J Korean Med Sci.
2008 Feb;23(1):66-71. 10.3346/jkms.2008.23.1.66.
Acute Effects of Asian Dust Events on Respiratory Symptoms and Peak Expiratory Flow in Children with Mild Asthma
- Affiliations
-
- 1Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea.
- 2Department of Pediatrics, Dongguk University International Hospital, Goyang, Korea.
- 3Department of Pediatrics, Seoul National University Hospital, Seoul, Korea. kohyy@plaza.snu.ac.kr
- KMID: 1786847
- DOI: http://doi.org/10.3346/jkms.2008.23.1.66
Abstract
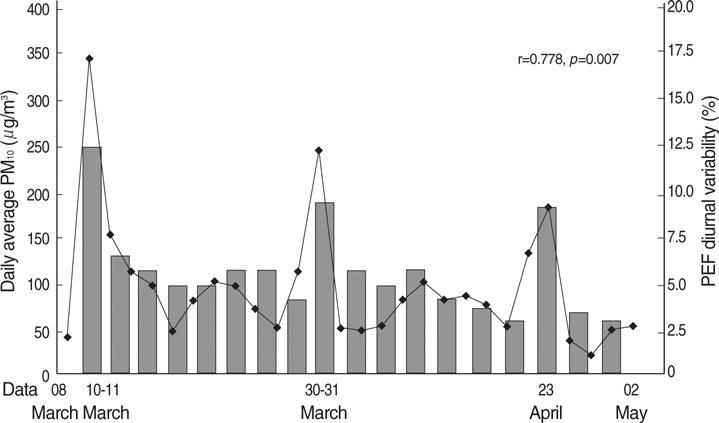
- The aim of this study was to investigate the possible adverse effects of Asian dust events on respiratory health in asthmatic children. Fifty-two children with mild asthma were studied for eight consecutive weeks in the spring of 2004 (March 8 to May 2). During the study period, five Asian dust days were identified; we included a lag period of two days following each of the events. Subjects recorded their respiratory symptom diaries and peak expiratory flow (PEF) twice daily during the study period; and they underwent methacholine bronchial challenge tests. The subjects reported a significantly higher frequency of respiratory symptoms during the Asian dust days than during the control days. They showed significantly more reduced morning and evening PEF values, and more increased PEF variability (10.1%+/-3.5% vs. 5.5%+/-2.2%) during the Asian dust days than during the control days. Methacholine PC20 was not significantly different between before and after the study period (geometric mean: 2.82 mg/mL vs. 3.16 mg/mL). These results suggest that the short-term Asian dust events might be associated with increased acute respiratory symptoms and changes in PEF outcomes. However, there might be little long-term influence on airway hyperresponsiveness in children with mild asthma.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Toxicity and health effects of Asian dust: a literature review
Ho-Jang Kwon
J Korean Med Assoc. 2012;55(3):234-242. doi: 10.5124/jkma.2012.55.3.234.Toxicity and health effects of Asian dust: a literature review
Ho-Jang Kwon
J Korean Med Assoc. 2012;55(3):234-242. doi: 10.5124/jkma.2012.55.3.234.Air pollution and childhood allergic disease
Young Yoo
Allergy Asthma Respir Dis. 2016;4(4):248-256. doi: 10.4168/aard.2016.4.4.248.
Reference
-
1. Kwon HJ, Cho SH, Chun Y, Lagarde F, Pershagen G. Effects of the Asian dust events on daily mortality in Seoul, Korea. Environ Res. 2002. 90:1–5.
Article2. Hwang SS, Cho SH, Kwon HJ. Effects of the severe Asian dust events on daily mortality during the spring of 2002, in Seoul, Korea. J Prev Med Pub Health. 2005. 38:197–202.3. Schwartz J, Dockery DW, Neas LM, Wypij D, Ware JH, Spengler JD, Koutrakis P, Speizer FE, Ferris BG Jr. Acute effects of summer air pollution on respiratory symptom reporting in children. Am J Respir Crit Care Med. 1994. 150:1234–1242.
Article4. Vedal S, Petkau J, White R, Blair J. Acute effects of ambient inhalable particles in asthmatic and nonasthmatic children. Am J Respir Crit Care Med. 1998. 157:1034–1043.
Article5. Preutthipan A, Udomsubpayakul U, Chaisupamongkollarp T, Pentamwa P. Effect of PM10 pollution in Bangkok on children with and without asthma. Pediatr Pulmonol. 2004. 37:187–192.6. Park JW, Lim YH, Kyung SY, An CH, Lee SP, Jeong SH, Ju YS. Effects of ambient particulate matter on peak expiratory flow rates and respiratory symptoms of asthmatics during Asian dust periods in Korea. Respirology. 2005. 10:470–476.
