Yonsei Med J.
2012 Jan;53(1):91-98. 10.3349/ymj.2012.53.1.91.
Plasma Adiponectin Concentration and Its Association with Metabolic Syndrome in Patients with Heart Failure
- Affiliations
-
- 1Cardiology Division, Severance Cardiovascular Hospital and Cardiovascular Research Institute, Yonsei University College of Medicine, Seoul, Korea. smkang@yuhs.ac
- 2Brain Korea 21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Food and Nutrition, Korea University, Seoul, Korea.
- KMID: 1779691
- DOI: http://doi.org/10.3349/ymj.2012.53.1.91
Abstract
- PURPOSE
Plasma adiponectin concentrations are inversely related with metabolic syndrome (MetS), and MetS is associated with increased risk for heart failure (HF). However, the relationship between adiponectin and MetS in HF remains undetermined. Therefore, we tested whether MetS was associated with the degree of plasma adiponectin concentrations in HF patients.
MATERIALS AND METHODS
One hundred twenty eight ambulatory HF patients with left ventricular ejection fraction of <50% (80 males, 61.8+/-11.9 years old) were enrolled for this cross-sectional study. Echocardiographic measurements were performed, and plasma concentrations of adiponectin, lipoproteins, apolipoproteins (apoB, apoA1) and high sensitive C-reactive protein (hsCRP) were measured.
RESULTS
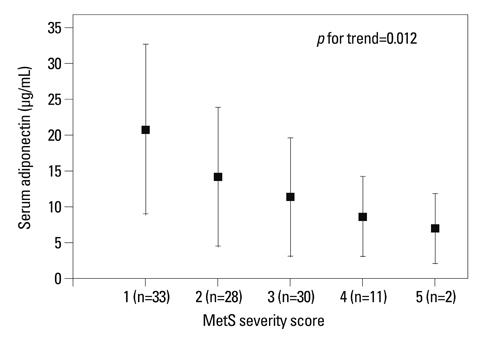
Adiponectin concentrations in HF patients with MetS (n=43) were significantly lower than those without MetS (n=85) (9.7+/-7.0 vs. 15.8+/-10.9 microg/mL, p=0.001). Higher concentrations of apoB (p=0.017), apoB/A1 ratio (p<0.001), blood urea nitrogen (p=0.034), creatinine (p=0.003), and fasting insulin (p=0.004) were observed in HF patients with MetS compared with those without MetS. In HF patients with MetS, adiponectin concentrations were negatively correlated with hsCRP (r=-0.388, p=0.015) and positively correlated with the ratio of early mitral inflow velocity to early diastolic mitral annular velocity, E/E' (r=0.399, p=0.015). There was a significant trend towards decreased adiponectin concentrations with an increasing number of components of MetS (p for trend=0.012).
CONCLUSION
Our study demonstrated that adiponectin concentrations decreased in HF patients with MetS, and that relationship between adiponectin, inflammation and abnormal diastolic function, possibly leading to the progression of HF.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Red Cell Distribution Width as an Independent Predictor of Exercise Intolerance and Ventilatory Inefficiency in Patients with Chronic Heart Failure
Sung-Jin Hong, Jong-Chan Youn, Jaewon Oh, Namki Hong, Hye Sun Lee, Sungha Park, Sang-Hak Lee, Donghoon Choi, Seok-Min Kang
Yonsei Med J. 2014;55(3):635-643. doi: 10.3349/ymj.2014.55.3.635.Lack of Superiority for Soluble ST2 over High Sensitive C-Reactive Protein in Predicting High Risk Coronary Artery Calcium Score in a Community Cohort
Jaewon Oh, Sungha Park, Hee Tae Yu, Hyuk-Jae Chang, Sang-Hak Lee, Seok-Min Kang, Donghoon Choi
Yonsei Med J. 2016;57(6):1347-1353. doi: 10.3349/ymj.2016.57.6.1347.
Reference
-
1. Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999. 257:79–83.
Article2. Pellmé F, Smith U, Funahashi T, Matsuzawa Y, Brekke H, Wiklund O, et al. Circulating adiponectin levels are reduced in nonobese but insulin-resistant first-degree relatives of type 2 diabetic patients. Diabetes. 2003. 52:1182–1186.
Article3. Ouchi N, Kihara S, Funahashi T, Nakamura T, Nishida M, Kumada M, et al. Reciprocal association of C-reactive protein with adiponectin in blood stream and adipose tissue. Circulation. 2003. 107:671–674.
