J Clin Neurol.
2006 Dec;2(4):272-275. 10.3988/jcn.2006.2.4.272.
Unilateral Epileptic Negative Myoclonus Following Focal Lesion of the Postcentral Cerebral Cortex Due to Acute Middle Cerebral Infarction
- Affiliations
-
- 1Department of Neurology, College of Medicine, The Catholic University of Korea, Korea. ks1007@catholic.ac.kr
- KMID: 1980469
- DOI: http://doi.org/10.3988/jcn.2006.2.4.272
Abstract
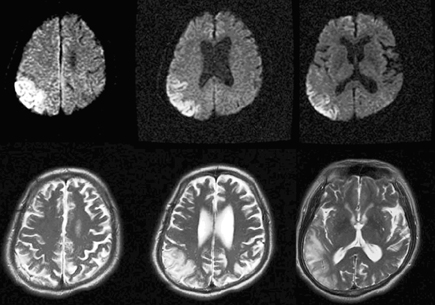
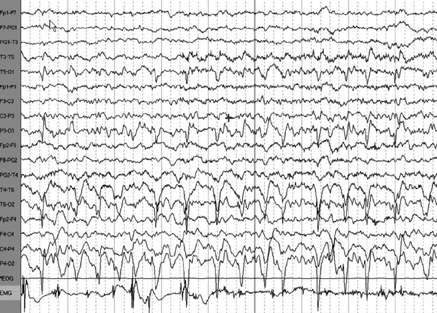
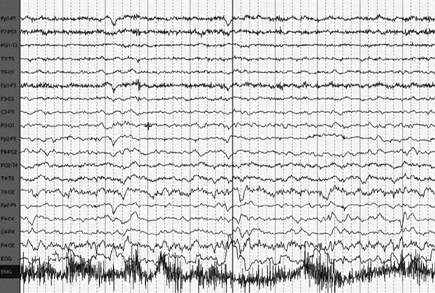
- Here we report a patient who suffered an acute infarction of the contralateral postcentral cerebral cortex and subsequently developed unilateral partial epilepsy with negative myoclonus. The findings of brain magnetic resonance imaging, polygraphic recordings of the postcentral somatosensory area, and response to anticonvulsant treatment support the presence of a cause-and-effect relationship, thereby providing evidence for a pathophysiological substrate for epileptic negative myoclonus.
MeSH Terms
Figure
Cited by 1 articles
-
Seizure Semiology: Its Value and Limitations in Localizing the Epileptogenic Zone
Krikor Tufenkjian, Hans O. Lüders
J Clin Neurol. 2012;8(4):243-250. doi: 10.3988/jcn.2012.8.4.243.
Reference
-
1. Noachtar S, Holthausen H, Lüders HO. Epileptic negative myoclonus. Subdural EEG recordings indicate a postcentral generator. Neurology. 1997. 49:1534–1537.
Article2. Shibasaki H. Fahn S, Hallett M, Luders HO, Marsden CD, editors. Pathophysiology of negative myoclonus and asterixis. Negative Motor Phenomena. 1995. Philadelphia: Lippincott-Raven;199–210.3. Rubboli G, Mai R, Meletti S, Francione S, Cardinale F, Tassi L, et al. Negative myoclonus induced by cortical electrical stimulation in epileptic patients. Brain. 2006. 129:65–81.
Article4. Guerrini R, Dravet C, Genton P, Bureau M, Roger J, Rubboli G, et al. Epileptic negative myoclonus. Neurology. 1993. 43(6):1078–1083.
Article5. Cirignotta F, Lugaresi E. Partial motor epilepsy with "negative myoclonus". Epilepsia. 1991. 32:54–58.
Article6. Ikeda A, Ohara S, Matsumoto R, Kunieda T, Nagamine T, Miyamoto S, et al. Role of primary sensorimotor cortices in generating inhibitory motor response in humans. Brain. 2000. 123:1710–1721.
Article7. Nighoghossian N, Trouillas P, Vial C, Froment JC. Unilateral upper limb asterixis related to primary motor cortex infarction. Stroke. 1995. 26:326–328.
Article8. Stell R, Davis S, Carroll WM. Unilateral asterixis due to a lesion of the ventrolateral thalamus. J Neurol Neurosurg Psychiatry. 1994. 57:878–880.
Article9. Young RR, Shahani BT. Asterixis: one type of negative myoclonus. Adv Neurol. 1986. 43:137–156.10. Lim SH, Dinner DS, Pillay PK, Lüders H, Morris HH, Klem G, et al. Functional anatomy of the human supplementary sensorimotor area: results of extraoperative electrical stimulation. Electroencephalogr Clin Neurophysiol. 1994. 91:179–193.
Article11. Young RR, Shahani BT. Anticonvulsant asterixis. Electroencephalogr Clin Neurophysiol. 1973. 34:760a.12. Rittmannsberger H. Asterixis induced by psychotropic drug treatment. Clin Neuropharmacol. 1996. 19:349–355.
Article13. Duarte J, Sempere AP, Cabezas MC, Marcos J, Claveria LE. Postural myoclonus induced by phenytoin. Clin Neuropharmacol. 1996. 19:536–538.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Cerebral Infarction in Carbon Monoxide Poisoning
- Cerebral Ptosis
- A Study of Effect of Recirculation in Experimental Cerebral Ischemia
- Distal anterior cerebral artery territory infarction caused by subfalcial herniation: CT findings
- Bilateral Periodic Limb Movement Disorder Developed after Anterior Cerebral Artery Infarction