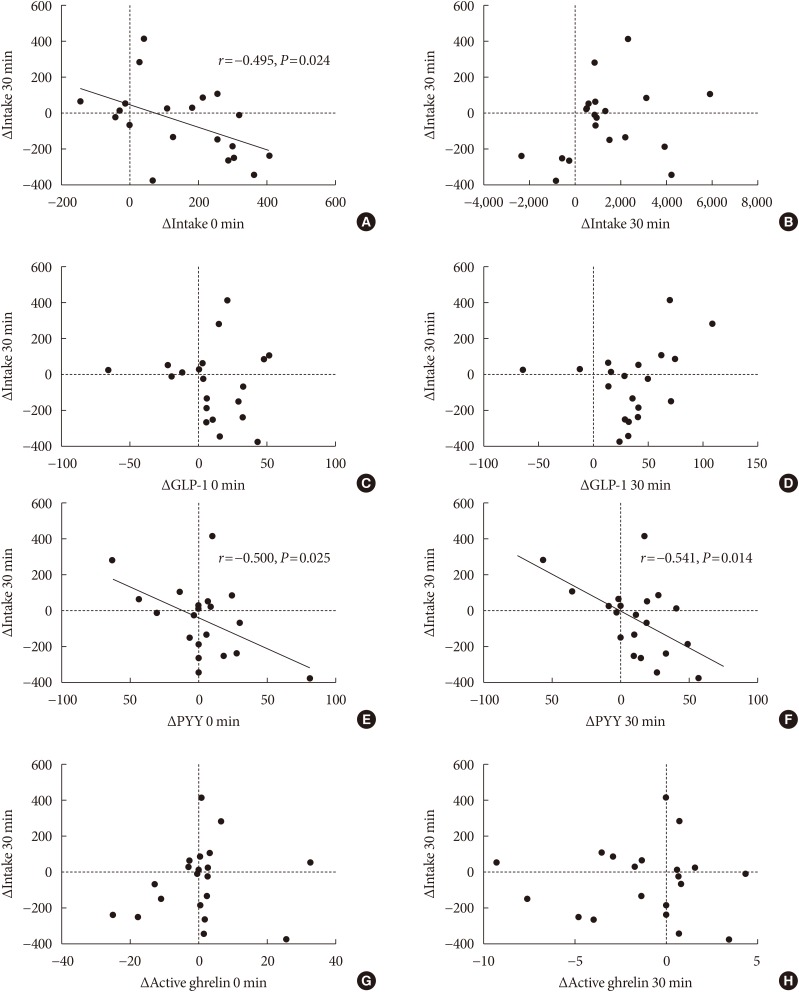
Total energy intake, including the bar and the test meal, was significantly reduced with the PFB preload compared to the water (904.4±534.9 kcal vs. 1,075.0±508.0 kcal, P=0.016). With the UB preload, only the intake of the test meal was reduced (P=0.044) but not the total energy intake (P=0.471) than the water. Fullness was also significantly increased after the PFB. In addition, postprandial glucose levels decreased and glucagon-like peptide-1 levels increased with the PFB compared with both the UB and water.
CONCLUSION
In healthy individuals, a premeal supplementation of PFB reduced total energy intake and decreased postprandial glucose excursion. This finding necessitates long-term studies regarding clinical use in obesity.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Letter: Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals (Diabetes Metab J 2019;43:879–92)
Mi-kyung Kim
Diabetes Metab J. 2020;44(1):203-204. doi: 10.4093/dmj.2020.0018.Response: Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals (Diabetes Metab J 2019;43:879–92)
Chang Ho Ahn, Jae Hyun Bae, Young Min Cho
Diabetes Metab J. 2020;44(1):207-208. doi: 10.4093/dmj.2020.0026.