Article7. Reddel HK, Salome CM, Peat JK, Woolcock AJ. Which index of peak expiratory flow is most useful in the management of stable asthma? Am J Respir Crit Care Med. 1995. 151:1320–1325.
Article8. National Asthma Education and Prevention Program. Guidelines for the diagnosis and management of asthma expert panel. Report 2. 1997. Bethesda, Md: US Dept of Health and Human Services;NIH publication 97-4051.9. Chai H, Farr RS, Froehlich LA, Mathison DA, McLean JA, Rosenthal RR, Sheffer AL, Spector SL, Townley RG. Standardization of bronchial inhalation challenge procedures. J Allergy Clin Immunol. 1975. 56:323–327.
Article10. Romieu I, Meneses F, Ruiz S, Huerta J, Sienra JJ, White M, Etzel R, Hernandez M. Effects of intermittent ozone exposure on peak expiratory flow and respiratory symptoms among asthmatic children in Mexico City. Arch Environ Health. 1997. 52:368–376.
Article11. Ostro B, Lipsett M, Mann J, Braxton-Owens H, White M. Air pollution and exacerbation of asthma in African-American children in Los Angeles. Epidemiology. 2001. 12:200–208.12. Park JW, Lim YH, Kyung SY, An CH, Lee SP, Jeong SH, Ju YS. Effects of ambient particulate matter (PM10) on peak expiratory flow and respiratory symptoms in subjects with bronchial asthma during Yellow Sand period. Tubercul Respir Dis. 2003. 55:570–578.13. Min PK, Kim CW, Yun YJ, Chang JH, Chu JK, Lee KE, Han JY, Park JW, Hong CS. Effect of Yellow Sand on respiratory symptoms and diurnal variation of peak expiratory flow in patients with bronchial asthma. J Asthma Allergy Clin Immunol. 2001. 21:1179–1186.14. Hakala K, Stenius-Aarniala B, Sovijarvi A. Effects of weight loss on peak flow variability, airways obstruction, and lung volumes in obese patients with asthma. Chest. 2000. 118:1315–1321.
Article15. Barnes PJ. A new approach to the treatment of asthma. N Engl J Med. 1989. 321:1517–1527.
Article16. Lei YC, Chan CC, Wang PY, Lee CT, Cheng TJ. Effects of Asian dust event particles on inflammation markers in peripheral blood and bronchoalveolar lavage in pulmonary hypertensive rats. Environ Res. 2004. 95:71–76.
Article17. Choi JC, Lee MH, Chun YS, Kim J, Oh S. Chemical composition and source signature of spring aerosol in Seoul Korea. J Geophys Res. 2001. 106:18067–18074.
Article18. Blomberg A, Krishna MT, Bocchino V, Biscione GL, Shute JK, Kelly FJ, Frew AJ, Holgate ST, Sandstrom T. The inflammatory effects of 2 ppm NO2 on the airways of healthy subjects. Am J Respir Crit Care Med. 1997. 156:418–424.19. Burnett RT, Smith-Doiron M, Stieb D, Raizenne ME, Brook JR, Dales RE, Leech JA, Cakmak S, Krewski D. Association between ozone and hospitalization for acute respiratory diseases in children less than 2 years of age. Am J Epidemiol. 2001. 153:444–452.
Article20. Ward DJ, Ayres JG. Particulate air pollution and panel studies in children: a systemic review. Occup Environ med. 2004. 61:e13.21. Krzyzanowski M, Quackenboss JJ, Lebowitz MD. Relation of peak expiratory flow rates and symptoms to ambient ozone. Arch Environ Health. 1992. 47:107–115.
Article22. Romieu I, Meneses F, Ruiz S, Sienra JJ, Huerta J, White MC, Etzel RA. Effects of air pollution on the respiratory health of asthmatic children living in Mexico City. Am J Respir Crit Care Med. 1996. 154:300–307.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Specific Immunotherapy with House Dust Mite AIleI-gen in ChiIdhood Asthma
- Effects of Ambient Particulate Matter(PM10) on Peak Expiratory Flow and Respiratory Symptoms in Subjects with Bronchial Asthma During Yellow Sand Period
- A study of predicted values of peak expiratory flow rates in primary school children
- Effect of Yellow sand on respiratory symptoms and diurnal variation of peak expiratory flow in patients with bronchial asthma
- The association of forced expiratory volume in one second and forced expiratory flow at 50% of the vital capacity, peak expiratory flow parameters, and blood eosinophil counts in exercise-induced bronchospasm in children with mild asthma