Article4. Matsushita K, Yatsuya H, Tamakoshi K, Wada K, Otsuka R, Takefuji S, et al. Comparison of circulating adiponectin and proinflammatory markers regarding their association with metabolic syndrome in Japanese men. Arterioscler Thromb Vasc Biol. 2006. 26:871–876.
Article5. Kumada M, Kihara S, Sumitsuji S, Kawamoto T, Matsumoto S, Ouchi N, et al. Association of hypoadiponectinemia with coronary artery disease in men. Arterioscler Thromb Vasc Biol. 2003. 23:85–89.
Article6. Hashimoto N, Kanda J, Nakamura T, Horie A, Kurosawa H, Hashimoto T, et al. Association of hypoadiponectinemia in men with early onset of coronary heart disease and multiple coronary artery stenoses. Metabolism. 2006. 55:1653–1657.
Article7. Adamczak M, Wiecek A, Funahashi T, Chudek J, Kokot F, Matsuzawa Y. Decreased plasma adiponectin concentration in patients with essential hypertension. Am J Hypertens. 2003. 16:72–75.
Article8. Biolo A, Shibata R, Ouchi N, Kihara S, Sonoda M, Walsh K, et al. Determinants of adiponectin levels in patients with chronic systolic heart failure. Am J Cardiol. 2010. 105:1147–1152.
Article9. George J, Patal S, Wexler D, Sharabi Y, Peleg E, Kamari Y, et al. Circulating adiponectin concentrations in patients with congestive heart failure. Heart. 2006. 92:1420–1424.
Article10. Kistorp C, Faber J, Galatius S, Gustafsson F, Frystyk J, Flyvbjerg A, et al. Plasma adiponectin, body mass index, and mortality in patients with chronic heart failure. Circulation. 2005. 112:1756–1762.
Article11. Tsutamoto T, Tanaka T, Sakai H, Ishikawa C, Fujii M, Yamamoto T, et al. Total and high molecular weight adiponectin, haemodynamics, and mortality in patients with chronic heart failure. Eur Heart J. 2007. 28:1723–1730.
Article12. Celik T, Yaman H. Elevated adiponectin levels in patients with chronic heart failure: an independent predictor of mortality or a marker of cardiac cachexia? Int J Cardiol. 2010. 144:319–320.
Article13. Steering Committee of the WHO Western Pacific Region, IASO & IOTF. The Asia-Pacific perspective: redefining obesity and its treatment. 2000. Austrailia:14. Tamariz L, Hassan B, Palacio A, Arcement L, Horswell R, Hebert K. Metabolic syndrome increases mortality in heart failure. Clin Cardiol. 2009. 32:327–331.
Article15. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002. 39:S1–S266.16. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985. 28:412–419.
Article17. Shim CY, Park S, Kim JS, Shin DJ, Ko YG, Kang SM, et al. Association of plasma retinol-binding protein 4, adiponectin, and high molecular weight adiponectin with insulin resistance in non-diabetic hypertensive patients. Yonsei Med J. 2010. 51:375–384.
Article18. Salas-Salvadó J, Granada M, Bulló M, Corominas A, Casas P, Foz M. Plasma adiponectin distribution in a Mediterranean population and its association with cardiovascular risk factors and metabolic syndrome. Metabolism. 2007. 56:1486–1492.
Article19. Koh SB, Yoon J, Kim JY, Yoo BS, Lee SH, Park JK, et al. Relationships between serum adiponectin with metabolic syndrome and components of metabolic syndrome in non-diabetic Koreans: ARIRANG Study. Yonsei Med J. 2011. 52:234–241.
Article20. Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005. 366:1640–1649.
Article21. Park JS, Cho MH, Nam JS, Yoo JS, Lee YB, Roh JM, et al. Adiponectin is independently associated with apolipoprotein B to A-1 ratio in Koreans. Metabolism. 2010. 59:677–682.
Article22. Takano H, Obata JE, Kodama Y, Kitta Y, Nakamura T, Mende A, et al. Adiponectin is released from the heart in patients with heart failure. Int J Cardiol. 2009. 132:221–226.
Article23. Ingelsson E, Arnlöv J, Sundström J, Zethelius B, Vessby B, Lind L. Novel metabolic risk factors for heart failure. J Am Coll Cardiol. 2005. 46:2054–2060.
