Elevated Serum Homocysteine Levels Were Not Correlated with Serum Uric Acid Levels, but with Decreased Renal Function in Gouty Patients
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea. drsong@cau.ac.kr
- KMID: 1796940
- DOI: http://doi.org/10.3346/jkms.2014.29.6.788
Abstract
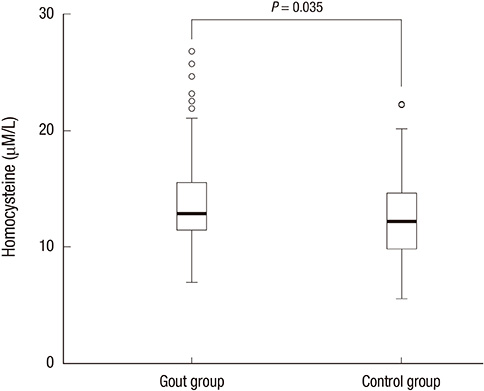
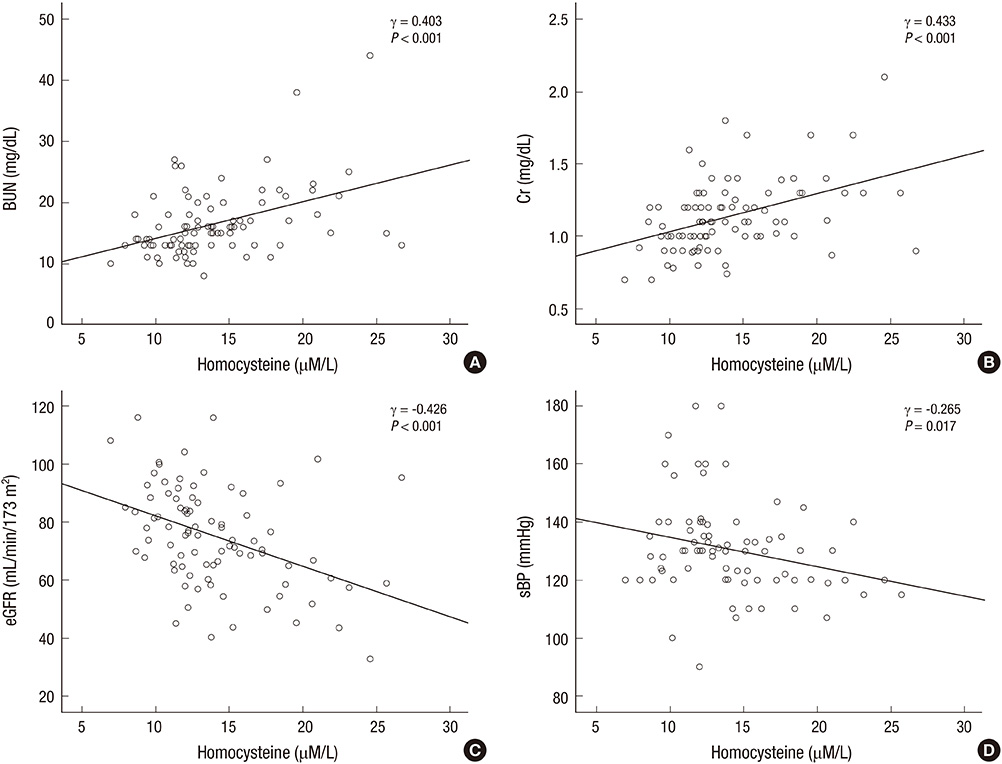
- Hyperhomocysteinemia is one of the important factors of the cardiovascular disease, and gout is well known to be associated with cardiovascular disease. There are a few reports on the serum homocysteine (Hcy) levels in patients with gout, however, the results showed discrepancies. In this study, we measured Hcy levels in patients with gout and examined factors associated with the levels of serum Hcy. Ninety-one male patients with gout and 97 age-matched healthy male controls were enrolled in the study. Serum uric acid levels were not significantly different between gout and healthy control groups. However, serum Hcy levels were significantly higher in patients with gout compared to controls (13.96+/-4.05 microM/L vs 12.67+/-3.52 microM/L, P=0.035). In gout group, patients with 1-2 stages of chronic kidney disease (CKD) had significantly lower serum Hcy than those with 3-5 stages of CKD (13.15+/-3.46 microM/L vs 17.45+/-4.68 microM/L, P<0.001). Multivariate linear analysis revealed an inverse association between serum Hcy and estimated glomerular filtration rate (eGFR) (beta=-0.107, P<0.001). In conclusion, serum Hcy was elevated in male patients with gout. Hyperhomocysteinemia was not correlated with serum uric acid, but it was inversely associated with impaired renal function.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Increased Carotid Intima-Media Thickness (IMT) in Hyperuricemic Individuals May Be Explained by Hyperhomocysteinemia Associated with Renal Dysfunction: a Cross-Sectional Study
Ji Ho Park, Jung Soo Song, Sang Tae Choi
J Korean Med Sci. 2019;34(37):. doi: 10.3346/jkms.2019.34.e237.Two-year Follow-up Study of the Relationship between the Changes of Serum Homocysteine and Those of Serum Uric Acid Levels, Lipid Profiles and Renal Function in Gout Patients
Eun Hye Park, Ji Ho Park, Jung-Soo Song, Sang Tae Choi
J Rheum Dis. 2016;23(1):30-36. doi: 10.4078/jrd.2016.23.1.30.The Relationship between Uric Acid and Homocysteine Levels based on Alcohol-related Facial Flushing
Eo Chin Kim, Jong Sung Kim, Won Chul Uh, Soo Young Choi, Sun Kyung Lee, Bog Seon Jeong
