Diabetes Metab J.
2013 Feb;37(1):63-71. 10.4093/dmj.2013.37.1.63.
Increased Selenoprotein P Levels in Subjects with Visceral Obesity and Nonalcoholic Fatty Liver Disease
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. medica7@gmail.com
- 2Department of Biostatistics, Korea University College of Medicine, Seoul, Korea.
- 3Department of Radiology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- KMID: 2280744
- DOI: http://doi.org/10.4093/dmj.2013.37.1.63
Abstract
- BACKGROUND
Selenoprotein P (SeP) has recently been reported as a novel hepatokine that regulates insulin resistance and systemic energy metabolism in rodents and humans. We explored the associations among SeP, visceral obesity, and nonalcoholic fatty liver disease (NAFLD).
METHODS
We examined serum SeP concentrations in subjects with increased visceral fat area (VFA) or liver fat accumulation measured with computed tomography. Our study subjects included 120 nondiabetic individuals selected from participants of the Korean Sarcopenic Obesity Study. In addition, we evaluated the relationship between SeP and cardiometabolic risk factors, including homeostasis model of insulin resistance (HOMA-IR), high sensitivity C-reactive protein (hsCRP), adiponectin values, and brachial-ankle pulse wave velocity (baPWV).
RESULTS
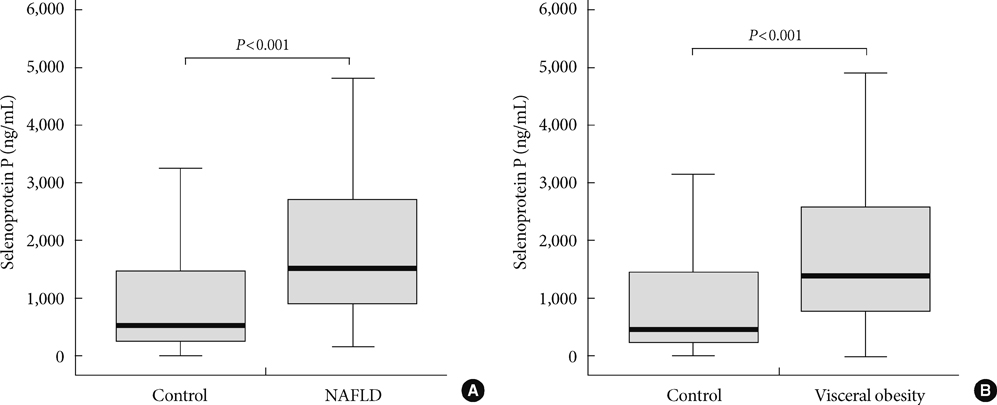
Subjects with NAFLD showed increased levels of HOMA-IR, hsCRP, VFA, and several components of metabolic syndrome and decreased levels of adiponectin and high density lipoprotein cholesterol than those of controls. Serum SeP levels were positively correlated with VFA, hsCRP, and baPWV and negatively correlated with the liver attenuation index. Not only subjects with visceral obesity but also those with NAFLD exhibited significantly increased SeP levels (P<0.001). In multiple logistic regression analysis, the subjects in the highest SeP tertile showed a higher risk for NAFLD than those in the lowest SeP tertile, even after adjusting for potential confounding factors (odds ratio, 7.48; 95% confidence interval, 1.72 to 32.60; P=0.007).
CONCLUSION
Circulating SeP levels were increased in subjects with NAFLD as well as in those with visceral obesity and may be a novel biomarker for NAFLD.
MeSH Terms
-
Adiponectin
C-Reactive Protein
Cholesterol
Cholesterol, HDL
Energy Metabolism
Fatty Liver
Homeostasis
Humans
Insulin Resistance
Intra-Abdominal Fat
Lipoproteins
Liver
Logistic Models
Obesity
Obesity, Abdominal
Pulse Wave Analysis
Risk Factors
Rodentia
Selenoprotein P
Selenoproteins
Adiponectin
C-Reactive Protein
Cholesterol
Cholesterol, HDL
Fatty Liver
Lipoproteins
Selenoprotein P
Selenoproteins
Figure
Cited by 1 articles
-
Exendin-4 Inhibits the Expression of SEPP1 and Fetuin-A via Improvement of Palmitic Acid-Induced Endoplasmic Reticulum Stress by AMPK
Jinmi Lee, Seok-Woo Hong, Se Eun Park, Eun-Jung Rhee, Cheol-Young Park, Ki-Won Oh, Sung-Woo Park, Won-Young Lee
Endocrinol Metab. 2015;30(2):177-184. doi: 10.3803/EnM.2015.30.2.177.