Article24. Sugiura K, Tamakoshi K, Yatsuya H, Otsuka R, Wada K, Matsushita K, et al. Contribution of adipocytokines to low-grade inflammatory state as expressed by circulating C-reactive protein in Japanese men: comparison of leptin and adiponectin. Int J Cardiol. 2008. 130:159–164.
Article25. Gustafsson S, Lind L, Zethelius B, Venge P, Flyvbjerg A, Söderberg S, et al. Adiponectin and cardiac geometry and function in elderly: results from two community-based cohort studies. Eur J Endocrinol. 2010. 162:543–550.
Article26. Unno K, Shibata R, Izawa H, Hirashiki A, Murase Y, Yamada T, et al. Adiponectin acts as a positive indicator of left ventricular diastolic dysfunction in patients with hypertrophic cardiomyopathy. Heart. 2010. 96:357–361.
Article27. Kuznetsova T, Herbots L, López B, Jin Y, Richart T, Thijs L, et al. Prevalence of left ventricular diastolic dysfunction in a general population. Circ Heart Fail. 2009. 2:105–112.
Article28. Perry GJ, Ahmed MI, Desai RV, Mujib M, Zile M, Sui X, et al. Left ventricular diastolic function and exercise capacity in community-dwelling adults ≥65 years of age without heart failure. Am J Cardiol. 2011. 108:735–740.
Article29. Sharp AS, Tapp RJ, Thom SA, Francis DP, Hughes AD, Stanton AV, et al. Tissue Doppler E/E' ratio is a powerful predictor of primary cardiac events in a hypertensive population: an ASCOT substudy. Eur Heart J. 2010. 31:747–752.
Article30. Gardin JM, Leifer ES, Fleg JL, Whellan D, Kokkinos P, Leblanc MH, et al. Relationship of Doppler-Echocardiographic left ventricular diastolic function to exercise performance in systolic heart failure: the HF-ACTION study. Am Heart J. 2009. 158:S45–S52.
Article31. Hwang YC, Jee JH, Kang M, Rhee EJ, Sung J, Lee MK. Metabolic syndrome and insulin resistance are associated with abnormal left ventricular diastolic function and structure independent of blood pressure and fasting plasma glucose level. Int J Cardiol. 2011. [Epub ahead of print].
Article32. Kirpichnikov D, McFarlane SI, Sowers JR. Heart failure in diabetic patients: utility of beta-blockade. J Card Fail. 2003. 9:333–344.33. Kovacić D, Marinsek M, Gobec L, Lainscak M, Podbregar M. Effect of selective and non-selective beta-blockers on body weight, insulin resistance and leptin concentration in chronic heart failure. Clin Res Cardiol. 2008. 97:24–31.
Article34. Yamaji M, Tsutamoto T, Tanaka T, Kawahara C, Nishiyama K, Yamamoto T, et al. Effect of carvedilol on plasma adiponectin concentration in patients with chronic heart failure. Circ J. 2009. 73:1067–1073.
Article35. Van Berendoncks AM, Beckers P, Hoymans VY, Possemiers N, Coenen S, Elseviers MM, et al. Beta-blockers modify the prognostic value of adiponectin in chronic heart failure. Int J Cardiol. 2011. 150:296–300.
Article36. Haugen E, Furukawa Y, Isic A, Fu M. Increased adiponectin level in parallel with increased NT-pro BNP in patients with severe heart failure in the elderly: a hospital cohort study. Int J Cardiol. 2008. 125:216–219.
Article37. Coughlin CC, Finck BN, Eagon JC, Halpin VJ, Magkos F, Mohammed BS, et al. Effect of marked weight loss on adiponectin gene expression and plasma concentrations. Obesity (Silver Spring). 2007. 15:640–645.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Association Between Plasma Adiponectin and the Components of Metabolic Syndrome in Adults with Abdominal Obesity
- The Role of Plasma Adiponectin and Polymorphism of Adiponectin Gene in the Development of Type 2 Diabetes Mellitus
- Adiponectin in Women with Polycystic Ovary Syndrome
- Interrelationship between Plasma Adiponectin and Cardiovascular Outcomes in Patients with End-Stage Renal Disease
- Serum adiponectin concentration according to visceral fat amount and its relationship of metabolic risk factors in premenopausal obese women