J Korean Med Sci.
2013 Jul;28(7):1048-1054. 10.3346/jkms.2013.28.7.1048.
Chronic Obstructive Pulmonary Disease Assessment Test Can Predict Depression: A Prospective Multi-Center Study
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea. pulmoks@hallym.ac.kr
- 3Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Genome Research Center for Allergy and Respiratory Disease, Soonchunhyang University Hospital, Bucheon, Korea.
- 5Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 6Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
- 7Department of Internal Medicine, Gangneung Asan Hospital, College of Medicine, University of Ulsan, Gangneung, Korea.
- 8Department of Internal Medicine, College of Medicine, Yeungnam University, Daegu, Korea.
- 9Department of Pulmonary and Critical Care Medicine, Kangdong Sacred Heart Hospital, Seoul, Korea.
- KMID: 1777501
- DOI: http://doi.org/10.3346/jkms.2013.28.7.1048
Abstract
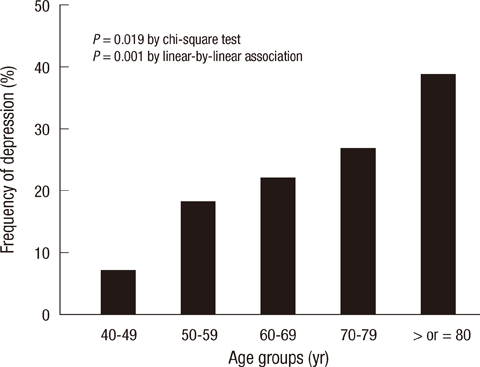
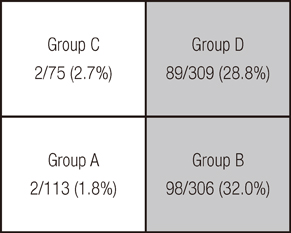
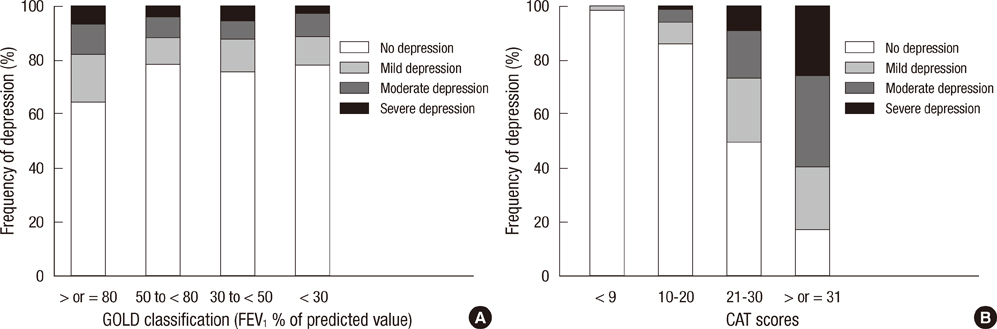
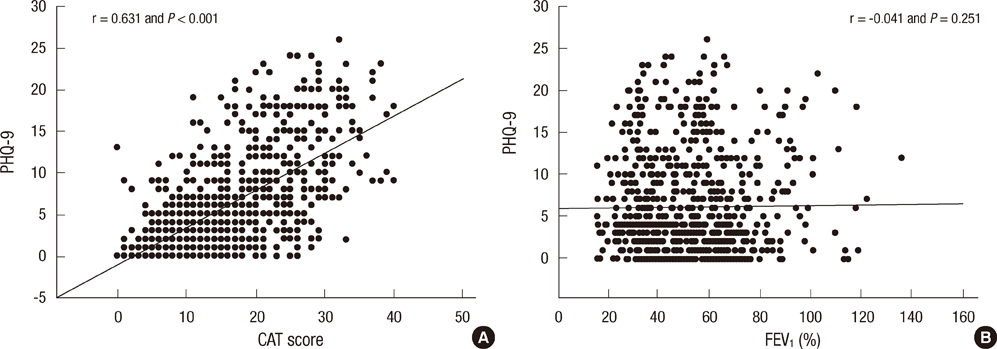
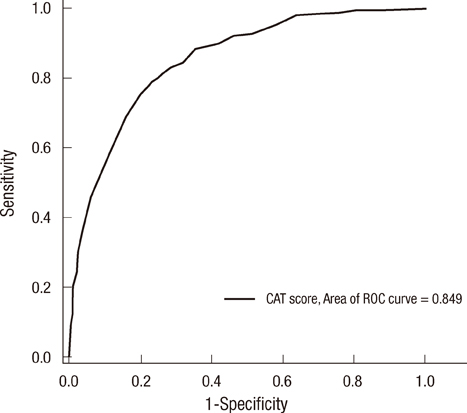
- This study was conducted to investigate the association between the chronic obstructive pulmonary disease (COPD) assessment test (CAT) and depression in COPD patients. The Korean versions of the CAT and patient health questionnaire-9 (PHQ-9) were used to assess COPD symptoms and depressive disorder, respectively. In total, 803 patients with COPD were enrolled from 32 hospitals and the prevalence of depression was 23.8%. The CAT score correlated well with the PHQ-9 score (r=0.631; P<0.001) and was significantly associated with the presence of depression (beta+/-standard error, 0.452+/-0.020; P<0.001). There was a tendency toward increasing severity of depression in patients with higher CAT scores. By assessment groups based on the 2011 Global Initiative for Chronic Obstructive Lung Disease guidelines, the prevalence of depression was affected more by current symptoms than by airway limitation. The area under the receiver operating characteristic curve for the CAT was 0.849 for predicting depression, and CAT scores > or =21 had the highest accuracy rate (80.6%). Among the eight CAT items, energy score showed the best correlation and highest power of discrimination. CAT scores are significantly associated with the presence of depression and have good performance for predicting depression in COPD patients.
