Korean J Clin Neurophysiol.
2013 Dec;15(2):59-62. 10.14253/kjcn.2013.15.2.59.
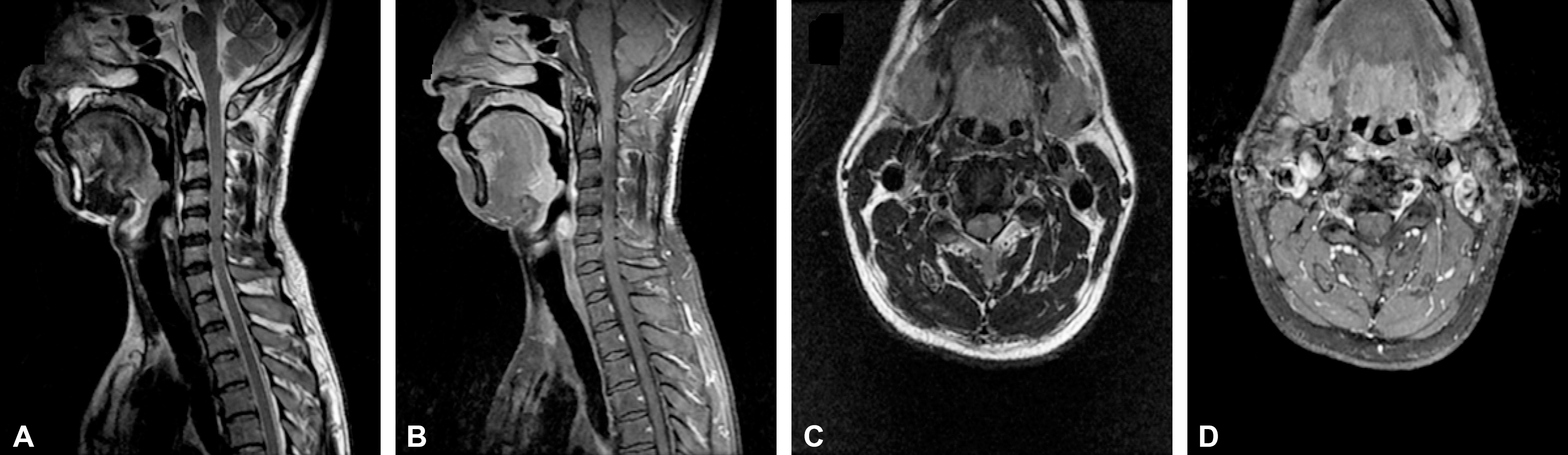
A Case of Man-in-the-Barrel Syndrome Induced by Cervical Spinal Cord Ischemia
- Affiliations
-
- 1Department of Neurology, Dong-A University College of Medicine, Busan, Korea. advania9@chol.com
- 2Department of Radiology, Dong-A University College of Medicine, Busan, Korea.
- KMID: 1863275
- DOI: http://doi.org/10.14253/kjcn.2013.15.2.59
Abstract
- Man-in-the-barrel syndrome (MIBS) is a clinical syndrome of bilateral upper limb weakness with normal lower extremity function. It can be caused by various neurological conditions such as bilateral cerebral hypoperfusion, syringomyelia, motor neuron disease, or cervical myelopathies. We report a patient with MIBS after cervical spinal cord ischemia. It is postulated to be caused by ischemic insults of anterior spinal artery from repeated and prolonged neck extension.
MeSH Terms
Figure
Cited by 1 articles
-
Two Cases of ‘Man-in-the-Barrel’ Syndrome Caused by Cerebral Hypoperfusion and Hypoxia
Jonguk Kim, Seung Hun Oh, Ok Joon Kim
J Neurocrit Care. 2015;8(1):30-34. doi: 10.18700/jnc.2015.8.1.30.
Reference
-
1.Orsini M., Catharino AM., Catharino FM., Mello MP., Freitas MR., Leite MA, et al. Man-in-the-barrel syndrome, a symmetrical proximal brachial amyotrophic diplegia related to motor neuron diseases: a survey of nine cases. Rev Assoc Med Bras. 2009. 55:712–715.
Article2.Crisostomo EA., Suslavich FJ. Man-in-the-barrel syndrome associated with closed head injury. J Neuroimaging. 1994. 4:116–117.
Article3.Vainstein G., Gordon CR., Gadoth N. HTLV-1 associated motor neuron disease mimicking “Man-in-the-Barrel” syndrome. J Clin Neuromuscul Dis. 2005. 6:127–131.
Article4.Sage JI., Van Uitert RL. Man-in-the-barrel syndrome. Neurology. 1986. 36:1102–1103.
Article5.Berg D., Mullges W., Koltzenburg M., Bendszus M., Reiners K. Man-in-the-barrel syndrome caused by cervical spinal cord infarction. Acta Neurol Scand. 1998. 97:417–419.6.Schneider RC., Cherry G., Pantek H. The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine. J Neurosurg. 1954. 11:546–577.7.Ben Sassi S., El Euch G., Regaieg A., Mabrouk T., Zouari M., Ben Romdhane N, et al. Man-in-the-barrel syndrome with combination of infarctions in the anterior spinal artery and posterior inferior cerebellar artery territories. Cerebrovasc Dis. 2009. 27:201–202.
Article8.Piao YS., Lu DH., Su YY., Yang XP. Anterior spinal cord infarction caused by fibrocartilaginous embolism. Neuropathology. 2009. 29:172–175.
Article9.Han JJ., Massagli TL., Jaffe KM. Fibrocartilaginous embolism-an uncommon cause of spinal cord infarction: a case report and review of the literature. Arch Phys Med Rehabil. 2004. 85:153–157.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertebral Artery Dissection Presenting with Acute Infarction in Cervical Spinal Cord and Cerebellum
- Monoplegia after Anterior Cervical Discectomy and Fusion: A Case Report
- Acute Rhabdomyolysis and Ischemia of the Spinal Cord Following the Heavy Alcohol Ingestion: A case report
- Cervical Spinal Cord Infarction Presenting as Chest Pain in Patients with Acute Cerebellar Infarction
- Myelopathy Caused by Surfing