Korean J Radiol.
2005 Mar;6(1):44-46. 10.3348/kjr.2005.6.1.44.
MR Imaging of Pregnancy Luteoma: a Case Report and Correlation with the Clinical Features
- Affiliations
-
- 1Department of Radiology, Tri-Service General Hospital, National Defense Medical Center, Korea. cohi.meow@msa.hinet.net
- 2Department of Obstetrics and Gynecology, Tri-Service General Hospital, National Defense Medical Center, Korea.
- 3Department of Pediatrics, Tri-Service General Hospital, National Defense Medical Center, Korea.
- KMID: 1783173
- DOI: http://doi.org/10.3348/kjr.2005.6.1.44
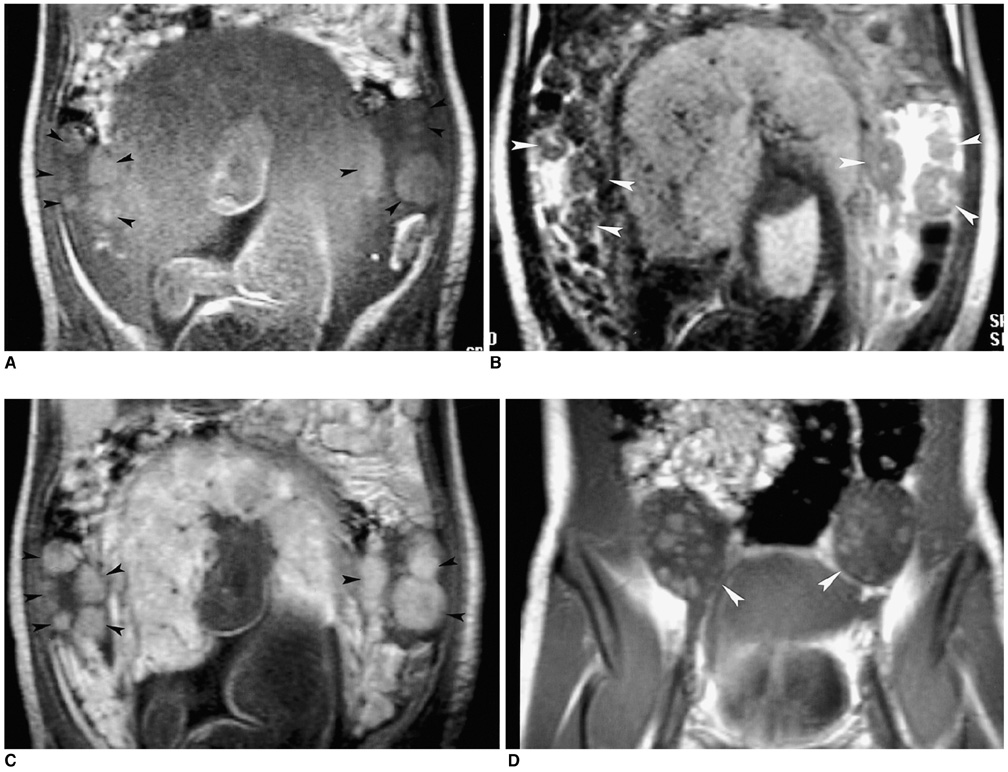
Abstract
- We report here on a 26-year-old pregnant female who developed hirsutism and virilization during her third trimester along with a significantly elevated serum testosterone level. Abdominal US and MR imaging studies were performed, and they showed unique imaging features that may suggest the diagnosis of pregnancy luteoma in the clinical context. After the delivery, the serum testosterone level continued to decrease, and it returned to normal three weeks postpartum. The follow-up imaging findings were closely correlated with the clinical presentation.
Keyword
MeSH Terms
-
Adult
Contrast Media
Diagnosis, Differential
Female
Gadolinium DTPA/diagnostic use
Hirsutism/etiology
Humans
Luteoma/complications/*diagnosis
Magnetic Resonance Imaging
Ovarian Neoplasms/complications/*diagnosis
Pregnancy
Pregnancy Complications, Neoplastic/*diagnosis
Pregnancy Outcome
Ultrasonography, Prenatal
Virilism/etiology
Figure
Reference
-
1. Sternberg WH, Barclay DL. Luteoma of pregnancy. Am J Obstet Gynecol. 1966. 95:165–184.2. Young RH, Dudley AG, Scully RE. Granulosa cell, Sertoli-Leydig cell, and unclassified sex cord-stromal tumors associated with pregnancy: a clinicopathological analysis of thirty-six cases. Gynecol Oncol. 1984. 18:181–205.3. Forest MG, Orgiazzi J, Tranchant D, Mornex R, Bertrand J. Approach to the mechanism of androgen overproduction in a case of Krukenbery tumor responsible for virilization during pregnancy. J Clin Endocrinol Metab. 1978. 47:428–434.4. Pascal RR, Grecco LA. Mucinous cystadenoma of the ovary with stromal luteinization and hilar cell hyperplasia during pregnancy. Hum Pathol. 1988. 19:179–180.5. Garcia-Bunuel R, Berek JS, Woodruff JD. Luteomas of pregnancy. Obstet Gynecol. 1975. 45:407–414.6. Clement PB. Tumor-like lesions of the ovary associated with pregnancy. Int J Gynecol Pathol. 1993. 12:108–115.7. Tinkanen H, Kuoppala T. Virilization during pregnancy caused by ovarian mucinous cystadenocarcinoma. Acta Obstet Gynecol Scand. 2001. 80:476–477.8. Joshi R, Dunaif A. Ovarian disorders of pregnancy. Endocrinol Metab Clin North Am. 1995. 24:153–169.9. Wang HK, Sheu MH, Guo WY, Hong CH, Chang CY. Magnetic resonance imaging of pregnancy luteoma. J Comput Assist Tomogr. 2003. 27:155–157.10. Ha HK, Baek SY, Kim SH, Kim HH, Chung EC, Yeon KM. Krukenberg's tumor of the ovary: MR imaging features. AJR Am J Roentgenol. 1995. 164:1435–1439.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pregnancy Luteoma of the Ovary in a Primiparous Woman: A case report
- Unusual Course of Acne Conglobata as a Skin Manifestation due to Bilateral Luteoma of Pregnancy
- Unusual Course of Acne Conglobata as a Skin Manifestation due to Bilateral Luteoma of Pregnancy
- Breast MRI in Pregnancy-Associated Breast Cancer
- MR Imaging of Focal Cervical Edema Mimicking Carcinoma: A Case Report