Korean J Gastroenterol.
2011 Jun;57(6):374-378. 10.4166/kjg.2011.57.6.374.
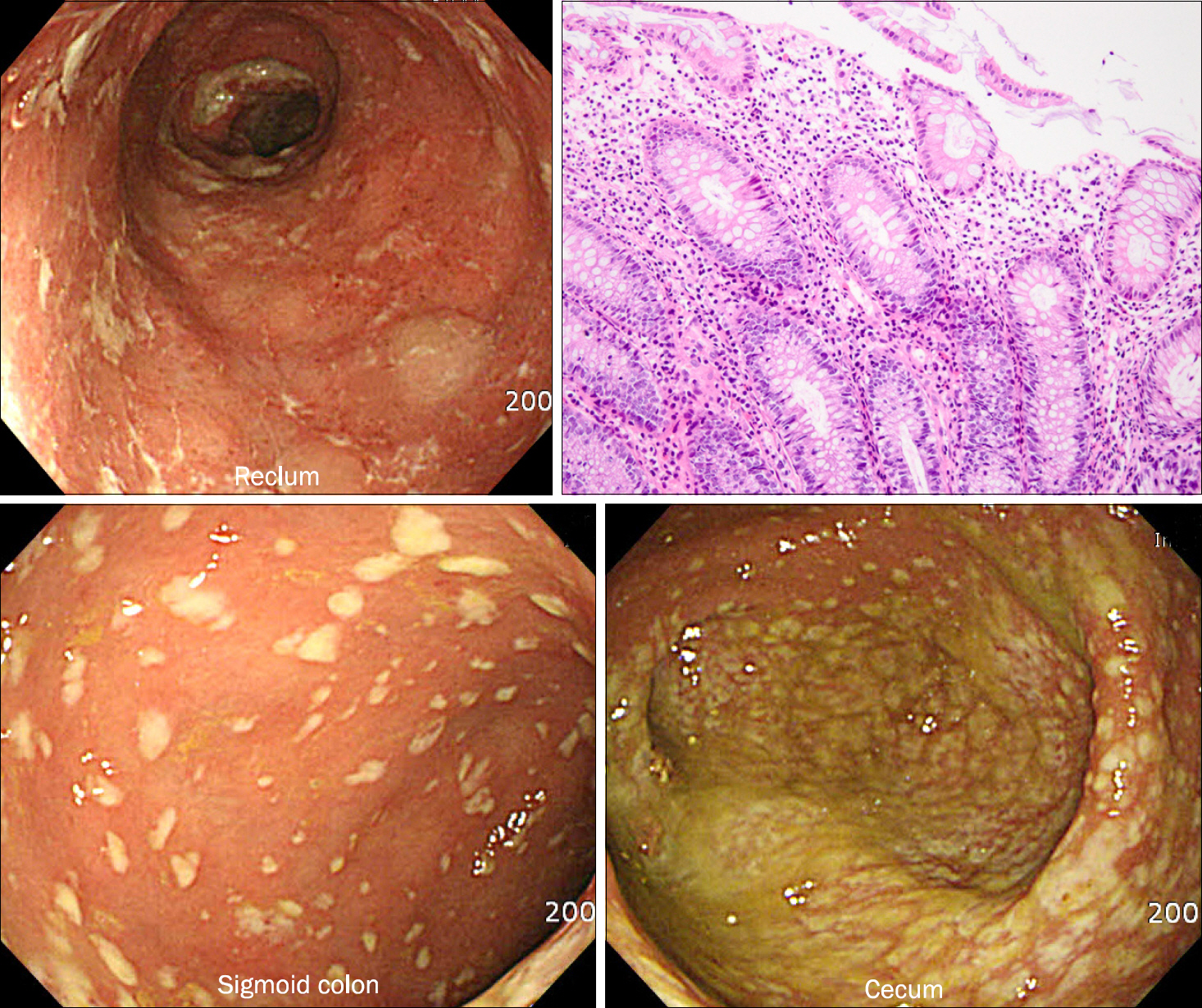
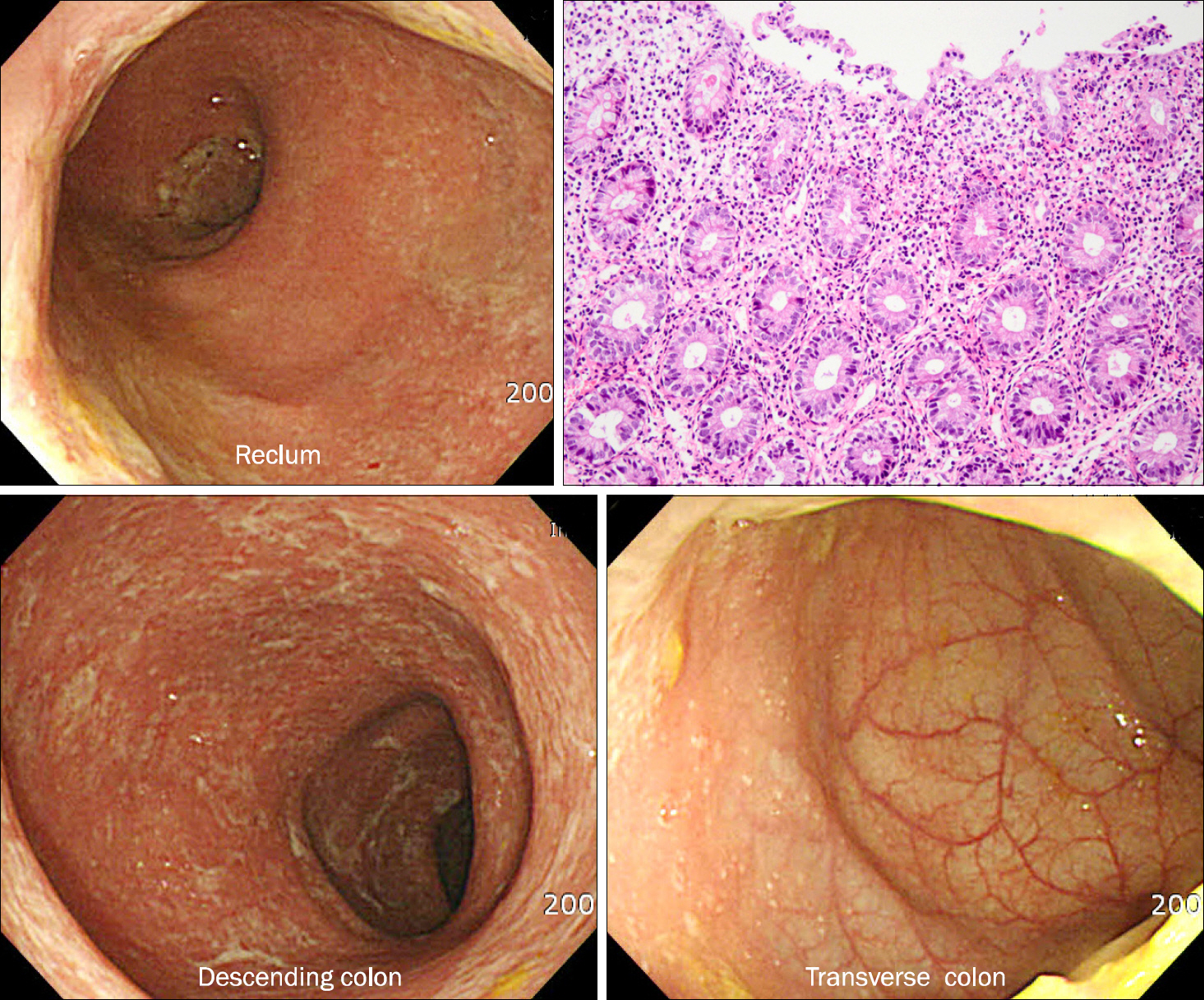
Left-sided Ulcerative Colitis Reactivated and Aggravated during Clostridium difficile Infection
- Affiliations
-
- 1Department of Medicine, Hallym University College of Medicine, Seoul, Korea. jbkim87@hallym.or.kr
- KMID: 1792803
- DOI: http://doi.org/10.4166/kjg.2011.57.6.374
Abstract
- Clostridium difficile (C. difficile) infection appears to be closely related to reactivation, diagnostic delay, and disease progression in patients with inflammatory bowel disease. However, whether C. difficile infection triggers the reactivation of inflammatory bowel disease or vice versa is not certain. We report a case of reactivated and progressed left ulcerative colitis following C. difficile infection in a 56-year-old woman. A series of endoscopic findings in this case report strongly supports a causative role of C. difficile infection on the reactivation and progression of ulcerative colitis.
Figure
Reference
-
References
1. Kethu SR. Extraintestinal manifestations of inflammatory bowel diseases. J Clin Gastroenterol. 2006; 40:467–475.
Article2. Satsangi J, Jewell DP, Bell JI. The genetics of inflammatory bowel disease. Gut. 1997; 40:572–574.
Article3. Bolton RP, Sherriff RJ, Read AE. Clostridium difficle associated diarrhea: a role in inflammatory bowel disease? Lancet. 1980; 1:383–384.4. Meyers S, Mayer L, Bottone E, Desmond E, Janowitz HD. Occurrence of Clostridium difficile toxin during the course of inflammatory bowel disease. Gastroenterology. 1981; 80:697–700.5. Meyer AM, Ramzan NN, Loftus EV Jr, Heigh RI, Leighton JA. The diagnostic yield of stool pathogen studies during relapses of inflammatory bowel disease. J Clin Gastroenterol. 2004; 38:772–775.
