J Korean Soc Spine Surg.
2008 Sep;15(3):133-139. 10.4184/jkss.2008.15.3.133.
Radiologic Changes of Adjacent-level after Anterior Cervical Spinal Fusion: Midterm Follow-up Results
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dong-A University, Busan, Korea. gylee@dau.ac.kr
- 2Department of Orthopedic Surgery, Dong-Eui Medical Center, Busan, Korea.
- KMID: 1747196
- DOI: http://doi.org/10.4184/jkss.2008.15.3.133
Abstract
-
STUDY DESIGN: We studied the changes of the adjacent-level after performing anterior cervical interbody fusion.
OBJECTIVES
We retrospectively analyzed the radiologic changes such as the degenerative changes and osteophyte formation in the adjacent-level and the affecting factors that affect the changes of the adjacent level after anterior cervical interbody fusion. SUMMARY OF LITERATURE REVIEW: We studied the patients who were more than sixty years old and who had more degeneration at the time of operation and who developed symptomatic new disease within the first four years after their procedure. When the interbody spacer was shortened by 10% to simulate subsidence, the plate lost nearly 70% of its load-sharing capabilities.
MATERIALS AND METHODS
All the patients were treated with a plate and an autoiliac bone graft. We reviewed the correlation between the changes in the adjacent level and the factors that included gender, age, the fused segments, the plate-to-disc distance, the preoperative degenerative changes in the adjacent level, subsidence of the graft bone, the height of the graft bone, fracture and dislocation, and loosening of the implant.
RESULTS
Radiologic changes in the adjacent-level were seen in 35 cases and these cases included 27 cases in the upper level and 17 cases in lower level. Adjacent level changes were seen in 27 of the 37 (73%) patient who were above 50 years old. Adjacent level changes were seen in 19 (90.5%) of the 21 cases that had preoperative cephalad level degeneration, and adjacent level changes were seen in 9 (81.8%) of the 11 cases that had preoperative caudal degeneration. Adjacent level degeneration developed or increased in the cases of subsidence of a graft over 2 mm.
