Hanyang Med Rev.
2010 Aug;30(3):176-186. 10.7599/hmr.2010.30.3.176.
Status of Plasmodium vivax Malaria in the Republic of Korea after Reemergence
- Affiliations
-
- 1Department of Microbiology, Graduate School of Medicine, Gachon University of Medicine and Science, Incheon, Korea. jw.moses.park@gmail.com
- KMID: 1460252
- DOI: http://doi.org/10.7599/hmr.2010.30.3.176
Abstract
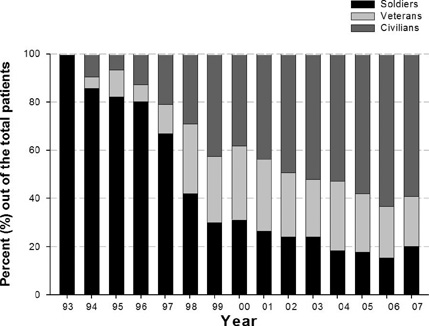
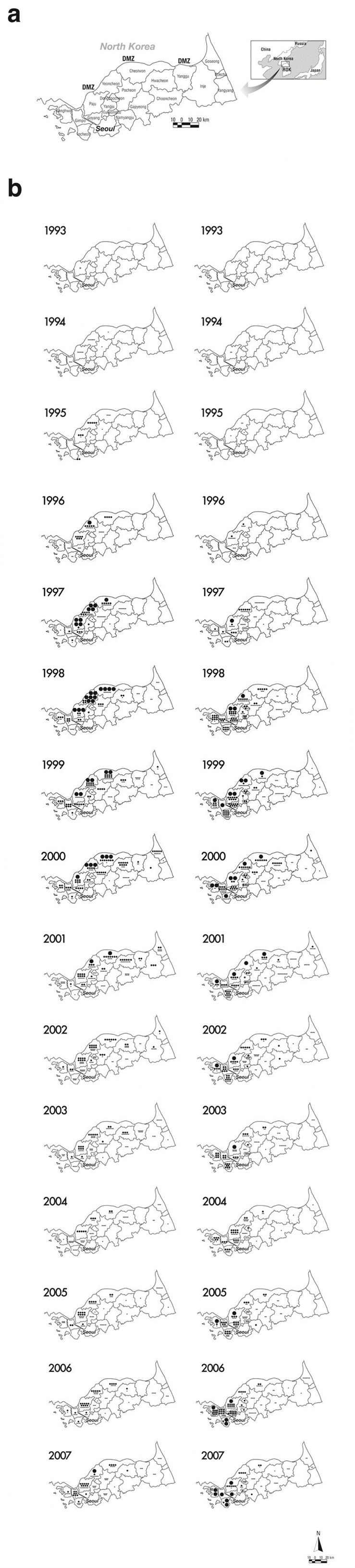
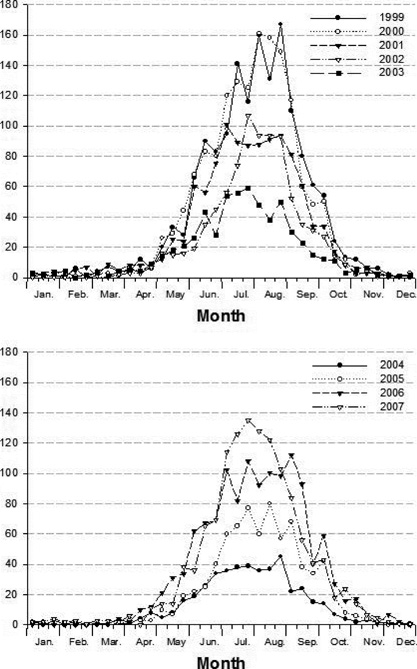
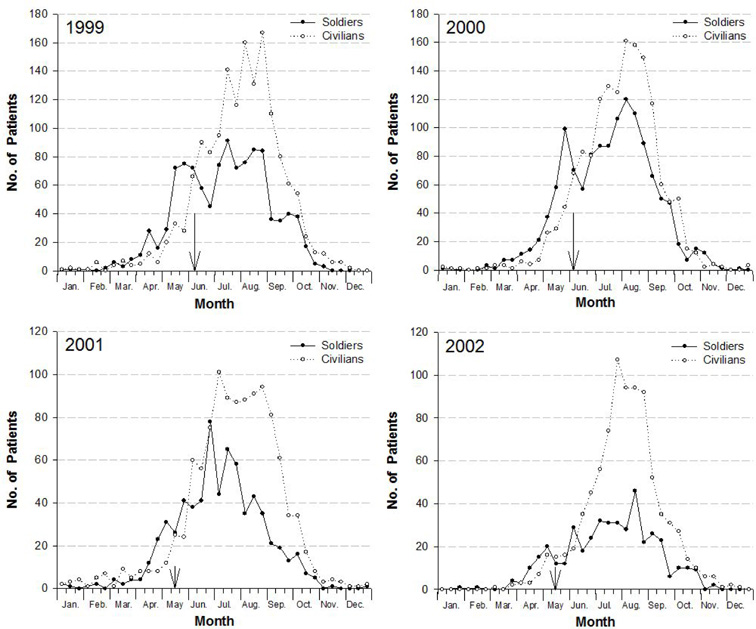
- The annual number of Plasmodium vivax malaria cases had rapidly increased since its reemergence in the Republic of Korea (ROK) in 1993 to reach more than 4,000 cases in 2000. Since 2001, it began to decrease to 864 cases in 2004, and once again increased to reach more than 2,000 cases by 2007. P. vivax malaria mainly has occurred in the areas adjacent to the Demilitarized Zone, which implies that current malaria occurrence in ROK has been strongly influenced by malaria situation of the Democratic People's Republic of Korea (DPRK). Besides the direct influence from DPRK, local transmission within ROK also likely occurred. Chemoprophylaxis