Korean J Radiol.
2010 Dec;11(6):627-631. 10.3348/kjr.2010.11.6.627.
Abnormal Motion of the Interventricular Septum after Coronary Artery Bypass Graft Surgery: Comprehensive Evaluation with MR Imaging
- Affiliations
-
- 1Department of Radiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan 682-714, Korea.
- 2Division of Cardiovascular Imaging, Department of Radiology, Seoul National University Bundang Hospital, Gyeonggi-do 463-707, Korea. drsic@radiol.snu.ac.kr
- 3Department of Internal Medicine, Division of Cardiology, Seoul National University Bundang Hospital, Gyeonggi-do 463-707, Korea.
- 4Departments of Thoracic and Cardiovascular Surgery and Radiology, Seoul National University Bundang Hospital, Gyeonggi-do 463-707, Korea.
- 5Department of Internal Medicine, Division of Cardiology, Ulsan University Hospital, Ulsan 682-714, Korea.
- 6Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- KMID: 1119225
- DOI: http://doi.org/10.3348/kjr.2010.11.6.627
Abstract
OBJECTIVE
To define the mechanism associated with abnormal septal motion (ASM) after coronary artery bypass graft surgery (CABG) using comprehensive MR imaging techniques.
MATERIALS AND METHODS
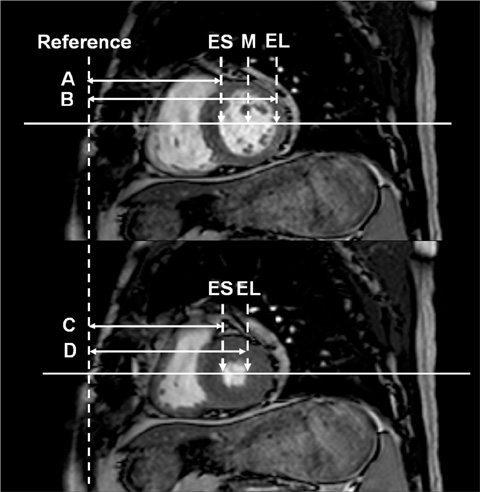
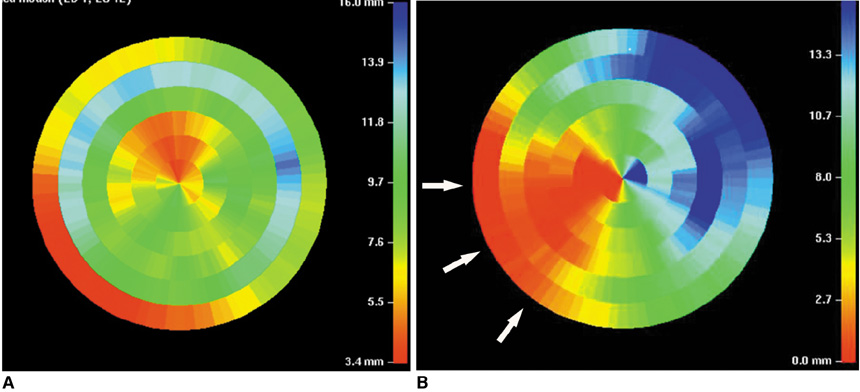
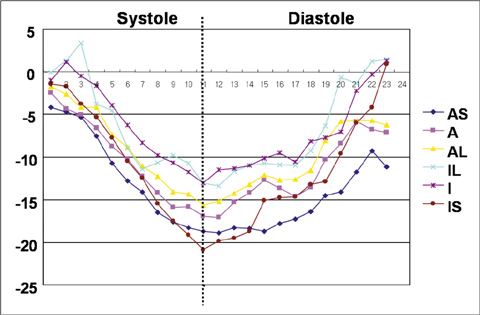
Eighteen patients (mean age, 58 +/- 12 years; 15 males) were studied with comprehensive MR imaging using rest/stress perfusion, rest cine, and delayed enhancement (DE)-MR techniques before and after CABG. Myocardial tagging was also performed following CABG. Septal wall motion was compared in the ASM and non-ASM groups. Preoperative and postoperative results with regard to septal wall motion in the ASM group were also compared. We then analyzed circumferential strain after CABG in both the septal and lateral walls in the ASM group.