Reference
-
1. GBD 2015 Obesity Collaborators. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, Salama JS, Vos T, Abate KH, Abbafati C, Ahmed MB, Al-Aly Z, Alkerwi A, Al-Raddadi R, Amare AT, Amberbir A, Amegah AK, Amini E, Amrock SM, Anjana RM, Arnlov J, Asayesh H, Banerjee A, Barac A, Baye E, Bennett DA, Beyene AS, Biadgilign S, Biryukov S, Bjertness E, Boneya DJ, Campos-Nonato I, Carrero JJ, Cecilio P, Cercy K, Ciobanu LG, Cornaby L, Damtew SA, Dandona L, Dandona R, Dharmaratne SD, Duncan BB, Eshrati B, Esteghamati A, Feigin VL, Fernandes JC, Fürst T, Gebrehiwot TT, Gold A, Gona PN, Goto A, Habtewold TD, Hadush KT, Hafezi-Nejad N, Hay SI, Horino M, Islami F, Kamal R, Kasaeian A, Katikireddi SV, Kengne AP, Kesavachandran CN, Khader YS, Khang YH, Khubchandani J, Kim D, Kim YJ, Kinfu Y, Kosen S, Ku T, Defo BK, Kumar GA, Larson HJ, Leinsalu M, Liang X, Lim SS, Liu P, Lopez AD, Lozano R, Majeed A, Malekzadeh R, Malta DC, Mazidi M, McAlinden C, McGarvey ST, Mengistu DT, Mensah GA, Mensink GBM, Mezgebe HB, Mirrakhimov EM, Mueller UO, Noubiap JJ, Obermeyer CM, Ogbo FA, Owolabi MO, Patton GC, Pourmalek F, Qorbani M, Rafay A, Rai RK, Ranabhat CL, Reinig N, Safiri S, Salomon JA, Sanabria JR, Santos IS, Sartorius B, Sawhney M, Schmidhuber J, Schutte AE, Schmidt MI, Sepanlou SG, Shamsizadeh M, Sheikhbahaei S, Shin MJ, Shiri R, Shiue I, Roba HS, Silva DAS, Silverberg JI, Singh JA, Stranges S, Swaminathan S, Tabares-Seisdedos R, Tadese F, Tedla BA, Tegegne BS, Terkawi AS, Thakur JS, Tonelli M, Topor-Madry R, Tyrovolas S, Ukwaja KN, Uthman OA, Vaezghasemi M, Vasankari T, Vlassov VV, Vollset SE, Weiderpass E, Werdecker A, Wesana J, Westerman R, Yano Y, Yonemoto N, Yonga G, Zaidi Z, Zenebe ZM, Zipkin B, Murray CJL. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017; 377:13–27. PMID: 28604169.2. Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011; 378:815–825. PMID: 21872750.
Article3. Bae JC. Trends of diabetes epidemic in Korea. Diabetes Metab J. 2018; 42:377–379. PMID: 30362303.
Article4. Choi SI, Chung D, Lim JS, Lee MY, Shin JY, Chung CH, Huh JH. Relationship between regional body fat distribution and diabetes mellitus: 2008 to 2010 Korean National Health and Nutrition Examination Surveys. Diabetes Metab J. 2017; 41:51–59. PMID: 28029016.
Article5. Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. International Agency for Research on Cancer Handbook Working Group. Body fatness and cancer: viewpoint of the IARC working group. N Engl J Med. 2016; 375:794–798. PMID: 27557308.6. Emerging Risk Factors Collaboration. Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, Sarwar N, Kizer JR, Lawlor DA, Nordestgaard BG, Ridker P, Salomaa V, Stevens J, Woodward M, Sattar N, Collins R, Thompson SG, Whitlock G, Danesh J. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011; 377:1085–1095. PMID: 21397319.7. Swinburn BA, Caterson I, Seidell JC, James WP. Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutr. 2004; 7:123–146. PMID: 14972057.8. Westerterp-Plantenga MS, Nieuwenhuizen A, Tome D, Soenen S, Westerterp KR. Dietary protein, weight loss, and weight maintenance. Annu Rev Nutr. 2009; 29:21–41. PMID: 19400750.
Article9. Pal S, Radavelli-Bagatini S. The effects of whey protein on cardiometabolic risk factors. Obes Rev. 2013; 14:324–343. PMID: 23167434.
Article10. Leidy HJ, Clifton PM, Astrup A, Wycherley TP, Westerterp-Plantenga MS, Luscombe-Marsh ND, Woods SC, Mattes RD. The role of protein in weight loss and maintenance. Am J Clin Nutr. 2015; 101:1320S–1329S. PMID: 25926512.
Article11. Akhavan T, Luhovyy BL, Brown PH, Cho CE, Anderson GH. Effect of premeal consumption of whey protein and its hydrolysate on food intake and postmeal glycemia and insulin responses in young adults. Am J Clin Nutr. 2010; 91:966–975. PMID: 20164320.
Article12. Giezenaar C, Trahair LG, Luscombe-Marsh ND, Hausken T, Standfield S, Jones KL, Lange K, Horowitz M, Chapman I, Soenen S. Effects of randomized whey-protein loads on energy intake, appetite, gastric emptying, and plasma gut-hormone concentrations in older men and women. Am J Clin Nutr. 2017; 106:865–877. PMID: 28747330.
Article13. Jakubowicz D, Froy O. Biochemical and metabolic mechanisms by which dietary whey protein may combat obesity and type 2 diabetes. J Nutr Biochem. 2013; 24:1–5. PMID: 22995389.
Article14. Konig D, Muser K, Berg A, Deibert P. Fuel selection and appetite-regulating hormones after intake of a soy protein-based meal replacement. Nutrition. 2012; 28:35–39. PMID: 21778035.
Article15. Papathanasopoulos A, Camilleri M. Dietary fiber supplements: effects in obesity and metabolic syndrome and relationship to gastrointestinal functions. Gastroenterology. 2010; 138:65–72.e1-2. PMID: 19931537.
Article17. Psichas A, Sleeth ML, Murphy KG, Brooks L, Bewick GA, Hanyaloglu AC, Ghatei MA, Bloom SR, Frost G. The short chain fatty acid propionate stimulates GLP-1 and PYY secretion via free fatty acid receptor 2 in rodents. Int J Obes (Lond). 2015; 39:424–429. PMID: 25109781.