performed in the ROK Army since 1997 has contributed to the reduction in cases among military personnel. However, many prophylactic failure cases due to the resistance to the prophylactic regimen have been reported since 2000 and two cases of chloroquine (CQ)-resistant P. vivax were reported, representing the first-known cases of CQ-resistant P. vivax from a temperate region of Asia. Delayed recrudescence, a kind of level I-resistance against CQ, has occurred frequently in DPRK. Continuous surveillance and monitoring are warranted to prevent further expansion of CQ-resistant P. vivax in ROK and DPRK.
Keyword
MeSH Terms
Figure
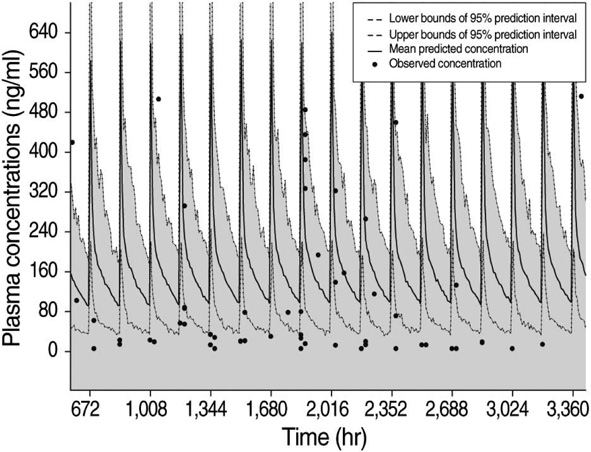
Cited by 2 articles
-
The Long and Short Incubation Periods of Plasmodium vivax Malaria in Korea: The Characteristics and Relating Factors
Sun-Ja Kim, Si-Heon Kim, Soo-Nam Jo, Jin Gwack, Seung-Ki Youn, Jae-Yeon Jang
Infect Chemother. 2013;45(2):184-193. doi: 10.3947/ic.2013.45.2.184.Clinical Characteristics of Vivax Malaria and Analysis of Recurred Patients
Yee Gyung Kwak, Hyo Keun Lee, Min Kim, Tae Hyun Um, Chong Rae Cho
Infect Chemother. 2013;45(1):69-75. doi: 10.3947/ic.2013.45.1.69.