Reference
-
1. Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002. 346:1221–1231.2. Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care. 2000. 23:465–471.3. Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest. 2004. 114:1752–1761.4. Leclercq IA, Da Silva Morais A, Schroyen B, Van Hul N, Geerts A. Insulin resistance in hepatocytes and sinusoidal liver cells: mechanisms and consequences. J Hepatol. 2007. 47:142–156.5. Marra F, Bertolani C. Adipokines in liver diseases. Hepatology. 2009. 50:957–969.6. Vanni E, Bugianesi E, Kotronen A, De Minicis S, Yki-Jarvinen H, Svegliati-Baroni G. From the metabolic syndrome to NAFLD or vice versa? Dig Liver Dis. 2010. 42:320–330.7. Kim SG, Kim HY, Seo JA, Lee KW, Oh JH, Kim NH, Choi KM, Baik SH, Choi DS. Relationship between serum adiponectin concentration, pulse wave velocity and nonalcoholic fatty liver disease. Eur J Endocrinol. 2005. 152:225–231.8. Seo JA, Kim NH, Park SY, Kim HY, Ryu OH, Lee KW, Lee J, Kim DL, Choi KM, Baik SH, Choi DS, Kim SG. Serum retinol-binding protein 4 levels are elevated in non-alcoholic fatty liver disease. Clin Endocrinol (Oxf). 2008. 68:555–560.9. Stefan N, Hennige AM, Staiger H, Machann J, Schick F, Krober SM, Machicao F, Fritsche A, Haring HU. Alpha2-Heremans-Schmid glycoprotein/fetuin-A is associated with insulin resistance and fat accumulation in the liver in humans. Diabetes Care. 2006. 29:853–857.10. Dushay J, Chui PC, Gopalakrishnan GS, Varela-Rey M, Crawley M, Fisher FM, Badman MK, Martinez-Chantar ML, Maratos-Flier E. Increased fibroblast growth factor 21 in obesity and nonalcoholic fatty liver disease. Gastroenterology. 2010. 139:456–463.11. Burk RF, Hill KE. Selenoprotein P: an extracellular protein with unique physical characteristics and a role in selenium homeostasis. Annu Rev Nutr. 2005. 25:215–235.12. Misu H, Takamura T, Takayama H, Hayashi H, Matsuzawa-Nagata N, Kurita S, Ishikura K, Ando H, Takeshita Y, Ota T, Sakurai M, Yamashita T, Mizukoshi E, Honda M, Miyamoto K, Kubota T, Kubota N, Kadowaki T, Kim HJ, Lee IK, Minokoshi Y, Saito Y, Takahashi K, Yamada Y, Takakura N, Kaneko S. A liver-derived secretory protein, selenoprotein P, causes insulin resistance. Cell Metab. 2010. 12:483–495.13. Yang SJ, Hwang SY, Choi HY, Yoo HJ, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Serum selenoprotein P levels in patients with type 2 diabetes and prediabetes: implications for insulin resistance, inflammation, and atherosclerosis. J Clin Endocrinol Metab. 2011. 96:E1325–E1329.14. Zhang Y, Chen X. Reducing selenoprotein P expression suppresses adipocyte differentiation as a result of increased preadipocyte inflammation. Am J Physiol Endocrinol Metab. 2011. 300:E77–E85.15. Kim TN, Yang SJ, Yoo HJ, Lim KI, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Prevalence of sarcopenia and sarcopenic obesity in Korean adults: the Korean sarcopenic obesity study. Int J Obes (Lond). 2009. 33:885–892.16. Kim TN, Park MS, Yang SJ, Yoo HJ, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Prevalence and determinant factors of sarcopenia in patients with type 2 diabetes: the Korean Sarcopenic Obesity Study (KSOS). Diabetes Care. 2010. 33:1497–1499.17. Examination Committee of Criteria for 'Obesity Disease' in Japan. Japan Society for the Study of Obesity. New criteria for 'obesity disease' in Japan. Circ J. 2002. 66:987–992.18. Hubscher SG. Histological assessment of non-alcoholic fatty liver disease. Histopathology. 2006. 