CONCLUSIONS
The patients who undergo anterior cervical interbody fusion need to be continuously followed up because radiologic changes can increase in the case with degenerative change in the adjacent segment and subsidence of the bone graft of more than 2 mm.
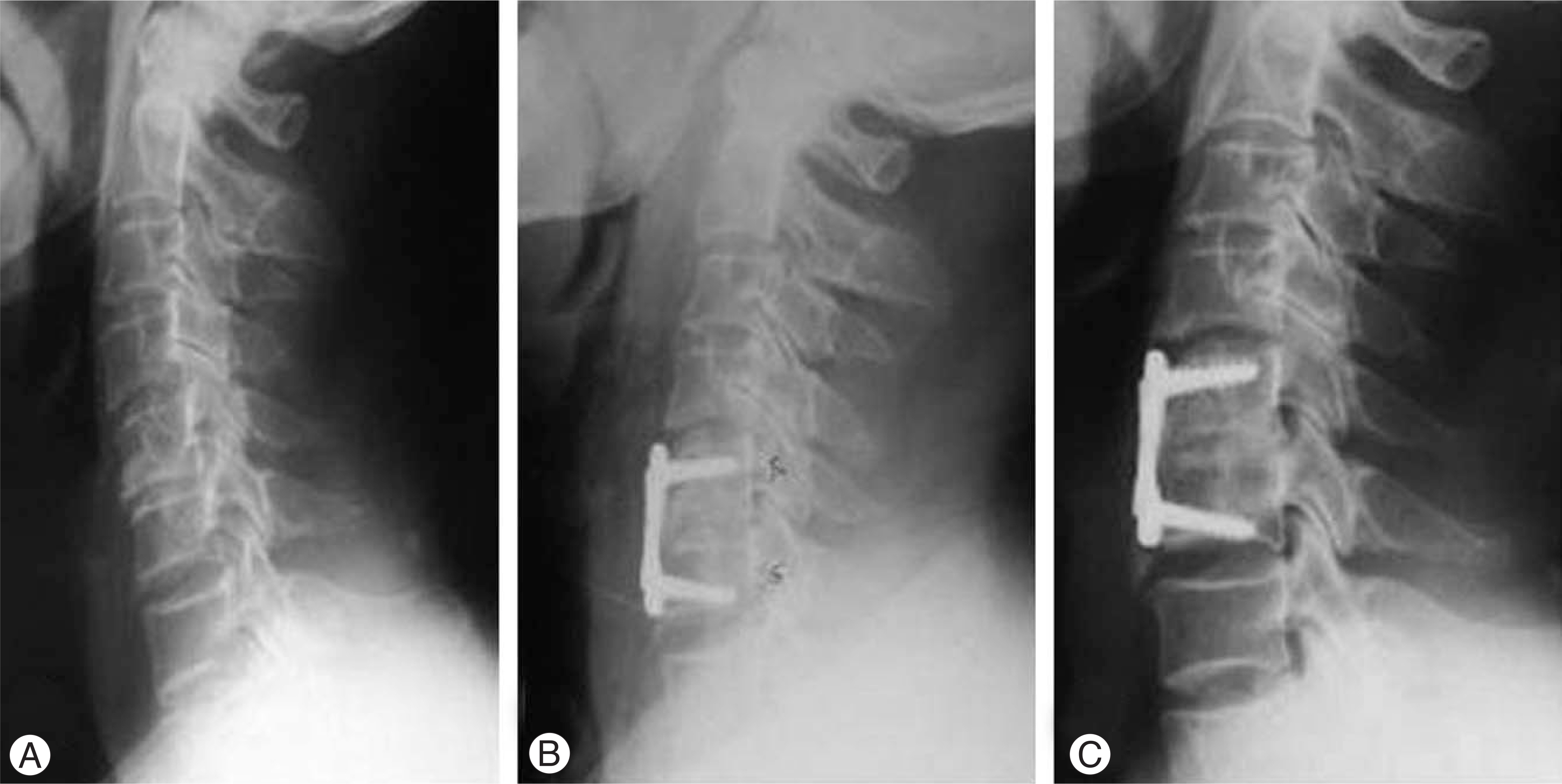
Figure
Reference
-
1). Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40:607–624.
Article2). Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958; 15:602–617.
Article3). Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993; 18:2167–2173.
Article4). Goffin J, van Loon J, Van Calenbergh F, Plets C. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J. Spinal Disord. 1995; 8:500–508.5). Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J. Am. Statist. Assn. 1958; 53:457–481.6). McGrory BJ, Klassen RA. Arthrodesis of the cervical spine for fractures and dislocations in children and adolescents. A long-term follow-up study. J. Bone and Joint Surg Am. 1994; 76:1606–1616.7). Brodke DS, Gollogly S, Mohr RA, Nguyen BK, Dailey AT, Bachus KN. Dynamic cervical plates: biomechanical evaluation of load sharing and stiffness. Spine. 2001; 26:1324–1329.8). Cochran T, Irstan L, Nachemson A. Long-term anatomic and functional changes in patients with adolescent idiopathic scoliosis treated by Harrington rod fusion. Spine. 1983; 8:576–583.
Article9). Frymoyer JW. Failed lumbar disc surgery requiring a second operation. Spine. 1978; 3:7–11.10). Ginsberg HH, Goldstein LA, Robinson SC. Back pain in postoperative idiopathic scoliosis long-term follow-up study. Spine. 1979; 4:518.11). Kahanovitz N, Bullough P, Jacobs RR. The effect of internal fixation without arthrodesis on human facet joint cartilage. Clin Orthop. 1984; 189:204–208.
Article12). Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988; 13:375–377.
Article13). Whitecloud TS, Davis JM, Olive PM. Operative treatment of the degenerated segment adjacent to a lumbar fusion. Spine. 1994; 19:531–536.
