J Korean Surg Soc.
2009 Dec;77(Suppl):S5-S8. 10.4174/jkss.2009.77.Suppl.S5.
Laparoscopic Treatment of Paraesophageal Hernia Complicated with Gastric Volvulus
- Affiliations
-
- 1Division of Gastrointestinal Surgery, Department of Surgery, The Catholic University of Korea College of Medicine, Seoul, Korea. skygs@catholic.ac.kr
- KMID: 1464788
- DOI: http://doi.org/10.4174/jkss.2009.77.Suppl.S5
Abstract
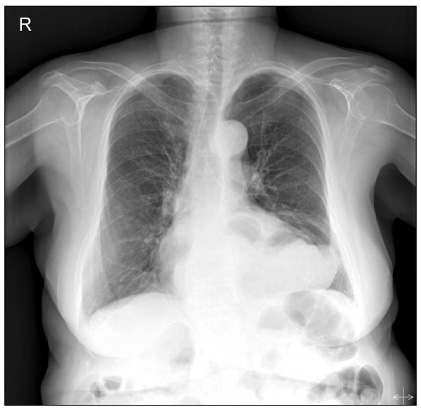
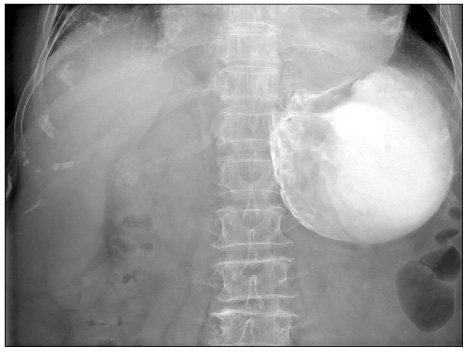
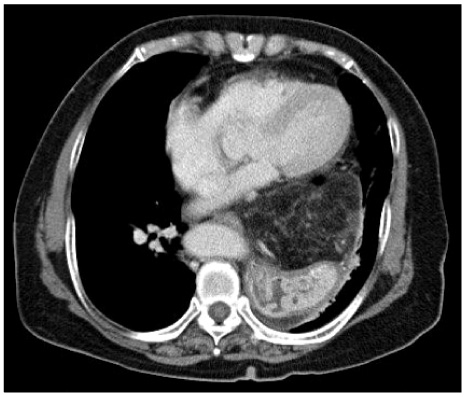
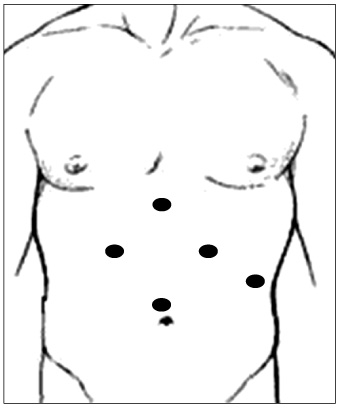
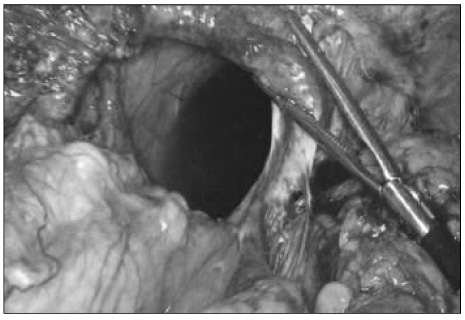
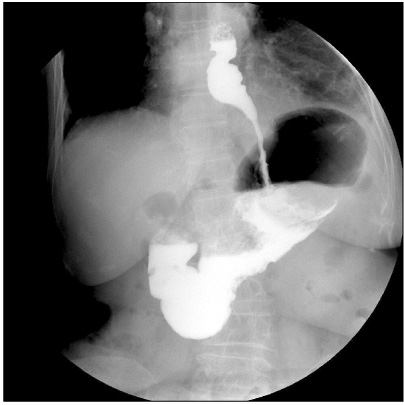
- Paraesophageal hernias are rare, accounting only for about 5% of all hiatal hernias but can sometimes lead to life-threatening complications such as bleeding, obstruction, incarceration, and strangulation. Accordingly, the surgical repair of paraesophageal hernia must be performed irrespectively of symptoms. Laparoscopic techniques of paraesophageal hernia offer several advantages compared with open techniques, including smaller incision, less traumatic handling of tissues, less postoperative pain. In this report, we describe a case of paraesophageal hernia complicated with gastric volvulus, which has been successfully repaired by the laparoscopic approach. A 79-year-old female was suffering from dysphagia, abdominal pain and intermittent vomiting for several months, and a paraesophageal hernia with partial gastric outlet obstruction due to gastric volvulus was diagnosed. The patient underwent the reduction of the hernia, dissection of the sac, crural repair and fundoplication via a laparoscopic approach. She recovered early and has been doing well on follow up with no recurrence.
Keyword
MeSH Terms
Figure
Reference
-
1. Hill LD, Tobias JA. Paraesophageal hernia. Arch Surg. 1968. 96:735–744.2. Larusson HJ, Zingg U, Hahnloser D, Delport K, Seifert B, Oertli D. Predictive factors for morbidity and mortality in patients undergoing laparoscopic paraesophageal hernia repair: age, ASA score and operation type influence morbidity. World J Surg. 2009. 33:980–985.3. Boushey RP, Moloo H, Burpee S, Schlachta CM, Poulin EC, Haggar F, et al. Laparoscopic repair of paraesophageal hernias: a Canadian experience. Can J Surg. 2008. 51:355–360.4. Draaisma WA, Gooszen HG, Tournoij E, Broeders IA. Controversies in paraesophageal hernia repair: a review of literature. Surg Endosc. 2005. 19:1300–1308.5. Bawahab M, Mitchell P, Church N, Debru E. Management of acute paraesophageal hernia. Surg Endosc. 2009. 23:255–259.6. Kim KC, Park HJ, Yoon DS, Chi HS, Lee WJ, Lee KS, et al. A case of paraesophageal hernia repaired by laparoscopic approach. Yonsei Med J. 1996. 37:151–157.7. Stair R, Olshaker J, Wehberg K. Paraesophageal hernia in an elderly woman with vomiting. J Emerg Med. 1999. 17:833–835.8. Skinner DB, Belsey RH. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg. 1967. 53:33–54.9. Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, et al. Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg. 2000. 190:553–561.10. Stylopoulos N, Gazelle GS, Rattner DW. Paraesophageal hernias: operation or observation? Ann Surg. 2002. 236:492–501.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mesenteroaxial Volvulus in the Stomach Associated with Paraesophageal Hernia: Case Report
- Pediatric gastric volvulus: experience with 7 cases
- A case of paraesophageal hernia repaired by laparoscopic approach
- 4 case of gastric volvulus complicated in diaphragmatic hernia
- A Case of Congenital Paraesophageal Hiatal Hernia in Infancy