Korean J Radiol.
2013 Dec;14(6):951-959. 10.3348/kjr.2013.14.6.951.
Is There Any Additional Benefit of Contrast-Enhanced CT as Part of Routine PET/CT Protocols for the Differentiation of Suspicious Incidental Gastrointestinal 2-Deoxy-18F-FDG Uptake?
- Affiliations
-
- 1Department of Radiology, Diagnostic and Interventional Radiology, University Hospital Tuebingen, Hoppe-Seyler-StraBe 3, 72076 Tuebingen, Germany. cornelia.brendle@med.uni-tuebingen.de
- 2Suedwestdeutsches PET-Zentrum, Diakonie Hospital Stuttgart, SeidenstraBe 47, 70174 Stuttgart, Germany.
- 3Department of Surgery, University Hospital Tuebingen, Hoppe-Seyler-StraBe 3, 72076 Tuebingen, Germany.
- 4Department of Radiology, Nuclear Medicine, University Hospital Tuebingen, Hoppe-Seyler-StraBe 3, 72076 Tuebingen, Germany.
- KMID: 1711463
- DOI: http://doi.org/10.3348/kjr.2013.14.6.951
Abstract
OBJECTIVE
Suspicious incidental gastrointestinal FDG uptake during positron-emission tomography/computed tomography (PET/CT) examinations can be caused by different diseases, including malignancies. However, differentiation with PET alone is difficult. The aim of this study was to investigate the potential of PET alone, contrast-enhanced CT (ceCT), and low-dose CT (ldCT) in routine PET/CT protocols for differentiation of incidental gastrointestinal lesions.
MATERIALS AND METHODS
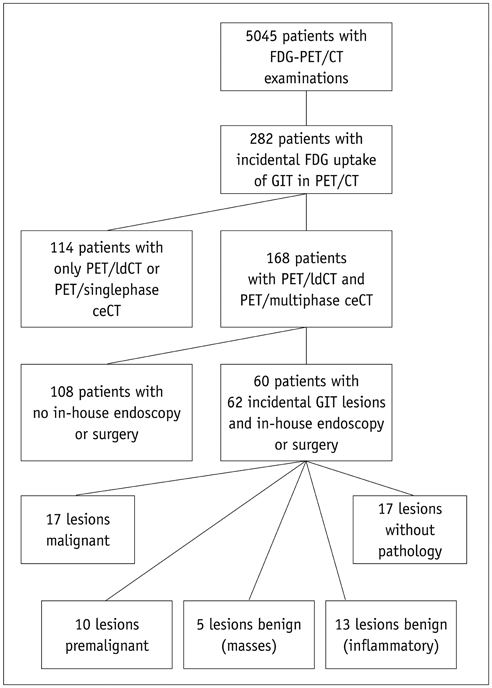
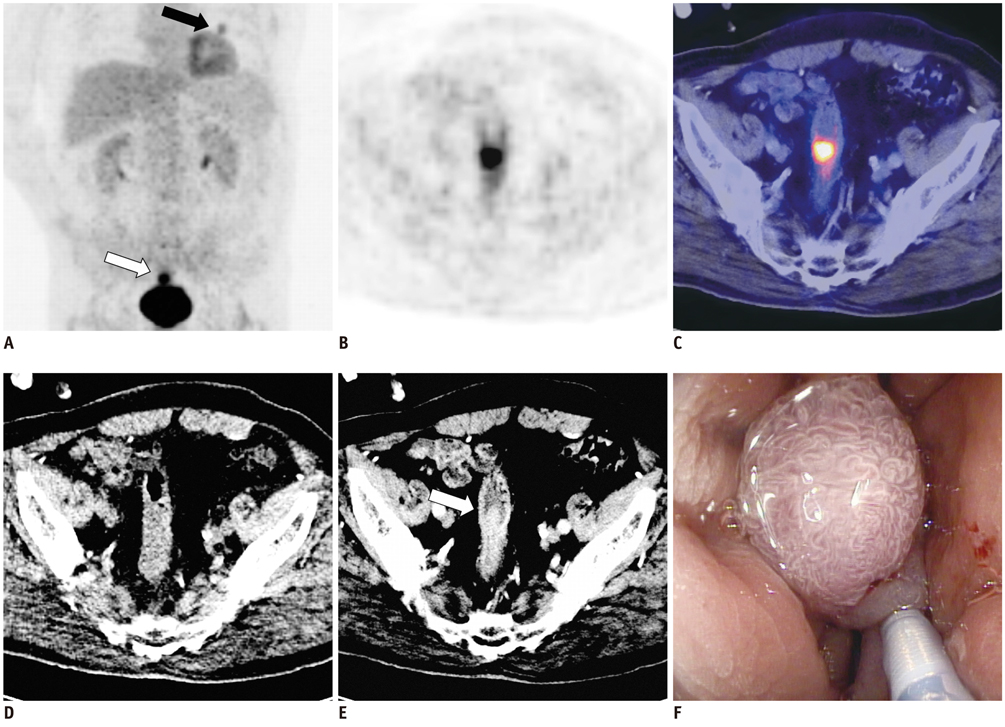
Sixty patients with incidental gastrointestinal lesions who underwent a routine PET/CT protocol with ldCT and ceCT were retrospectively analysed. The PET lesions were evaluated regarding their FDG uptake patterns and the standard uptake value. The anatomical correlates in both CT protocols were compared in regard to the correct lesion classification with the reference standard endoscopy.
RESULTS
Sixty-two lesions were found in 60 patients (17 malignant, 10 premalignant, 5 benign, 13 inflammatory, 17 physiological). The differentiation of the FDG uptake patterns did not enable reliable lesion classification. The positive predictive value for pathology was 0.81 for ceCT in PET/CT and 0.70 for ldCT. Malignancies were detected in 100% of the patients by ceCT vs. 29.4% by ldCT. The false negative rate of ceCT for all pathologies was 31.1%, vs. 68.9% for ldCT. False positive results (17/62) could not be excluded sufficiently by either CT protocol.
CONCLUSION
