Korean J Physiol Pharmacol.
2013 Oct;17(5):423-426. 10.4196/kjpp.2013.17.5.423.
Estrogen Rather Than Progesterone Cause Constipation in Both Female and Male Mice
- Affiliations
-
- 1Obesity-Diabetes Advanced Research Center, School of Medicine, Yeungnam University, Daegu 705-717, Korea. jykim@ynu.ac.kr
- KMID: 1500237
- DOI: http://doi.org/10.4196/kjpp.2013.17.5.423
Abstract
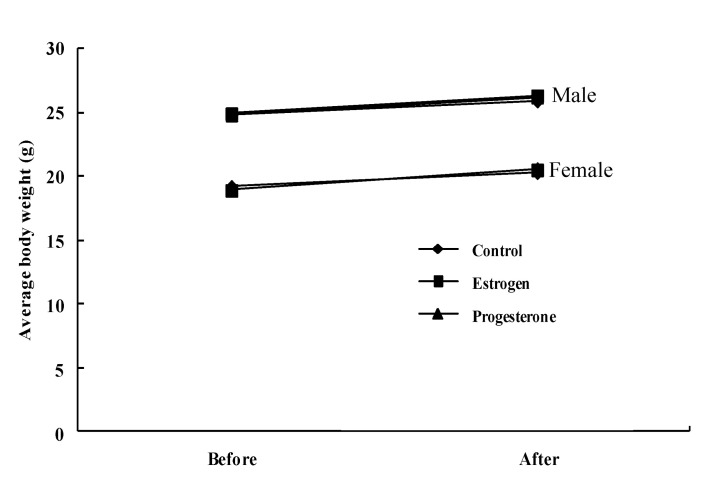
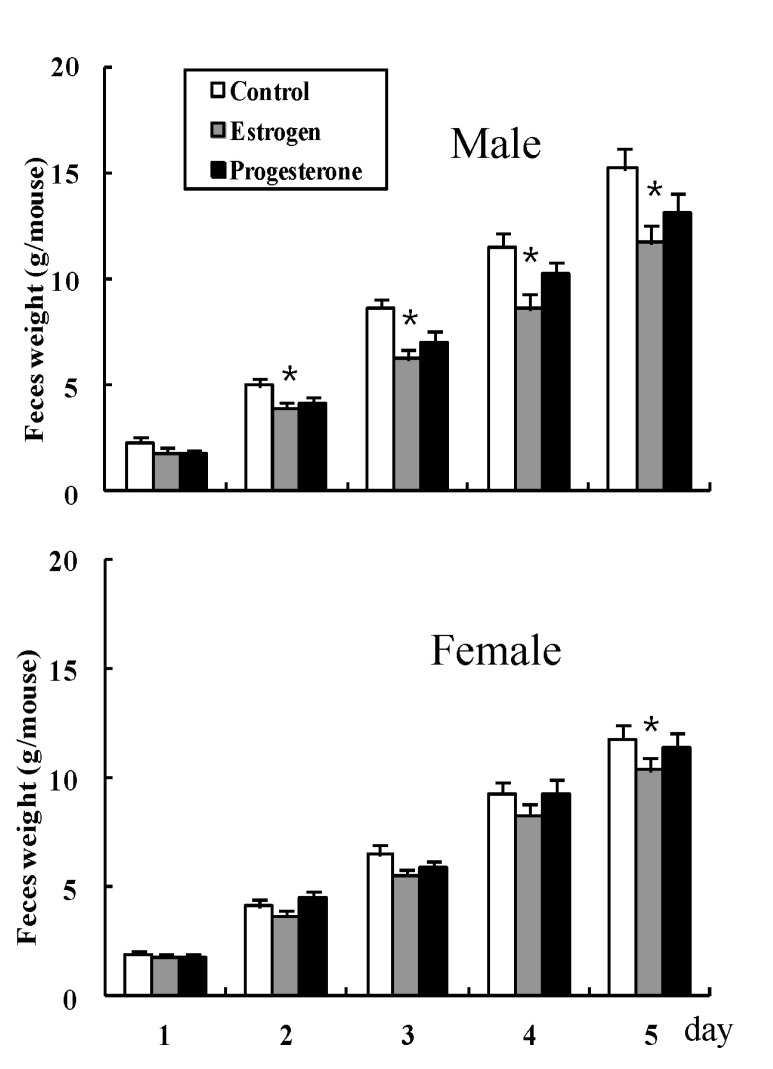
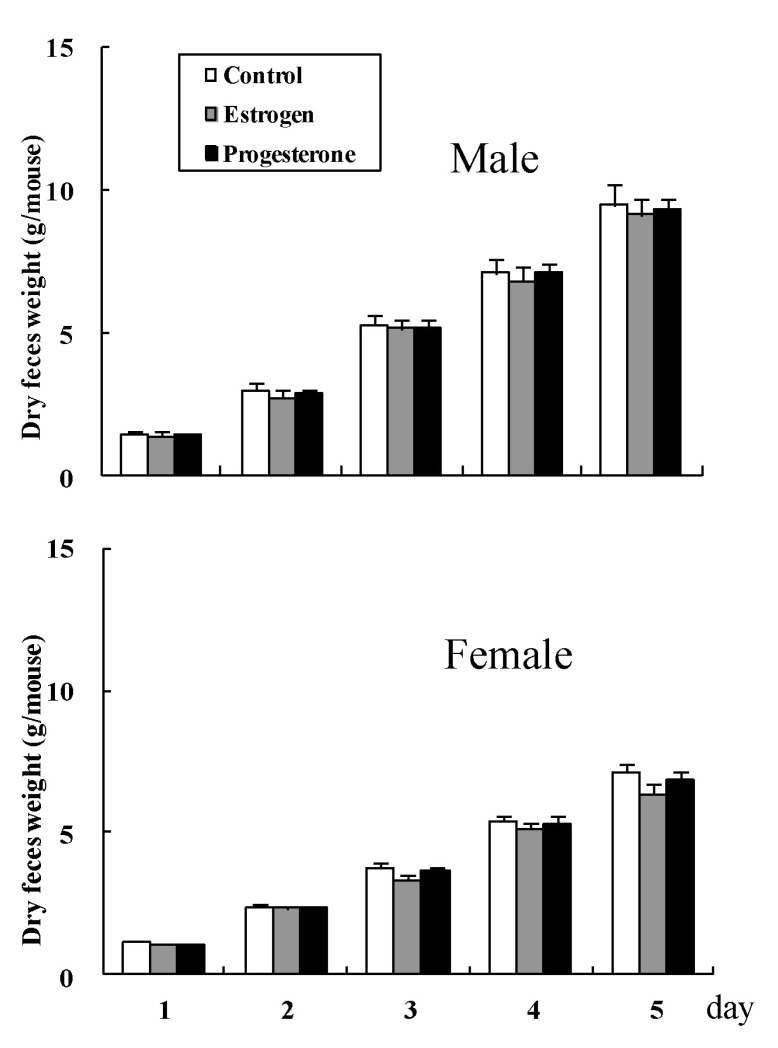
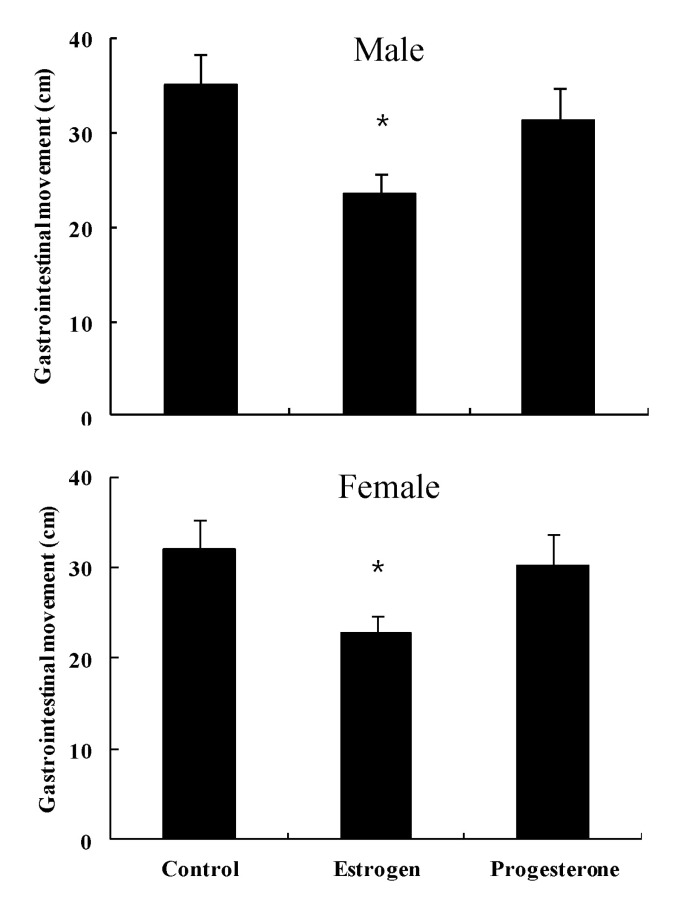
- Females are more often affected by constipation than males, especially during pregnancy, which is related to the menstrual cycle. Although still controversial, alterations of progesterone and estrogen may be responsible. Therefore, this study was conducted in order to determine whether the female sex steroid hormone itself is responsible for development of constipation in both female and male mice. Administration of estrogen resulted in a decrease in weight of accumulated feces on days 2, 3, 4, and 5 in male mice and on day 5 in female mice, compared with the control group, but progesterone administration