Article18. Bae JH, Kim LK, Min SH, Ahn CH, Cho YM. Postprandial glucose-lowering effect of premeal consumption of protein-enriched, dietary fiber-fortified bar in individuals with type 2 diabetes mellitus or normal glucose tolerance. J Diabetes Investig. 2018; 9:1110–1118.
Article19. National Institute for Clinical Excellence. Type 2 diabetes: prevention in people at high risk. cited 2019 May 16. Available from: https://www.nice.org.uk/guidance/ph38.20. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013; 310:2191–2194. PMID: 24141714.21. Anderson GH, Tecimer SN, Shah D, Zafar TA. Protein source, quantity, and time of consumption determine the effect of proteins on short-term food intake in young men. J Nutr. 2004; 134:3011–3015. PMID: 15514267.
Article22. Bowen J, Noakes M, Clifton PM. Appetite regulatory hormone responses to various dietary proteins differ by body mass index status despite similar reductions in ad libitum energy intake. J Clin Endocrinol Metab. 2006; 91:2913–2919. PMID: 16735482.23. Baer DJ, Stote KS, Paul DR, Harris GK, Rumpler WV, Clevidence BA. Whey protein but not soy protein supplementation alters body weight and composition in free-living overweight and obese adults. J Nutr. 2011; 141:1489–1494. PMID: 21677076.
Article24. Mojtahedi MC, Thorpe MP, Karampinos DC, Johnson CL, Layman DK, Georgiadis JG, Evans EM. The effects of a higher protein intake during energy restriction on changes in body composition and physical function in older women. J Gerontol A Biol Sci Med Sci. 2011; 66:1218–1225. PMID: 21798863.
Article25. Bergmann JF, Chassany O, Petit A, Triki R, Caulin C, Segrestaa JM. Correlation between echographic gastric emptying and appetite: influence of psyllium. Gut. 1992; 33:1042–1043. PMID: 1398229.
Article26. Brown AJ, Goldsworthy SM, Barnes AA, Eilert MM, Tcheang L, Daniels D, Muir AI, Wigglesworth MJ, Kinghorn I, Fraser NJ, Pike NB, Strum JC, Steplewski KM, Murdock PR, Holder JC, Marshall FH, Szekeres PG, Wilson S, Ignar DM, Foord SM, Wise A, Dowell SJ. The orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J Biol Chem. 2003; 278:11312–11319. PMID: 12496283.
Article27. Kimura I, Ozawa K, Inoue D, Imamura T, Kimura K, Maeda T, Terasawa K, Kashihara D, Hirano K, Tani T, Takahashi T, Miyauchi S, Shioi G, Inoue H, Tsujimoto G. The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR43. Nat Commun. 2013; 4:1829. PMID: 23652017.
Article28. Ludwig DS, Pereira MA, Kroenke CH, Hilner JE, Van Horn L, Slattery ML, Jacobs DR Jr. Dietary fiber, weight gain, and cardiovascular disease risk factors in young adults. JAMA. 1999; 282:1539–1546. PMID: 10546693.
Article29. Thompson SV, Hannon BA, An R, Holscher HD. Effects of isolated soluble fiber supplementation on body weight, glycemia, and insulinemia in adults with overweight and obesity: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2017; 106:1514–1528. PMID: 29092878.
Article30. Johansson EV, Nilsson AC, Ostman EM, Bjorck IM. Effects of indigestible carbohydrates in barley on glucose metabolism, appetite and voluntary food intake over 16 h in healthy adults. Nutr J. 2013; 12:46. PMID: 23577719.
Article31. Kim EK, Oh TJ, Kim LK, Cho YM. Improving effect of the acute administration of dietary fiber-enriched cereals on blood glucose levels and gut hormone secretion. J Korean Med Sci. 2016; 31:222–230. PMID: 26839476.
Article32. King DG, Walker M, Campbell MD, Breen L, Stevenson EJ, West DJ. A small dose of whey protein co-ingested with mixed-macronutrient breakfast and lunch meals improves postprandial glycemia and suppresses appetite in men with type 2 diabetes: a randomized controlled trial. Am J Clin Nutr. 2018; 107:550–557. PMID: 29635505.
Article33. Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL, Wren AM, Brynes AE, Low MJ, Ghatei MA, Cone RD, Bloom SR. Gut hormone PYY(3-36) physiologically inhibits food intake. Nature. 2002; 418:650–654. PMID: 12167864.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter: Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals (Diabetes Metab J 2019;43:879–92)
- Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals
- Response: Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals (Diabetes Metab J 2019;43:879–92)
- Analysis of the Relationship between Dietary Fiber Intake & Food Habits in the Korean Adult Population: Using the 2001 Korean National Health and Nutrition Survey Data and the Newly Established Dietary Fiber Database
- Effect of Total Dietary Fiber on Bowel Habit and Bowel Transit in Healthy Subjects