MeSH Terms
Figure
Reference
-
1. Abrams TE, Vaughan-Sarrazin M, Van der Weg MW. Acute exacerbations of chronic obstructive pulmonary disease and the effect of existing psychiatric comorbidity on subsequent mortality. Psychosomatics. 2011; 52:441–449.2. Dalal AA, Shah M, Lunacsek O, Hanania NA. Clinical and economic burden of depression/anxiety in chronic obstructive pulmonary disease patients within a managed care population. COPD. 2011; 8:293–299.3. Jennings JH, Digiovine B, Obeid D, Frank C. The association between depressive symptoms and acute exacerbations of COPD. Lung. 2009; 187:128–135.4. Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital read-mission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007; 167:60–67.5. Maurer J, Rebbapragada V, Borson S, Goldstein R, Kunik ME, Yohannes AM, Hanania NA. ACCP Workshop Panel on Anxiety and Depression in COPD. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008; 134:43S–56S.6. Hanania NA, Müllerova H, Locantore NW, Vestbo J, Watkins ML, Wouters EF, Rennard SI, Sharafkhaneh A. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Study Investigators. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am J Respir Crit Care Med. 2011; 183:604–611.7. Von Leupoldt A, Taube K, Lehmann K, Fritzsche A, Magnussen H. The impact of anxiety and depression on outcomes of pulmonary rehabilitation in patients with COPD. Chest. 2011; 140:730–736.8. Al-shair K, Dockry R, Mallia-Milanes B, Kolsum U, Singh D, Vestbo J. Depression and its relationship with poor exercise capacity, BODE index and muscle wasting in COPD. Respir Med. 2009; 103:1572–1579.9. Balcells E, Gea J, Ferrer J, Serra I, Orozco-Levi M, de Batlle J, Rodriguez E, Benet M, Donaire-González D, Antó JM, et al. Factors affecting the relationship between psychological status and quality of life in COPD patients. Health Qual Life Outcomes. 2010; 8:108.10. Ito K, Kawayama T, Shoji Y, Fukushima N, Matsunaga K, Edakuni N, Uchimura N, Hoshino T. Depression, but not sleep disorder, is an independent factor affecting exacerbations and hospitalization in patients with chronic obstructive pulmonary disease. Respirology. 2012; 17:940–949.11. Kil SY, Oh WO, Koo BJ, Suk MH. Relationship between depression and health-related quality of life in older Korean patients with chronic obstructive pulmonary disease. J Clin Nurs. 2010; 19:1307–1314.12. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009; 34:648–654.13. COPD Assessment Test. accessed on 1 January 2011. Available at http://www.catestonline.org.14. Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ, Nishimura M, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013; 187:347–365.15. Hwang YI, Lee YS, Oh YM, Lee SD, Park SW, Kim YS, In KH, Jung BH, Lee KH, Ra SW, et al. Prevalence of depression and its influence on health-related quality of life in COPD patients. Chest. 2011; 140:542A.16. Han C, Jo SA, Kwak JH, Pae CU, Steffens D, Jo I, Park MH. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric Study. Compr Psychiatry. 2008; 49:218–223.17. Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006; 21:547–552.18. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16:606–613.19. Lamers F, Jonkers CC, Bosma H, Penninx BW, Knottnerus JA, van Eijk JT. Summed score of the Patient Health Questionnaire-9 was a reliable and valid method for depression screening in chronically ill elderly patients. J Clin Epidemiol. 2008; 61:679–687.20. Ringbaek T, Martinez G, Lange P. A comparison of the assessment of quality of life with CAT, CCQ, and SGRQ in COPD patients participating in pulmonary rehabilitation. COPD. 2012; 9:12–15.21. Lee S, Lee JS, Song JW, Choi CM, Shim TS, Kim TB, Cho YS, Moon HB, Lee SD, Oh YM. Validation of the Korean version of chronic obstructive pulmonary disease assessment test (CAT) and dyspnea-12 questionnaire. Tuberc Respir Dis. 2010; 69:171–176.22. Chavannes NH, Huibers MJ, Schermer TR, Hendriks A, van Weel C, Wouters EF, van Schayck CP. Associations of depressive symptoms with gender, body mass index and dyspnea in primary care COPD patients. Fam Pract. 2005; 22:604–607.23. De S. Prevalence of depression in stable chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2011; 53:35–39.24. Di Marco F, Verga M, Reggente M, Maria Casanova F, Santus P, Blasi F, Allegra L, Centanni S. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir Med. 2006; 100:1767–1774.25. Pincus HA, Hough L, Houtsinger JK, Rollman BL, Frank RG. Emerging models of depression care: multi-level ('6 P') strategies. Int J Methods Psychiatr Res. 2003; 12:54–63.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of COPD Assessment Test as valuable predictor of depression in chronic obstructive pulmonary disease
- Nutritional Assessment in Patients with Chronic Obstructive Pulmonary Disease
- Symptom Experience, Self-Efficacy, Depression, and Medication Adherence in Patients with Chronic Obstructive Pulmonary Disease
- Cor Pulmonale with Particular Reference to Chronic Obstructive Pulmonary Disease and Pulmonary Tuberculosis
- Effect of Depression on Pulmonary Symptoms and Quality of Life in Patients with Chronic Obstructive Pulmonary Disease