J Korean Assoc Oral Maxillofac Surg.
2010 Aug;36(4):314-319. 10.5125/jkaoms.2010.36.4.314.
Retropharyngeal space abscess due to spread of odontogenic infection: two cases report
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Busan Paik Hospital, College of Medicine, Inje University, Busan, Korea. dwjty@hanmail.net
- KMID: 1457785
- DOI: http://doi.org/10.5125/jkaoms.2010.36.4.314
Abstract
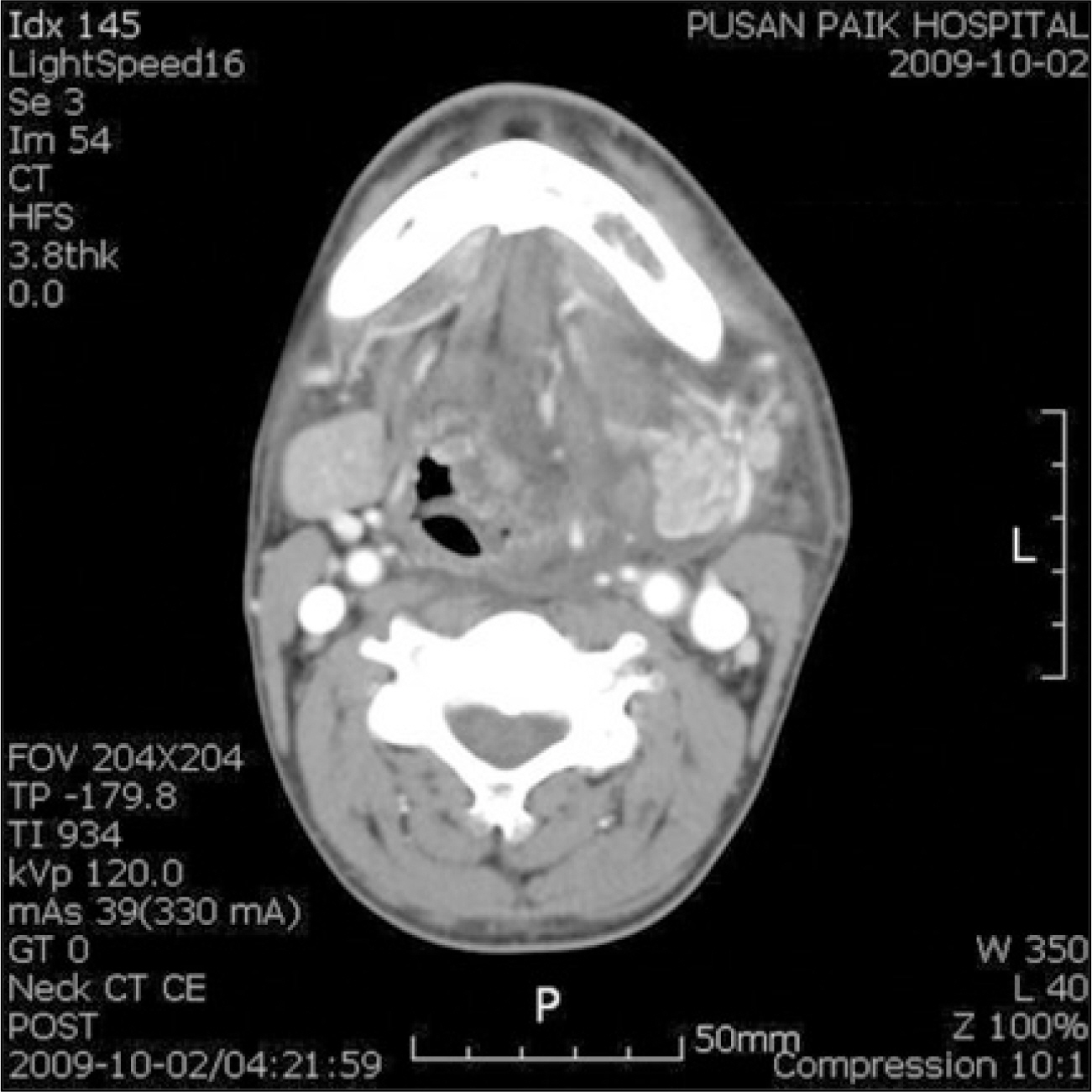
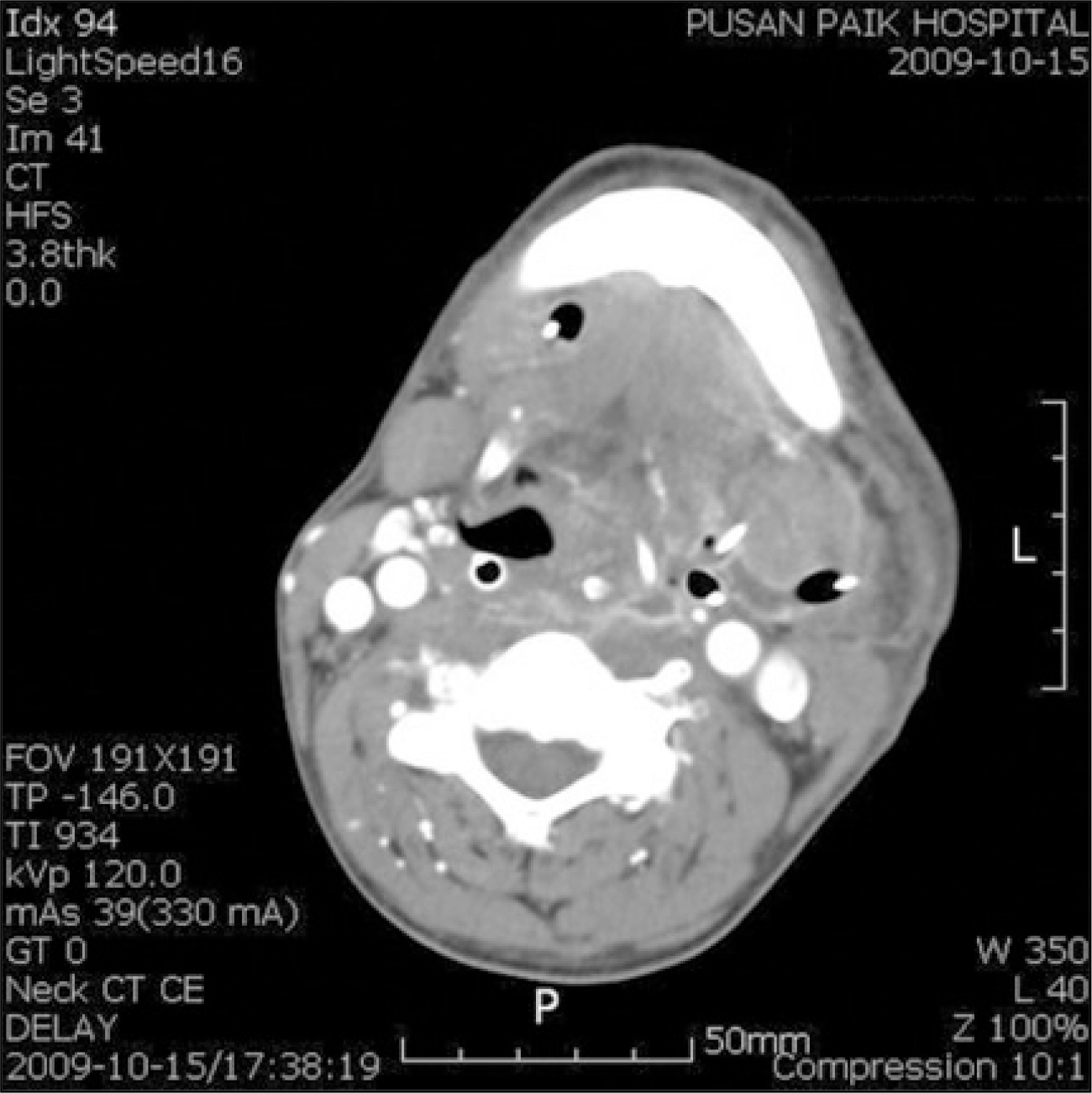
- Odontogenic infections are a normally locally confined, self-limiting process that is easily treated by antibiotic therapy and local surgical treatment. However, it may spread into the surrounding tissues through a perforation of the bone, and into contiguous fascial spaces or planes like the primary or secondary fascial spaces. If the infection extends widely, it may spread into the lateral pharyngeal and retropharyngeal space. The retropharyngeal space is located posterior to the pharynx. If an odontogenic infection spreads into this space, severe life-threatening complications will occur, such as airway obstruction, mediastinitis, pericarditis, pleurisy, pulmonary abscess, aspiration pneumonia and hematogenous dissemination to the distant organs. The mortality rate of mediastinitis ranges from 35% to 50%. Therefore, a rapid evaluation and treatment are essential for treating retropharyngeal space abscesses and preventing severe complications. Recently, we encountered two cases of a retropharyngeal space abscess due to the spread of an odontogenic infection. In all patients, early diagnosis was performed by computed tomography scanning and a physical examination. All patients were treated successfully by extensive surgical and antibiotic therapy.
