Korean J Radiol.
2006 Jun;7(2):125-130. 10.3348/kjr.2006.7.2.125.
Safety and Effectiveness of Moderate Sedation for Radiologic Non-Vascular Intervention
- Affiliations
-
- 1Department of Radiology, Dankook University Hospital, Chungnam, Korea. radiology@dankook.ac.kr
- KMID: 1782185
- DOI: http://doi.org/10.3348/kjr.2006.7.2.125
Abstract
OBJECTIVE
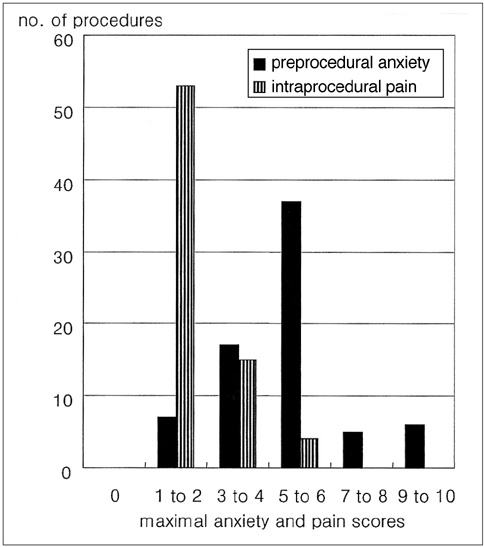
The purpose of this study was to prospectively characterize the safety and effectiveness of moderate sedation/analgesia for performing radiologic non-vascular abdominal intervention. MATERIALS AND METHODS: During a 3-month period, a total of 63 adult patients with a mean age of 64 years (range: 27-82) underwent moderate sedation for 72 radiologic non-vascular interventional procedures. A combination of fentanyl citrate and midazolam hydrochloride, based on the patient's body weight, was intravenously administered until the patient was drowsy and tranquil. The adverse events associated with this moderate sedation were assessed. The visual analog scale format was used to measure the subjective feelings of the patient's pre-procedural anxiety and intraprocedural pain. RESULTS: The mean total dose per kilogram of body weight of fentanyl used in PTBD was 1.148ug, it was 1.157ug for PTGBD, 1ug for AD, 1ug for PCN, 1.641ug for TDC, 1ug for DJS, 2ug for BS, 1ug for GS and 2ug for RFA. The mean total dose per kilogram of body weight of midazolam was 0.035 mg in PTBD, PTGBD, AD, PCN, DJS, GS and RFA, 0.039 mg in TDC, and 0.043 mg in BS. A temporary reduction of systolic blood pressure to less than 80 mmHg was observed during 5 procedures (6.9%), whereas a temporary elevation of systolic blood pressure above 150 mmHg was observed during 10 procedures (13.8%). A reduction of arterial oxygen saturation to less than 90% was observed during 14 procedures (19.4%). None of the patients required pharmacologic reversal agents or cardiopulmonary resuscitation. The mean anxiety score recorded before all procedures was 5.2 (distressing). The mean pain score during the procedure, which was recorded after all procedures, was 2.9 (mild). CONCLUSION: Moderate sedation allows performance of safe and effective radiologic non-vascular intervention, and it is also easy for an interventional radiologist to use. The patients should be continuously monitored to check their vital signs and arterial oxygen saturation during the procedures.