did not. Administration of estrogen resulted in a decrease in gastrointestinal movement, compared to normal; however, no significant change was observed by administration of progesterone. In conclusion, estrogen, rather than progesterone, may be a detrimental factor of constipation via decreased bowel movement in mice.
Keyword
MeSH Terms
Figure
Reference
-
1. Chatoor D, Emmnauel A. Constipation and evacuation disorders. Best Pract Res Clin Gastroenterol. 2009; 23:517–530. PMID: 19647687.
Article2. Foxx-Orenstein AE, McNally MA, Odunsi ST. Update on constipation: one treatment does not fit all. Cleve Clin J Med. 2008; 75:813–824. PMID: 19068963.
Article3. Peppas G, Alexiou VG, Mourtzoukou E, Falagas ME. Epidemiology of constipation in Europe and Oceania: a systematic review. BMC Gastroenterol. 2008; 8:5. PMID: 18269746.
Article4. Chang L, Toner BB, Fukudo S, Guthrie E, Locke GR, Norton NJ, Sperber AD. Gender, age, society, culture, and the patient's perspective in the functional gastrointestinal disorders. Gastroenterology. 2006; 130:1435–1446. PMID: 16678557.
Article5. Wald A, Van Thiel DH, Hoechstetter L, Gavaler JS, Egler KM, Verm R, Scott L, Lester R. Effect of pregnancy on gastrointestinal transit. Dig Dis Sci. 1982; 27:1015–1018. PMID: 7140485.
Article6. Gill RC, Bowes KL, Kingma YJ. Effect of progesterone on canine colonic smooth muscle. Gastroenterology. 1985; 88:1941–1947. PMID: 3996847.
Article7. Shah S, Hobbs A, Singh R, Cuevas J, Ignarro LJ, Chaudhuri G. Gastrointestinal motility during pregnancy: role of nitrergic component of NANC nerves. Am J Physiol Regul Integr Comp Physiol. 2000; 279:R1478–R1485. PMID: 11004018.
Article8. Hutson WR, Roehrkasse RL, Wald A. Influence of gender and menopause on gastric emptying and motility. Gastroenterology. 1989; 96:11–17. PMID: 2909416.
Article9. Jung HK, Kim DY, Moon IH. Effects of gender and menstrual cycle on colonic transit time in healthy subjects. Korean J Intern Med. 2003; 18:181–186. PMID: 14619388.
Article10. Guyton AC, Hall JE. Textbook of medical physiology. 11th ed. Philadelphia: Elsevier Saunders;2006. p. 1013.11. Wald A, Van Thiel DH, Hoechstetter L, Gavaler JS, Egler KM, Verm R, Scott L, Lester R. Gastrointestinal transit: the effect of the menstrual cycle. Gastroenterology. 1981; 80:1497–1500. PMID: 7227774.