PET/ceCT protocols provide additional benefit especially in detecting gastrointestinal malignancies as a cause of suspicious incidental gastrointestinal FDG uptake. However, since follow-up endoscopy cannot be forgone due to the considerable false negative rate even with ceCT, the addition of ceCT to a routine PET/ldCT protocol cannot be recommended for this purpose.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Contrast Media/diagnostic use/pharmacokinetics
Female
Fluorodeoxyglucose F18/*diagnostic use/pharmacokinetics
Follow-Up Studies
Gastrointestinal Diseases/*diagnosis/metabolism
Gastrointestinal Tract/*metabolism/radiography/radionuclide imaging
Humans
Male
Middle Aged
Positron-Emission Tomography/*methods
Reproducibility of Results
Retrospective Studies
Tomography, X-Ray Computed/*methods
Contrast Media
Fluorodeoxyglucose F18
Figure
Reference
-
1. Israel O, Yefremov N, Bar-Shalom R, Kagana O, Frenkel A, Keidar Z, et al. PET/CT detection of unexpected gastrointestinal foci of 18F-FDG uptake: incidence, localization patterns, and clinical significance. J Nucl Med. 2005; 46:758–762.2. Kamel EM, Thumshirn M, Truninger K, Schiesser M, Fried M, Padberg B, et al. Significance of incidental 18F-FDG accumulations in the gastrointestinal tract in PET/CT: correlation with endoscopic and histopathologic results. J Nucl Med. 2004; 45:1804–1810.3. Gutman F, Alberini JL, Wartski M, Vilain D, Le Stanc E, Sarandi F, et al. Incidental colonic focal lesions detected by FDG PET/CT. AJR Am J Roentgenol. 2005; 185:495–500.4. Delbeke D. Oncological applications of FDG PET imaging: brain tumors, colorectal cancer, lymphoma and melanoma. J Nucl Med. 1999; 40:591–603.5. Engel H, Steinert H, Buck A, Berthold T, Huch Böni RA, von Schulthess GK. Whole-body PET: physiological and artifactual fluorodeoxyglucose accumulations. J Nucl Med. 1996; 37:441–446.6. Strauss LG. Fluorine-18 deoxyglucose and false-positive results: a major problem in the diagnostics of oncological patients. Eur J Nucl Med. 1996; 23:1409–1415.7. Abouzied MM, Crawford ES, Nabi HA. 18F-FDG imaging: pitfalls and artifacts. J Nucl Med Technol. 2005; 33:145–155. quiz 162-163.8. Tatlidil R, Jadvar H, Bading JR, Conti PS. Incidental colonic fluorodeoxyglucose uptake: correlation with colonoscopic and histopathologic findings. Radiology. 