MeSH Terms
Figure
Reference
-
1. Mueller PR, Biswal S, Halpern EF, Kaufman JA, Lee MJ. Interventional radiologic procedures: patient anxiety, perception of pain, understanding of procedure, and satisfaction with medication-a prospective study. Radiology. 2000. 215:684–688.2. Harshfield DL, Teplick SK, Brandon JC. Pain control during interventional biliary procedures: epidural anesthesia vs iv sedation. AJR Am J Roentgenol. 1993. 161:1057–1059.3. Lang EV, Chen F, Fick LJ, Berbaum KS. Determinants of intravenous conscious sedation for arteriography. J Vasc Interv Radiol. 1998. 9:407–412.4. Kennedy PT, Kelly IM, Loan WC, Boyd CS. Conscious sedation and analgesia for routine aortofemoral arteriography: a prospective evaluation. Radiology. 2000. 216:660–664.5. Wagner HJ, Nowacki J, Klose KJ. Propofol versus midazolam for sedation during percutaneous transluminal angioplasty. J Vasc Interv Radiol. 1996. 7:673–680.6. Martin ML, Lennox PH. Sedation and analgesia in the interventional radiology department. J Vasc Interv Radiol. 2003. 14:1119–1128.7. Skehan SJ, Malone DE, Buckley N, Matsumoto S, Rawlinson J, Ting G, et al. Sedation and analgesia in adult patients: evaluation of a staged-dose system based on body weight for use in abdominal interventional radiology. Radiology. 2000. 216:653–659.8. Whitwam JG. Minimally invasive therapy--implications for anaesthesia. Anaesthesia. 1993. 48:937–939.9. Bluemke DA, Breiter SN. Sedation procedures in MR imaging: safety, effectiveness, and nursing effect on examinations. Radiology. 2000. 216:645–652.10. American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002. 96:1004–1017.11. Innes G, Murphy M, Nijssen-Jordan C, Ducharme J, Drummond A. Procedural sedation and analgesia in the emergency department. Canadian Consensus Guidelines. J Emerg Med. 1999. 17:145–156.12. Krauss B, Green SM. Sedation and analgesia for procedures in children. N Engl J Med. 2000. 342:938–945.13. Arepally A, Oechsle D, Kirkwood S, Savader SJ. Safety of conscious sedation in interventional radiology. Cardiovasc Intervent Radiol. 2001. 24:185–190.14. Monk TG. Clinical applications of monitored anesthesia care. Minim Invasive Therapy. 1994. 3:17S–20S.15. McDermott VG, Chapman ME, Gillespie I. Sedation and patient monitoring in vascular and interventional radiology. Br J Radiol. 1993. 66:667–671.16. Yaster M, Nichols DG, Deshpande JK, Wetzel RC. Midazolam-fentanyl intravenous sedation in children: case report of respiratory arrest. Pediatrics. 1990. 86:463–467.17. Michalodimitrakis M, Christodoulou P, Tsatsakis AM, Askoxilakis I, Stiakakis I, Mouzas I. Death related to midazolam overdose during endoscopic retrograde cholangiopancreatography. Am J Forensic Med Pathol. 1999. 20:93–97.18. Bailey PL, Pace NL, Ashburn MA, Moll JW, East KA, Stanley TH. Frequent hypoxemia and apnea after sedation with midazolam and fentanyl. Anesthesiology. 1990. 73:826–830.19. Cragg AH, Smith TP, Berbaum KS, Nakagawa N. Radomized double-blind trial of midazolam/placebo and midazolam/fentanyl for sedation and analgesia in lower-extremity angiography. AJR Am J Roentgenol. 1991. 157:173–176.20. Ben-Shlomo I, abd-el-Khalim H, Ezry J, Zohar S, Tverskoy M. Midazolam acts synergistically with fentanyl for induction of anaesthesia. Br J Anaesth. 1990. 64:45–47.21. Lind LJ, Mushlin PS. Sedation, analgesia, and anesthesia for radiologic procedures. Cardiovasc Intervent Radiol. 1987. 10:247–253.22. Ayre-Smith G. Fentanyl and midazolam: an alternative to diazepam. Radiology. 1987. 164:285.23. Sacchetti A, Schafermeyer R, Geradi M, Graneto J, Fuerst RS, Cantor R, et al. Pediatric analgesia and sedation. Ann Emerg Med. 1994. 23:237–250.24. Murphy MF. Sedation. Ann Emerg Med. 1996. 27:461–463.25. Green SM, Krauss B. Procedural sedation terminology: moving beyond "conscious sedation". Ann Emerg Med. 2002. 39:433–435.26. Cote CJ. "Conscious sedation": time for this oxymoron to go away! J Pediatr. 2001. 139:15–17.27. Miller DL, Wall RT. Fentanyl and diazepam for analgesia and sedation during radiologic special procedures. Radiology. 1987. 162:195–198.28. Lundgren S, Rosenquist JB. Amnesia, pain experience, and patient satisfaction after sedation with intravenous diazepam. J Oral Maxillofac Surg. 1983. 41:99–102.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Considerable Variability of Procedural Sedation and Analgesia Practices for Gastrointestinal Endoscopic Procedures in Europe
- Inhalation Sedation: A Systematic Review and Meta-Analysis
- The Effectiveness and Side Effects of Conscious Sedation using Chloral hydrate, Hydroxyzine, and Nitrous oxide
- General Anesthesia and Endoscopic Upper Gastrointestinal Tumor Resection
- Safety and efficacy of target controlled infusion administration of propofol and remifentanil for moderate sedation in non-hospital dental practice