MeSH Terms
Figure
Reference
-
References
1. The Korean Association of Oral and Maxillofacial Surgeons. Textbook of oral and maxillofacial surgery. 2nd ed.Seoul: Dental and Medical Publishing;2005.2. Bonapart IE, Stevens HP, Kerver AJ, Rietveld AP. Rare complications of an odontogenic abscess: mediastinitis, thoracic empyema and cardiac tamponade. J Oral Maxillofac Surg. 1995; 53:610–3.3. Haug RH, Picard U, Indresano AT. Diagnosis and treatment of the retropharyngeal abscess in adults. Br J Oral Maxillofac Surg. 1990; 28:34–8.
Article4. Flynn TR. The swollen face. Severe odontogenic infections. Emerg Med Clin North Am. 2000; 18:481–519.5. Peterson LJ. Principles of management and prevention of odontogenic infections. Peterson LJ, Ellis III E, Hupp JR, Tucker MR, editors. Contemporary oral and maxillofacial surgery. 4th ed.St. Louis, Missouri: Mosby;2003. p. 344–65.6. Park MS, Kim CL, Lee SH, Jung JS, Jeong JC, Kim KJ, et al. Retropharyngeal and mediastinal abscess secondary to odontogenic infections. J Korean Assoc Maxillofac Plast Reconstr Surg. 1996; 18:626–35.7. Stefanopoulos PK, Kolokotronis AE. The clinical significance of anaerobic bacteria in acute orofacial odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:398–408.
Article8. Kim IK, Youn SH, Oh SS, Choi JH, Oh NS, Kim ES, et al. A study of microorganisms in oral and maxillofacial infected patients. J Korean Assoc Maxillofac Plast Reconstr Surg. 2000; 22:420–9.9. Walton RE. Culturing the exudate of an odontogenic infection-a useful procedure? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:525.10. Limeres J, Toma ′ s I, Alvarez M, Diz P. Empirical antimicrobial therapy for odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 100:263–4.
Article11. Kuriyama T, Karasawa T, Nakagawa K, Saiki Y, Yamamoto E, Nakamura S. Bacteriologic features and antimicrobial susceptibility in isolates from orofacial odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90:600–8.
Article12. Kim MS, Nam OH, Kim SG, Cho SI. A clinicostatistical analysis of oral and maxillofacial infected patients. J Korean Assoc Maxillofac Plast Reconstr Surg. 2002; 24:317–24.13. Bryan CS, King BG Jr, Bryant RE. Retropharyngeal infection in adults. Arch Intern Med. 1974; 134:126–30.
Article14. Lee WH, Ahn KM, Jang BY, Ahn MR, Lee JY, Sohn DS. Clinicostatistical study of inpatients of abscess in fascial spaces for the last 5 years. J Korean Assoc Oral Maxillofac Surg. 2004; 30:497–503.15. Laskin DM. Systemic effects of oral infections: a possible preventive role for the oral and maxillofacial surgeon. J Oral Maxillofac Surg. 2001; 59:853.
Article16. Peters ES, Fong B, Wormuth DW, Sonis ST. Risk factors affecting hospital length of stay in patients with odontogenic maxillofacial infections. J Oral Maxillofac Surg. 1996; 54:1386–91.
Article17. Rubin MM, Cozzi GM. Fatal necrotizing mediastinitis as a complication of an odontogenic infection. J Oral Maxillofac Surg. 1987; 45:529–33.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deep Neck Space Infection Caused by Keratocystic Odontogenic Tumor
- A Case of Second Branchial Cyst in Retropharyngeal Space, Appearing as Dyspnea and Dysphagia
- The various orbital infections from odontogenic origin
- A Case of Retropharyngeal Abscess and Mediastinal Abscess with Dyspnea
- Headache in the Retropharyngeal Abscess: A case report