Article14). Park JB, Cho YS, Reiw D. Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am. 2005; 87:558–563.
Article15). Chow DH, Luk KD, Evans JH, Leong JC. Effects of short anterior lumbar interbody fusion on the biomechanics of neighboring unfused segments. Spine. 1996; 21:549–555.16). Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989; 25:491–502.
Article17). Caspar W, Geisler FH, Pitzen T, Johnson TA. Anterior cervical plate stabilization in one and two level degenerative disease: overtreatment or benefit? J Spinal Disord. 1998; 11:1–11.18). Caspar W, Pitzen T, Papavero L, Geisler FH, Johnson TA. Anterior cervical plating for the treatment of neoplasms in the cervical vertebrae. J Neurosurg. 1999; 90:27–34.
Article19). Connolly PJ, Esses SI, Kostuik JP. Anterior cervical fusion: outcome analysis of patients fused with and without anterior cervical plates. J Spinal Disord. 1996; 9:202–206.20). Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002; 50:229–238.
Article21). Fuller DA, Kirkpatrick JS, Emery SE, Wilber RG, Davy DT. A kinematic study of the cervical spine before and after segmental arthrodesis. Spine. 1998; 23:1649–1656.
Article22). Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999; 81:519–528.
Article23). Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine. 1999; 24:670–675.
Article24). Wu W, Thuomas KA, Hedlund R, Leszniewski W, Vavruch L. Degenerative changes following anterior cervical discectomy and fusion evaluated by fast spinecho MR imaging. Acta Radiol. 1996; 37:614–617.
Article25). Goran A. Fracture and dislocation of cervical spine. Value of anterior approach. New York State J Med. 1969; 69:1050.26). Williams JL, Allen MB Jr, Harkess JW. Late results of cervical discectomy and interbody fusion: some factors influencing the results. J Bone Joint Surg Am. 1968; 50:277–286.27). An HS, Evanich CJ, Nowicki BH, Haughton VM. Ideal thickness of Smith-Robinson graft for anterior cervical fusion: A cadaveric study with computed tomographic correlation. Spine. 1993; 18:2043–2047.28). Ma¨hring M. [Segment changes in the cervical spine following cervical spondylodeses of unstable injuries]. Unfallchirurgie. 1988; 14:247–258.29). Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine. 2004; 4:624–628.
Article30). Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J. Bone and Joint Surg Am. 1990; 72:1178–1184.31). Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine. 1986; 11:521–524.
Article32). Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate: a prospective comparative analysis. J Neurosurg. 1996; 85:206–210.
Article33). Closkey RF, Parsons JR, Lee CK, Blacksin MF, Zimmerman MC. Mechanics of interbody spinal fusion. Analysis of critical bone graft area. Spine. 1993; 18:1011–1015.34). Tye GW, Graham RS, Broaddus WC, Young HF. Graft subsidence after instrument-assisted anterior cervical fusion. J Neurosurg. 2002; 97:186–192.
Article35). Brodke DS, Klimo P Jr, Bachus KN, Braun JT, Dailey AT. Anterior cervical fixation: Analysis of load-sharing and stability with use of static and dynamic plates. J Bone Joint Surg Am. 2006; 88:1566–1573.36). Kim KS. Long-term effects on the cervical spine after anterior locking plate fixation. J Korean Neurosurg Soc. 2001; 30:493–500.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Radiologic Factors Affecting Longterm Surgical Results of Anterior Cervical Fusion Patients
- Changes of Adjacent Segment in Anterior Cervical Fusion
- Comparative Study of Two-Level Hybrid Surgery (Cervical Artificial Disc with Cage) with Two-Level Anterior Cervical Interbody Fusion for Multi-level Cervical Degenerative Disease
- Prevalence And Risk Factor of Degenerative Disease of Adjacent Segment after Anterior Cervical Arthrodesis
- Comparison of Adjacent Segment Degeneration, Cervical Alignment, and Clinical Outcomes after One- and Multilevel Anterior Cervical Discectomy and Fusion