Korean J Gastroenterol.
2010 Nov;56(5):293-298. 10.4166/kjg.2010.56.5.293.
Comparison of the Cut Direction between Gross Finding, Streoscopic Finding, and Pathologic Mapping of Endoscopic Submucosal Dissection Specimen
- Affiliations
-
- 1Department of Internal Medicine, Institute for Digestive Research, Soonchunhyang University College of Medicine, Seoul, Korea. cjy6695@dreamwiz.com
- 2Department of Pathology, Soonchunhyang University College of Medicine, Seoul, Korea.
- KMID: 1718370
- DOI: http://doi.org/10.4166/kjg.2010.56.5.293
Abstract
- BACKGROUND/AIMS
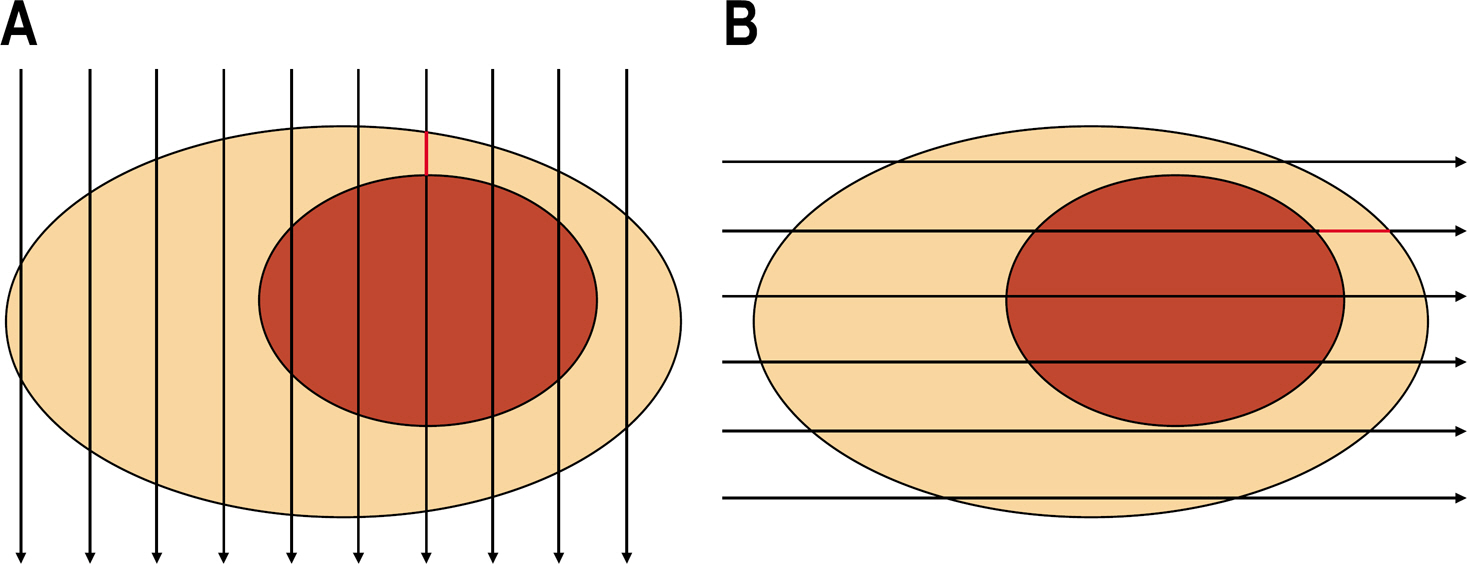
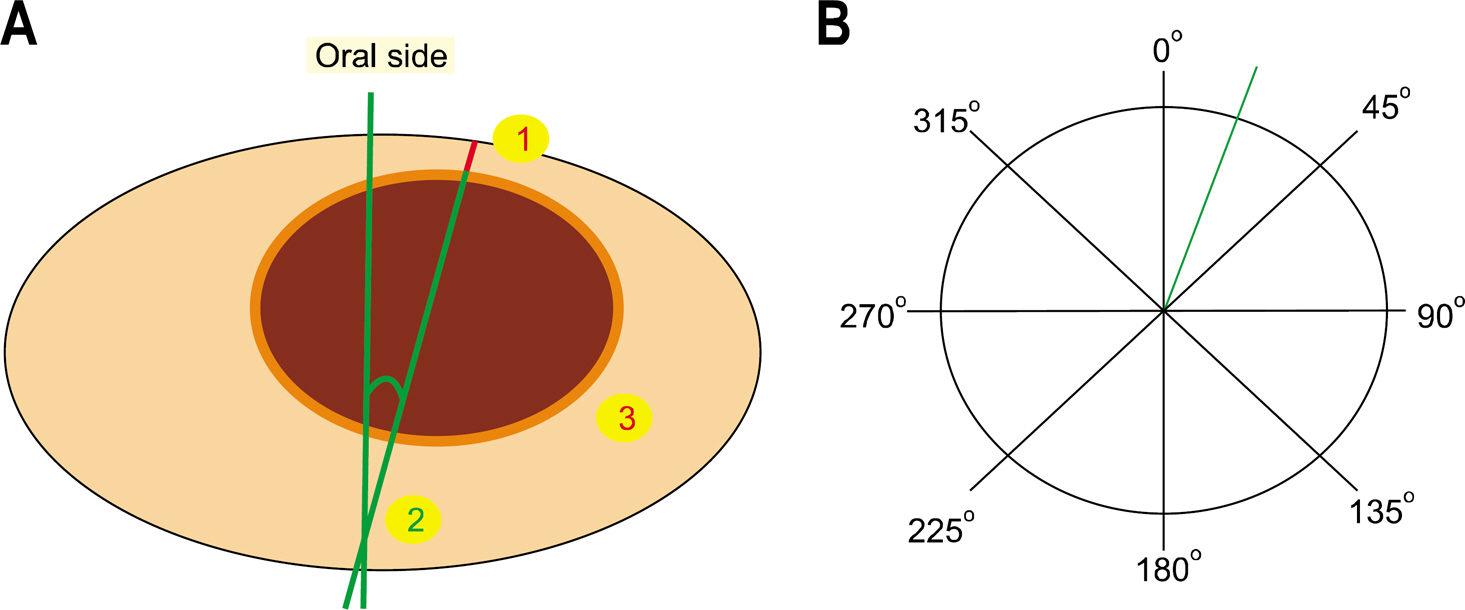
The correct pathologic review is very important after endoscopic submucosal dissection. The cut direction of specimen should be the right angle of the closest area between the lesion and the lateral margin for the correct pathologic review. The aim of this study was to evaluate the concordance of the gross finding and stereoscopic finding compared to the pathologic mapping in the setting of the cut direction.
