Korean J Radiol.
2005 Mar;6(1):41-43. 10.3348/kjr.2005.6.1.41.
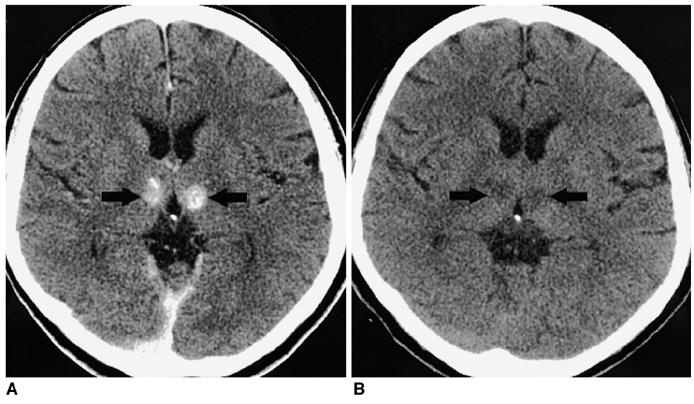
Bilateral Paramedian Thalamic Contrast Enhancement on CT after Intra-arterial Thrombolysis
- Affiliations
-
- 1Department of Radiology, Chonnam National University Medical School, Chonnam National University Hospital, Korea. radyoon@cnuh.com
- KMID: 1783172
- DOI: http://doi.org/10.3348/kjr.2005.6.1.41
Abstract
- A 58-year-old woman presented with an acute embolic occlusion of the distal basilar artery. She underwent angioplasty and intra-arterial thrombolysis. Angiography performed after recanalization revealed a single perforating thalamic artery. A nonenhanced CT scan carried out immediately after the procedure revealed hyperdense lesions in the bilateral paramedian portions of the thalami, which disappeared on the 24-hour follow-up CT scan. Three months later, the patient improved to functional independence, but had some memory dysfunction and vertical gaze palsy. This case suggests that contrast enhancement or extravasation can occur in the thalamus after intra-arterial thrombolysis performed to recanalize a basilar artery occlusion.
Keyword
MeSH Terms
Figure
Reference
-
1. Yoon W, Seo JJ, Kim JK, Cho KH, Park JG, Kang HK. Contrast enhancement and contrast extravasation on computed tomography after intra-arterial thrombolysis in patients with acute ischemic stroke. Stroke. 2004. 35:876–881.2. Nakano S, Iseda T, Kawano H, Yoneyama T, Ikeda T, Wakisaka S. Paranchymal hyperdensity on computed tomography after intra-arterial reperfusion therapy for acute middle cerebral artery occlusion: incidence and clinical significance. Stroke. 2001. 32:2042–2048.3. Yokogami K, Nakano S, Ohta H, Goya T, Wakisaka S. Prediction of hemorrhagic complications after thrombolytic therapy for middle cerebral artery occlusion: value of pre-and post-therapeutic computed tomographic findings and angiographic occlusive site. Neurosurgery. 1996. 39:1102–1107.4. Mericle RA, Lopes DK, Fronckowiak MD, Wakhloo AK, Guterman LR, Hopkins LN. A grading scale to predict outcomes after intra-arterial thrombolysis for stroke complicated by contrast extravasation. Neurosurgery. 2000. 46:1307–1315.5. Bogousslavsky J, Regli F, Uske A. Thalamic infarcts: clinical syndromes, etiology, and prognosis. Neurology. 1988. 38:837–848.6. Roitberg BZ, Tuccar E, Alp MS. Bilateral paramedian thalamic infarct in the presence of an unpaired thalamic perforating artery. Acta Neurochir. 2002. 144:301–304.7. Cosson A, Tatu L, Vuillier F, Parratte B, Diop M, Monnier G. Arterial vascularization of the human thalamus: extra-parenchymal arterial groups. Surg Radiol Anat. 2003. 25:408–415.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Paramedian Thalamic Infarction due to Occlusion of Artery of Percheron
- Two Cases of Bilateral Thalamic Infarction
- Acute Pseudobulbar Palsy After Bilateral Paramedian Thalamic Infarction: A Case Report
- The Effect of Intra-arterial Thrombolysis in Retinal Artery Occlusion: Case Series and Literature Review
- Bilateral Thalamic Infarction Related to Artery of Percheron with Microembolic Signal