2002; 224:783–787.9. Ishimori T, Patel PV, Wahl RL. Detection of unexpected additional primary malignancies with PET/CT. J Nucl Med. 2005; 46:752–757.10. Drenth JP, Nagengast FM, Oyen WJ. Evaluation of (pre-) malignant colonic abnormalities: endoscopic validation of FDG-PET findings. Eur J Nucl Med. 2001; 28:1766–1769.11. Kei PL, Vikram R, Yeung HW, Stroehlein JR, Macapinlac HA. Incidental finding of focal FDG uptake in the bowel during PET/CT: CT features and correlation with histopathologic results. AJR Am J Roentgenol. 2010; 194:W401–W406.12. Prabhakar HB, Sahani DV, Fischman AJ, Mueller PR, Blake MA. Bowel hot spots at PET-CT. Radiographics. 2007; 27:145–159.13. Yasuda S, Fujii H, Nakahara T, Nishiumi N, Takahashi W, Ide M, et al. 18F-FDG PET detection of colonic adenomas. J Nucl Med. 2001; 42:989–992.14. van Kouwen MC, Nagengast FM, Jansen JB, Oyen WJ, Drenth JP. 2-(18F)-fluoro-2-deoxy-D-glucose positron emission tomography detects clinical relevant adenomas of the colon: a prospective study. J Clin Oncol. 2005; 23:3713–3717.15. Weston BR, Iyer RB, Qiao W, Lee JH, Bresalier RS, Ross WA. Ability of integrated positron emission and computed tomography to detect significant colonic pathology: the experience of a tertiary cancer center. Cancer. 2010; 116:1454–1461.16. Abdel-Nabi H, Doerr RJ, Lamonica DM, Cronin VR, Galantowicz PJ, Carbone GM, et al. Staging of primary colorectal carcinomas with fluorine-18 fluorodeoxyglucose whole-body PET: correlation with histopathologic and CT findings. Radiology. 1998; 206:755–760.17. Elstrom RL, Leonard JP, Coleman M, Brown RK. Combined PET and low-dose, noncontrast CT scanning obviates the need for additional diagnostic contrast-enhanced CT scans in patients undergoing staging or restaging for lymphoma. Ann Oncol. 2008; 19:1770–1773.18. Pfannenberg AC, Aschoff P, Brechtel K, Müller M, Klein M, Bares R, et al. Value of contrast-enhanced multiphase CT in combined PET/CT protocols for oncological imaging. Br J Radiol. 2007; 80:437–445.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Supraclavicular Lymph Node Metastasis from Various Malignancies: Assessment with 18F-Fluorodeoxyglucose Positron Emission Tomography/CT, Contrast-Enhanced CT and Ultrasound
- Colon Cancer Mimicking Physiologic FDG Uptake: with Using of Negative Oral Contrast
- A Comparison Study of Esophageal Findings on 18F-FDG PET/CT and Esophagogastroduodenoscopy
- Incidental Bilateral Renal Oncocytoma in a Patient with Metastatic Carcinoma of Unknown Primary: a Pitfall on 18F-FDG PET/CT
- Usefulness of Low Dose Oral Contrast Media in 18F-FDG PET/CT