METHODS
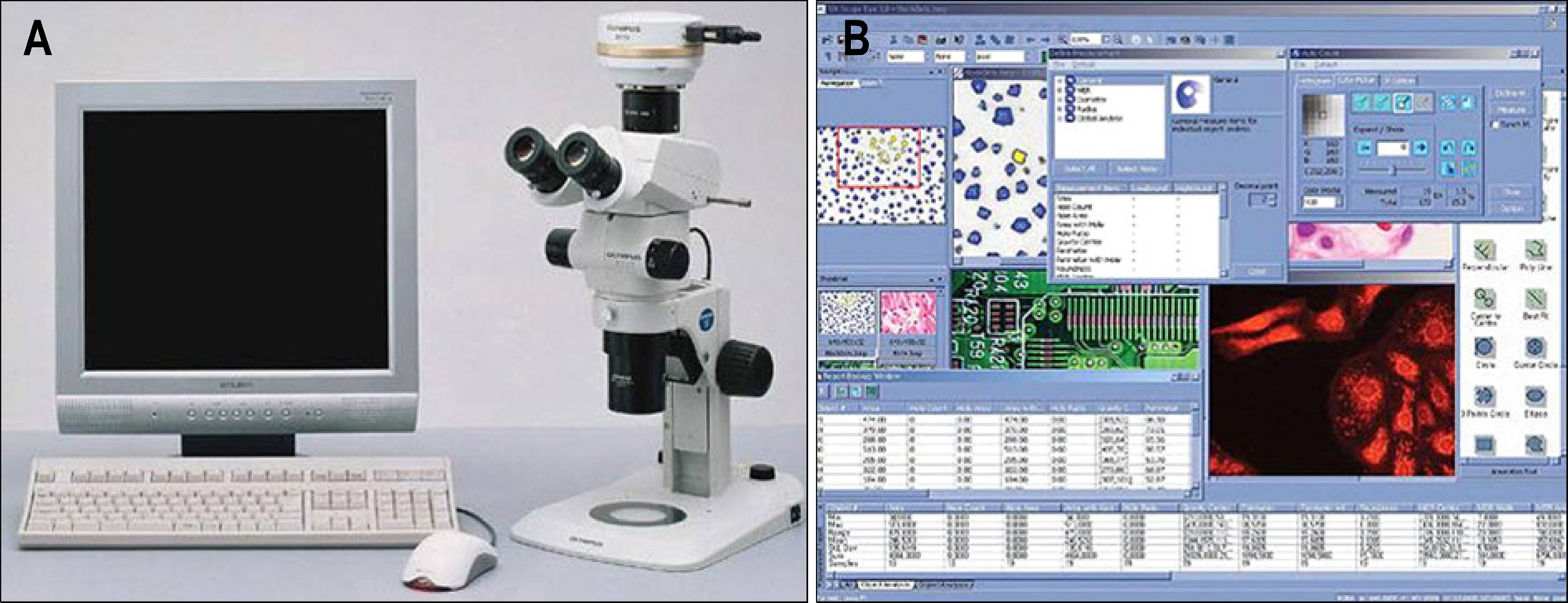
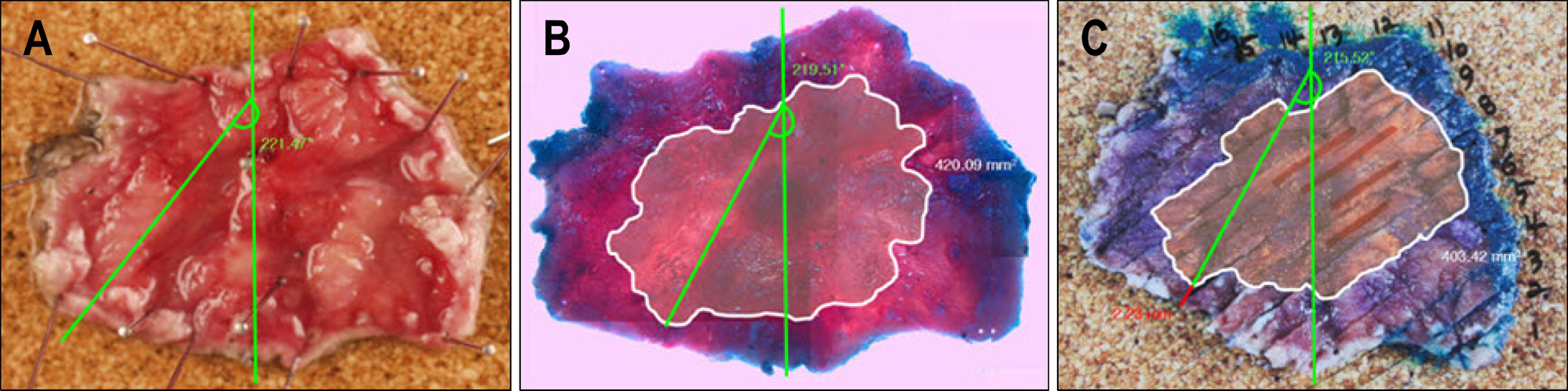
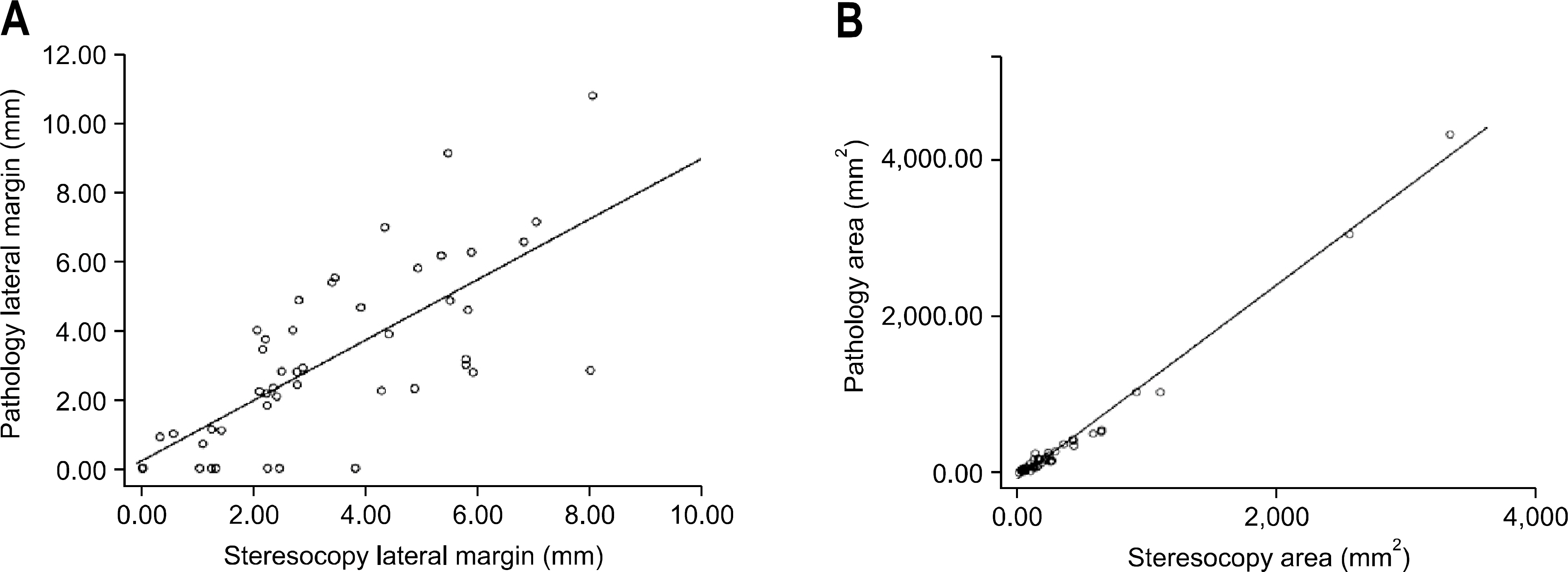
Between December 2008 and May 2009, the objects were 48 specimens in 46 patients who were diagnosed with early gastric cancer and high grade adenoma after endoscopic submucosal dissection. The specimens were stained with hematoxylin and observed by the stereoscopy and analyzed by the image analysis system. The cut direction was divided by an angle of 45 degree based on the oral side of the specimen, and the cut directions of the gross finding, the stereoscopic finding, and the pathologic finding were compared.
RESULTS
The concordance of the gross finding in the setting of the cut direction was 68% (33/48), and the kappa value was 0.626, and the concordance of the stereoscopic finding in the setting of the cut direction was 87% (33/48), and the kappa value was 0.874. The accuracy of the gross finding was significantly lower than that of the stereoscopic finding in the setting of the cut direction (p<0.05).
CONCLUSIONS
The endoscopist needs the careful observation and close attention in the setting of the cut direction of the specimen by gross finding, and stereoscopic analysis may be a useful tool for decision of the cut direction.