Korean J Health Promot. 2015;15(3):91-97. doi: 10.15384/kjhp.2015.15.3.91.
Reference
-
1. Rakieh C, Conaghan PG. Diagnosis and treatment of gout in primary care. Practitioner. 2011; 255:17–20.2. Choi HK, Curhan G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation. 2007; 116:894–900.3. Krishnan E, Svendsen K, Neaton JD, Grandits G, Kuller LH. MRFIT Research Group. Long-term cardiovascular mortality among middle-aged men with gout. Arch Intern Med. 2008; 168:1104–1110.4. Krishnan E. Inflammation, oxidative stress and lipids: the risk triad for atherosclerosis in gout. Rheumatology (Oxford). 2010; 49:1229–1238.5. Tomita M, Mizuno S, Yamanaka H, Hosoda Y, Sakuma K, Matuoka Y, Odaka M, Yamaguchi M, Yosida H, Morisawa H, et al. Does hyperuricemia affect mortality? a prospective cohort study of Japanese male workers. J Epidemiol. 2000; 10:403–409.6. Fessel WJ. High uric acid as an indicator of cardiovascular disease: independence from obesity. Am J Med. 1980; 68:401–404.7. Niskanen LK, Laaksonen DE, Nyyssönen K, Alfthan G, Lakka HM, Lakka TA, Salonen JT. Uric acid level as a risk factor for cardiovascular and all-cause mortality in middle-aged men: a prospective cohort study. Arch Intern Med. 2004; 164:1546–1551.8. Petri M, Roubenoff R, Dallal GE, Nadeau MR, Selhub J, Rosenberg IH. Plasma homocysteine as a risk factor for atherothrombotic events in systemic lupus erythematosus. Lancet. 1996; 348:1120–1124.9. McCully KS, Wilson RB. Homocysteine theory of arteriosclerosis. Atherosclerosis. 1975; 22:215–227.10. Eikelboom JW, Hankey GJ. Associations of homocysteine, C-reactive protein and cardiovascular disease in patients with renal disease. Curr Opin Nephrol Hypertens. 2001; 10:377–383.11. Slot O. Homocysteine, a marker of cardiovascular disease risk, is markedly elevated in patients with gout. Ann Rheum Dis. 2013; 72:457.12. Istok R, Kovalancík M, Rovenský J. Total plasma homocysteine in patients with gout. J Rheumatol. 1999; 26:2068–2069.13. Cheng TT, Lai HM, Chang HW, Luo SF. Elevated serum homocysteine levels for gouty patients. Clin Rheumatol. 2005; 24:103–106.14. Tsutsumi Z, Moriwaki Y, Yamamoto T, Takahashi S, Hada T, Fukuchi M. Total plasma homocysteine is not increased in Japanese patients with gout. J Rheumatol. 2002; 29:1805–1806.15. Wallace SL, Robinson H, Masi AT, Decker JL, McCarty DJ, Yü TF. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977; 20:895–900.16. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation: Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999; 130:461–470.17. Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, Gansevoort RT, Kasiske BL, Eckardt KU. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011; 80:17–28.18. Petriş A, Cimpoeşu D, Petriş O, Costache I. Uric acid, cardiovascular events and renal dysfunction: a circumstantial connection? Rev Med Chir Soc Med Nat Iasi. 2012; 116:407–412.19. Rolland PH, Friggi A, Barlatier A, Piquet P, Latrille V, Faye MM, Guillou J, Charpiot P, Bodard H, Ghiringhelli O, et al. Hyperhomocysteinemia-induced vascular damage in the minipig: captopril-hydrochlorothiazide combination prevents elastic alterations. Circulation. 1995; 91:1161–1174.20. Tsai JC, Perrella MA, Yoshizumi M, Hsieh CM, Haber E, Schlegel R, Lee ME. Promotion of vascular smooth muscle cell growth by homocysteine: a link to atherosclerosis. Proc Natl Acad Sci U S A. 1994; 91:6369–6373.21. Ferechide D, Radulescu D. Hyperhomocysteinemia in renal diseases. J Med Life. 2009; 2:53–59.22. Nashar K, Fried LF. Hyperuricemia and the progression of chronic kidney disease: is uric acid a marker or an independent risk factor? Adv Chronic Kidney Dis. 2012; 19:386–391.23. Marwah RK. Comorbidities in gouty arthritis. J Investig Med. 2011; 59:1211–1220.24. Feng SQ, Ye P, Luo LM, Xiao WK, Xu RY, Wu HM. Relationship between serum homocysteine and metabolic syndrome: a cross-sectional study. Zhonghua Liu Xing Bing Xue Za Zhi. 2012; 33:256–259.25. Daly C, Fitzgerald AP, O'Callaghan P, Collins P, Cooney MT, Graham IM. COMAC Group. Homocysteine increases the risk associated with hyperlipidaemia. Eur J Cardiovasc Prev Rehabil. 2009; 16:150–155.26. Mikuls TR, Farrar JT, Bilker WB, Fernandes S, Schumacher HR Jr, Saag KG. Gout epidemiology: results from the UK General Practice Research Database, 1990-1999. Ann Rheum Dis. 2005; 64:267–272.27. Hak AE, Curhan GC, Grodstein F, Choi HK. Menopause, postmenopausal hormone use and risk of incident gout. Ann Rheum Dis. 2010; 69:1305–1309.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two-year Follow-up Study of the Relationship between the Changes of Serum Homocysteine and Those of Serum Uric Acid Levels, Lipid Profiles and Renal Function in Gout Patients
- The Relationship between Homocysteine and Uric Acid Levels in Gouty Patients
- Change in Plasma Homocysteine Concentration during the Recovery Phase of Renal Transplantation
- Serum Levels of Homocysteine, Folate, and Vitamin B12 and Cognitive Function in Mild Cognitive Impairment and Alzheimer's Disease
- Sonographic Findings in Gouty Nephropathy