Clin Exp Otorhinolaryngol.
2009 Mar;2(1):52-54. 10.3342/ceo.2009.2.1.52.
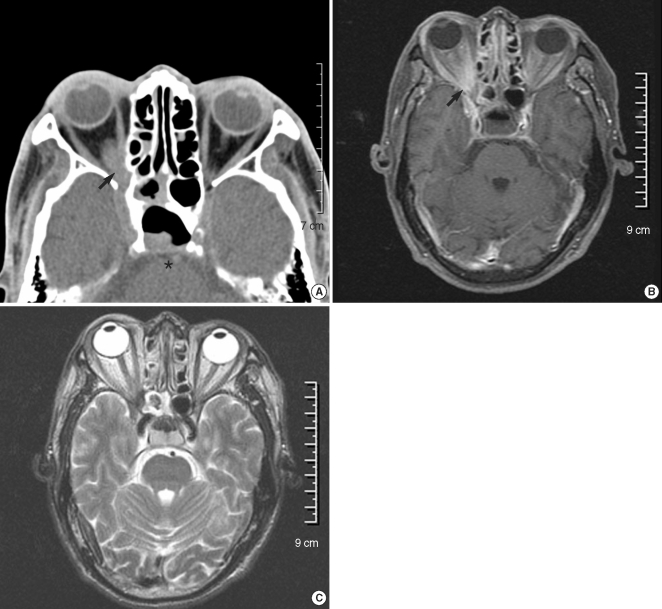
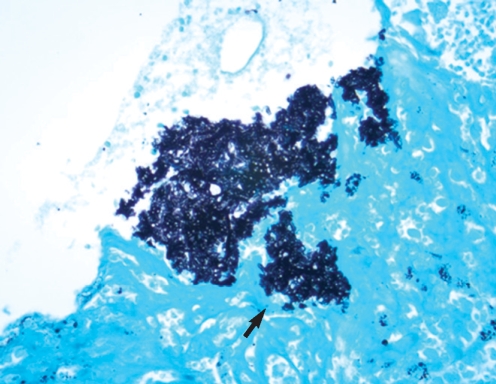
Orbital Apex Syndrome in a Patient with Sphenoid Fungal Balls
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, Hanyang University, Seoul, Korea. shcho@hanyang.ac.kr
- 2Department of Pathology, College of Medicine, Hanyang University, Seoul, Korea. shcho@hanyang.ac.kr
- 3Department of Ophthalmology, College of Medicine, Hanyang University, Seoul, Korea.
- 4Department of Neurosurgery, College of Medicine, Hanyang University, Seoul, Korea.
- KMID: 1466565
- DOI: http://doi.org/10.3342/ceo.2009.2.1.52
Abstract
- Orbital apex syndrome (OAS) is a rare disease that presents with a complex of symptoms, including ophthalmoplegia, ptosis and visual loss. Due to the poor prognosis, making a prompt diagnosis and administering the appropriate treatment must be initiated without delay if OAS is suspected. We report here on a case of a patient with sphenoid fungal balls, and he presented with acute visual loss and ophthalmoplegia.
Keyword
Figure
Cited by 1 articles
-
A Case of Optic Neuropathy Caused by Fungal Ball in an Onodi Cell
Young Soo Han, Chan Min Yang, Jae Ho Shin, In Ki Park
J Korean Ophthalmol Soc. 2014;55(3):426-431. doi: 10.3341/jkos.2014.55.3.426.
Reference
-
1. Yeh S, Foroozan R. Orbital apex syndrome. Curr Opin Ophthalmol. 2004; 12. 15(6):490–498. PMID: 15523194.
Article2. Tarazi AE, Shikani AH. Irreversible unilateral visual loss due to acute sinusitis. Arch Otolaryngol Head Neck Surg. 1991; 12. 117(12):1400–1401. PMID: 1845269.
Article3. Ferguson BJ. Fungus balls of the paranasal sinuses. Otolaryngol Clin North Am. 2000; 4. 33(2):389–398. PMID: 10736412.
Article4. Gungor A, Adusumilli V, Corey JP. Fungal sinusitis: progression of disease in immunosuppression-a case report. Ear Nose Throat J. 1998; 3. 77(3):207–210. 215PMID: 9557411.5. Pieroth L, Winterkorn JM, Schubert H, Millar WS, Kazim M. Concurrent sino-orbital aspergillosis and cerebral nocardiosis. J Neuroophthalmol. 2004; 6. 24(2):135–137. PMID: 15179067.
Article6. Thiagalingam S, Fernando GT, Tan K, O'Donnell BA, Weeks K, Branley M. Orbital apex syndrome secondary to Pseudallescheria boydii fungal sinusitis in an immunocompetent patient. Clin Experiment Ophthalmol. 2004; 10. 32(5):545–547. PMID: 15498073.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Orbital Apex Syndrome Caused by Mucocele in the Sphenoid Sinus
- Orbital Apex Syndrome Related to Isolated Sphenoid Fungal Sinusitis
- A Case of Rhino-orbital Mucormycoses with Orbital Apex Syndrome in Diabetic Patient
- Three Cases of Fungal Sinusitis with Orbital Complication
- A Case of Multiple Fungal Balls Involving the Isolated Three Sinuses