49:450–465.19. Limanond P, Raman SS, Lassman C, Sayre J, Ghobrial RM, Busuttil RW, Saab S, Lu DS. Macrovesicular hepatic steatosis in living related liver donors: correlation between CT and histologic findings. Radiology. 2004. 230:276–280.20. Yoo HJ, Park MS, Lee CH, Yang SJ, Kim TN, Lim KI, Kang HJ, Song W, Yeon JE, Baik SH, Choi DS, Choi KM. Cutoff points of abdominal obesity indices in screening for non-alcoholic fatty liver disease in Asians. Liver Int. 2010. 30:1189–1196.21. Kim SM, Lee J, Ryu OH, Lee KW, Kim HY, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Serum osteoprotegerin levels are associated with inflammation and pulse wave velocity. Clin Endocrinol (Oxf). 2005. 63:594–598.22. Moore JB. Non-alcoholic fatty liver disease: the hepatic consequence of obesity and the metabolic syndrome. Proc Nutr Soc. 2010. 69:211–220.23. Kantartzis K, Schick F, Haring HU, Stefan N. Environmental and genetic determinants of fatty liver in humans. Dig Dis. 2010. 28:169–178.24. Day CP, James OF. Steatohepatitis: a tale of two "hits"? Gastroenterology. 1998. 114:842–845.25. Hennige AM, Staiger H, Wicke C, Machicao F, Fritsche A, Haring HU, Stefan N. Fetuin-A induces cytokine expression and suppresses adiponectin production. PLoS One. 2008. 3:e1765.26. Reinehr T, Roth CL. Fetuin-A and its relation to metabolic syndrome and fatty liver disease in obese children before and after weight loss. J Clin Endocrinol Metab. 2008. 93:4479–4485.27. Zhang X, Yeung DC, Karpisek M, Stejskal D, Zhou ZG, Liu F, Wong RL, Chow WS, Tso AW, Lam KS, Xu A. Serum FGF21 levels are increased in obesity and are independently associated with the metabolic syndrome in humans. Diabetes. 2008. 57:1246–1253.28. Yilmaz Y, Eren F, Yonal O, Kurt R, Aktas B, Celikel CA, Ozdogan O, Imeryuz N, Kalayci C, Avsar E. Increased serum FGF21 levels in patients with nonalcoholic fatty liver disease. Eur J Clin Invest. 2010. 40:887–892.29. Guerrero R, Vega GL, Grundy SM, Browning JD. Ethnic differences in hepatic steatosis: an insulin resistance paradox? Hepatology. 2009. 49:791–801.30. Fracanzani AL, Valenti L, Bugianesi E, Andreoletti M, Colli A, Vanni E, Bertelli C, Fatta E, Bignamini D, Marchesini G, Fargion S. Risk of severe liver disease in nonalcoholic fatty liver disease with normal aminotransferase levels: a role for insulin resistance and diabetes. Hepatology. 2008. 48:792–798.31. Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005. 25:932–943.32. Choi KM, Lee KW, Seo JA, Oh JH, Kim SG, Kim NH, Choi DS, Baik SH. Relationship between brachial-ankle pulse wave velocity and cardiovascular risk factors of the metabolic syndrome. Diabetes Res Clin Pract. 2004. 66:57–61.33. Choi KM, Yoo HJ, Kim HY, Lee KW, Seo JA, Kim SG, Kim NH, Choi DS, Baik SH. Association between endogenous secretory RAGE, inflammatory markers and arterial stiffness. Int J Cardiol. 2009. 132:96–101.34. Blake GJ, Ridker PM. Novel clinical markers of vascular wall inflammation. Circ Res. 2001. 89:763–771.35. Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, Grimaldi A, Capron F, Poynard T. LIDO Study Group. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005. 128:1898–1906.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Increased Selenoprotein P Levels in Subjects with Visceral Obesity and Nonalcoholic Fatty Liver Disease
- Prevalence of the Nonalcoholic Fatty Liver Disease in Obese Children
- Hepatokines as a Link between Obesity and Cardiovascular Diseases
- Gut Microbiota and Clinical Disease: Obesity and Nonalcoholic Fatty Liver Disease
- Nonalcoholic Fatty Liver Disease