Article12. Madsen JL. Effects of gender, age, and body mass index on gastrointestinal transit times. Dig Dis Sci. 1992; 37:1548–1553. PMID: 1396002.13. Soffer EE, Kongara K, Achkar JP, Gannon J. Colonic motor function in humans is not affected by gender. Dig Dis Sci. 2000; 45:1281–1284. PMID: 10961704.14. Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999; 45(Suppl 2):II43–II47. PMID: 10457044.
Article15. Surrenti E, Rath DM, Pemberton JH, Camilleri M. Audit of constipation in a tertiary referral gastroenterology practice. Am J Gastroenterol. 1995; 90:1471–1475. PMID: 7661172.16. Knowles CH, Scott SM, Rayner C, Glia A, Lindberg G, Kamm MA, Lunniss PJ. Idiopathic slow-transit constipation: an almost exclusively female disorder. Dis Colon Rectum. 2003; 46:1716–1717. PMID: 14668603.
Article17. Preston DM, Lennard-Jones JE. Severe chronic constipation of young women: 'idiopathic slow transit constipation'. Gut. 1986; 27:41–48. PMID: 3949236.
Article18. Thomas ML, Xu X, Norfleet AM, Watson CS. The presence of functional estrogen receptors in intestinal epithelial cells. Endocrinology. 1993; 132:426–430. PMID: 8419141.
Article19. Ryan JP, Pellecchia D. Effect of progesterone pretreatment on guinea pig gallbladder motility in vitro. Gastroenterology. 1982; 83:81–83. PMID: 6281127.
Article20. Bruce LA, Behsudi FM. Differential inhibition of regional gastrointestinal tissue to progesterone in the rat. Life Sci. 1980; 27:427–434. PMID: 7412484.
Article21. Xiao ZL, Pricolo V, Biancani P, Behar J. Role of progesterone signaling in the regulation of G-protein levels in female chronic constipation. Gastroenterology. 2005; 128:667–675. PMID: 15765402.
Article22. Cong P, Pricolo V, Biancani P, Behar J. Abnormalities of prostaglandins and cyclooxygenase enzymes in female patients with slow-transit constipation. Gastroenterology. 2007; 133:445–453. PMID: 17681165.
Article23. Xiao ZL, Biancani P, Behar J. Effects of progesterone on motility and prostaglandin levels in the distal guinea pig colon. Am J Physiol Gastrointest Liver Physiol. 2009; 297:G886–G893. PMID: 20501437.
Article24. Kane SV, Sable K, Hanauer SB. The menstrual cycle and its effect on inflammatory bowel disease and irritable bowel syndrome: a prevalence study. Am J Gastroenterol. 1998; 93:1867–1872. PMID: 9772046.
Article25. Heitkemper MM, Cain KC, Jarrett ME, Burr RL, Hertig V, Bond EF. Symptoms across the menstrual cycle in women with irritable bowel syndrome. Am J Gastroenterol. 2003; 98:420–430. PMID: 12591063.
Article26. Celik AF, Turna H, Pamuk GE, Pamuk ON. How prevalent are alterations in bowel habits during menses? Dis Colon Rectum. 2001; 44:300–301. PMID: 11227952.27. Shah S, Nathan L, Singh R, Fu YS, Chaudhuri G. E2 and not P4 increases NO release from NANC nerves of the gastrointestinal tract: implications in pregnancy. Am J Physiol Regul Integr Comp Physiol. 2001; 280:R1546–R1554. PMID: 11294780.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immunohistochemical studies on the rate of positive reaction of estrogen receptors and progesterone receptors in the breast diseases
- Estrogen and progesterone receptors in normal and abnormal female reproductive tissues with EIA monoclonal assay
- Estrogen and Progesterone receptors in Meningioma
- Estrogen and progesterone receptors in the human fallopian tubes
- A Case of Estrogen and Progesterone Receptor-Positive Male Breast Cancer