MeSH Terms
Figure
Cited by 1 articles
-
Clinicopathologic Characteristics of Patients Who Underwent Curative Additional Gastrectomy after Endoscopic Submucosal Dissection for Early Gastric Cancer or Adenoma
Hyejin Noh, Jong-Jae Park, Jae-Won Yun, Minjung Kwon, Dae Woong Yoon, Won Jin Chang, Ha Yong Oh, Moon Kyung Joo, Beom Jae Lee, Ji Hoon Kim, Jong Eun Yeon, Jae Seon Kim, Kwan Soo Byun, Young-Tae Bak
Korean J Gastroenterol. 2012;59(4):289-295. doi: 10.4166/kjg.2012.59.4.289.
Reference
-
1. Cho JY, Cho WY. The curren tstatus of endoscopic submucosal dissection. Korean J Gastrointest Endosc. 2008; 37:317–320.2. Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000; 3:219–225.
Article3. Kudo S, Hirota S, Nakajima T, et al. Colorectal tumors and pit pattern. J Clin Pathol. 1994; 47:880–885.4. Ryozawa S, Watanabe H, Abe M, Ajioka Y, Nishikura K, Okita K. Macroscopic and stereomicroscopic diagnosis of superficial flat-type early carcinomas of the gallbladder. J Gastroenterol. 1997; 32:635–642.
Article5. Miyamoto S, Muto M, Hamamoto Y, et al. A new technique for endoscopic mucosal resection with an insulated-tip elec-trosurgical knife improves the completeness of resection of intramucosal gastric neoplasms. Gastrointest Endosc. 2002; 55:576–581.
Article6. Ono H. Early gastric cancer: diagnosis, pathology, treatment techniques and treatment outcomes. Eur J Gastroenterol Hepatol. 2006; 18:863–866.
Article7. Yokoi C, Gotoda T, Hamanaka H, Oda I. Endoscopic submucosal dissection allows curative resection of locally recurrent early gastric cancer after prior endoscopic mucosal resection. Gastrointest Endosc. 2006; 64:212–218.
Article8. Iizuka T, Kikuchi D, Hoteya S, Yahagi N. The acetic acid + indigocarmine method in the delineation of gastric cancer. J Gastroenterol Hepatol. 2008; 23:1358–1361.9. Sumiyama K, Kaise M, Nakayoshi T, et al. Combined use of a magnifying endoscope with a narrow band imaging system and a multibending endoscope for en bloc EMR of early stage gastric cancer. Gastrointest Endosc. 2004; 60:79–84.
Article10. Oyama T, Tomori A, Hotta K. Efficacy of NBI system for the diagnosis of the lateral extension of superficial gastric cancer. Gastrointest Endosc. 2007; 65:AB162.
Article11. Osawa H, Yoshizawa M, Yamamoto H, et al. Optimal band imaging system can facilitate detection of changes in de-pressed-type early gastric cancer. Gastrointest Endosc. 2008; 67:226–234.
Article12. Mouri R, Yoshida S, Tanaka S, Oka S, Yoshihara M, Chayama K. Evaluation and validation of computed virtual chromoendoscopy in early gastric cancer. Gastrointest Endosc. 2009; 69:1052–1058.
Article13. Kawahara Y, Okada H, Kawano S, et al. New digital imaging technology i-scan for upper GI endoscopy: a pilot study. Gastrointest Endosc. 2009; 69:AB377.
Article14. Jin SY. Management and interpretation of specimen after endoscopic submucosal dissection of early gastric cancer. Korean J Gastrointest Endosc. 2007; 35(suppl):S188–S192.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Streoscopic Finding Valuable for the Pathologic Diagnosis of Endoscopic Submucosal Dissection Specimen?
- Pathology of Endoscopic Submucosal Dissection; How Do We Interpret?
- History and Development of Accessories for Endoscopic Submucosal Dissection
- Debates on Colorectal Endoscopic Submucosal Dissection - Traction for Effective Dissection: Gravity Is Enough
- Early Esophageal Cancer