Reference
-
1. Galinski MR, Barnwell JW. Plasmodium vivax: Merozoites, invasion of reticulocytes and considerations for malaria vaccine development. Parasitol Today. 1996. 12:20–29.
Article2. Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002. 415:680–685.
Article3. Hasegawa Y. Malaria in Korea. Chosen Igakkai Zasshi. 1913. 4:53–69.4. Hankey DD, Jones R Jr, Coatney GR, Alving AS, Coker WG, Garrison PL, Donovan WN. Korean vivax malaria. I. Natural history and response to chloroquine. Am J Trop Med Hyg. 1953. 2:958–969.5. Alving AS, Hankey DD, Coatney GR, Jones R Jr, Coker WG, Garrison PL, Donovan WN. Korean vivax malaria. II. Curative treatment with pamaquine and primaquine. Am J Trop Med Hyg. 1953. 2:970–976.6. World Health Organization. Synopsis of the world malaria situation in 1979. Wkly Epidemiol Rec. 1981. 56:145–149.7. Park JW, Klein TA, Lee HC, Pacha LA, Ryu SH, Yeom JS, Moon SH, Kim TS, Chai JY, Oh MD, Choe KW. Vivax malaria: a continuing health threat to the Republic of Korea. Am J Trop Med Hyg. 2003. 69:159–167.
Article8. Yeom JS, Ryu SH, Oh S, Lee WJ, Kim TS, Kim KH, Kim YA, Ahn SY, Cha JE, Park JW. Status of Plasmodium vivax malaria in the Republic of Korea during 2001-2003. Am J Trop Med Hyg. 2005. 73:604–608.
Article9. Yeom JS, Kim TS, Oh S, Sim JB, Barn JS, Kim HJ, Kim YA, Ahn SY, Shin MY, Yoo JA, Park JW. Plasmodium vivax malaria in the Republic of Korea during 2004-2005: changing patterns of infection. Am J Trop Med Hyg. 2007. 76:865–868.
Article10. Jun G, Yeom JS, Hong JY, Shin EH, Chang KS, Yu JR, Oh S, Chung H, Park JW. Resurgence of Plasmodium vivax malaria in the Republic of Korea during 2006-2007. Am J Trop Med Hyg. 2009. 81:605–610.
Article11. Yeom JS, Ryu SH, Oh S, Choi DH, Song KJ, Oh YH, Lee JH, Kim YA, Ahn SY, Yang HY, Cha JE, Park JW. Evaluation of anti-malarial effects of mass chemoprophylaxis in the Republic of Korea Army. J Korean Med Sci. 2005. 20:707–712.
Article12. Park JW, Jun G, Yeom JS. Plasmodium vivax malaria: status in the Republic of Korea following reemergence. Korean J Parasitol. 2009. 47:Suppl. S39–S50.13. Lim HS, Im JS, Cho JY, Bae KS, Klein TA, Yeom JS, Kim TS, Choi JS, Jang IJ, Park JW. Pharmacokinetics of Hydroxychloroquine and Its Clinical Implications in Chemoprophylaxis against Malaria Caused by Plasmodium vivax. Antimicrob Agents Chemother. 2009. 53:1468–1475.
Article14. Lee KS, Kim TH, Kim ES, Lim HS, Yeom JS, Jun G, Park JW. Short report: chloroquine-resistant Plasmodium vivax in the Republic of Korea. Am J Trop Med Hyg. 2009. 80:215–217.15. Park JW, Kim KH, Jung YJ, Bae I, Yeom JS. Status of vivax malaria in North Korea. Korean Unific Health Care. 2007. 6:31–58.