Article6. Mylonaki M, Langmead L, Pantes A, Johnson F, Rampton DS. Enteric infection in relapse of inflammatory bowel disease: im-portance of microbiological examination of stool. Eur J Gastroenterol Hepatol. 2004; 16:775–778.7. Issa M, Vijayapal A, Graham MB, et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007; 5:345–351.8. Ananthakrishnan AN, McGinley EL, Binion DG. Excess hospital-isation burden associated with Clostridium difficile in patients with inflammatory bowel disease. Gut. 2008; 57:205–210.9. Rodemann JF, Dubberk ER, Reske KA, Seo da H, Stone CD. Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007; 5:339–344.10. Issa M, Ananthakrishnan AN, Binion DG. Clostridium difficile and inflammatory bowel disease. Inflamm Bowel Dis. 2008; 14:1432–1442.11. Miller DL, Sedlack JD, Holt RW. Perforation complicating ri-fampin-associated pseudomembranous enteritis. Arch Surg. 1989; 124:1082.
Article12. Wang A, Takeshima F, Ikeda M, et al. Ulcerative colitis complicating pseudomembranous colitis of the right colon. J Gastroenterol. 2002; 37:309–312.
Article13. Hookman P, Barkin JS. Clostridium difficile associated infection, diarrhea and colitis. World J Gastroenterol. 2009; 15:1554–1580.14. Bartlett JG. Clinical practice. Antibiotic-associated diarrhea. N Engl J Med. 2002; 346:334–339.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of Clostridium difficile colitis
- A Case of Reactive Arthritis in a Patient with Clostridium Difficile Diarrhea
- Clostridium difficile Infection: A Worldwide Disease
- Toxic Megacolon Associated with Secondary Amyloidosis: An Unusual Complication of Clostridium difficile Colitis
- Diagnosis of Clostridium difficile-associated diarrhea