RESULTS
All patients had normal septal wall motion and perfusion without evidence of non-viable myocardium prior to surgery. Postoperatively, ASM at rest and/or stress state was documented in 10 patients (56%). However, all of these had normal rest/stress perfusion and DE findings at the septum. Septal wall motion after CABG in the ASM group was significantly lower than that in the non-ASM group (2.1+/-5.3 mm vs. 14.9+/-4.7 mm in the non-ASM group; p < 0.001). In the ASM group, the degree of septal wall motion showed a significant decrease after CABG (preoperative vs. postoperative = 15.8+/-4.5 mm vs. 2.1+/-5.3 mm; p = 0.007). In the ASM group after CABG, circumferential shortening of the septum was even larger than that of the lateral wall (-20.89+/-5.41 vs. -15.41+/-3.7, p < 0.05)
CONCLUSION
Abnormal septal motion might not be caused by ischemic insult. We suggest that ASM might occur due to an increase in anterior cardiac mobility after incision of the pericardium.
Keyword
MeSH Terms
-
Contrast Media/diagnostic use
*Coronary Artery Bypass
Coronary Disease/*surgery
Female
Gadolinium DTPA/diagnostic use
Humans
Image Interpretation, Computer-Assisted
Magnetic Resonance Imaging/*methods
Male
Middle Aged
Pericardium/surgery
Retrospective Studies
Statistics, Nonparametric
Ventricular Septum/*physiopathology
Figure
Cited by 1 articles
-
Echocardiographic Investigation of the Mechanism Underlying Abnormal Interventricular Septal Motion after Open Heart Surgery
Min-Kyung Kang, Hyuk-Jae Chang, In Jeong Cho, Sanghoon Shin, Chi-Young Shim, Geu-Ru Hong, Kyung-Jong Yu, Byung-Chul Chang, Namsik Chung
J Cardiovasc Ultrasound. 2014;22(1):8-13. doi: 10.4250/jcu.2014.22.1.8.
Reference
-
1. Otto C. Textbook of clinical echocardiography. 2004. 3rd ed. Philadelphia, PA: Saunders;154.2. Schroeder E, Marchandise B, Schoevaerdts JC, Kremer R. Paradoxical ventricular septal motion after cardiac surgery. Analysis of M-mode echocardiograms and follow-up in 324 patients. Acta Cardiol. 1985. 40:315–324.3. Reynolds HR, Tunick PA, Grossi EA, Dilmanian H, Colvin SB, Kronzon I. Paradoxical septal motion after cardiac surgery: a review of 3,292 cases. Clin Cardiol. 2007. 30:621–623.4. De Nardo D, Caretta Q, Mercanti C, Alessandri N, Scibilia G, Chiavarelli R, et al. Effects of uncomplicated coronary artery bypass graft surgery on global and regional left ventricular function at rest. Study by equilibrium radionuclide angiocardiography. Cardiology. 1989. 76:285–292.5. Wranne B, Pinto FJ, Siegel LC, Miller DC, Schnittger I. Abnormal postoperative interventricular motion: new intraoperative transesophageal echocardiographic evidence supports a novel hypothesis. Am Heart J. 1993. 126:161–167.6. Righetti A, Crawford MH, O'Rourke RA, Schelbert H, Daily PO, Ross J Jr. Interventricular septal motion and left ventricular function after coronary bypass surgery: evaluation with echocardiography and radionuclide angiography. Am J Cardiol. 1977. 39:372–377.7. Yoshida K, Yoshikawa J, Kato H, Yanagihara K, Takagi Y, Okumachi F, et al. Pericardial closure causing post-operative abnormal septal motion: an echocardiographic study during cardiac surgery. J Cardiogr. 1983. 13:359–370. [Japanese].8. Schnittger I, Keren A, Yock PG, Allen MD, Modry DL, Zusman DR, et al. Timing of abnormal interventricular septal motion after cardiopulmonary bypass operations. Lack of injury proved by preoperative, intraoperative, and postoperative echocardiography. J Thorac Cardiovasc Surg. 1986. 91:619–623.9. Chang SA, Chang HJ, Choi SI, Chun EJ, Yoon YE, Kim HK, et al. Usefulness of left ventricular dyssynchrony after acute myocardial infarction, assessed by a tagging magnetic resonance image derived metric, as a determinant of ventricular remodeling. Am J Cardiol. 2009. 104:19–23.10. Choi SI, Kang JW, Chun EJ, Choi SH, Lim TH. High-resolution diffusion tensor MR imaging for evaluating myocardial anisotropy and fiber tracking at 3T: the effect of the number of diffusion-sensitizing gradient directions. Korean J Radiol. 2010. 11:54–59.11. Giubbini R, Rossini P, Bertagna F, Bosio G, Paghera B, Pizzocaro C, et al. Value of gated SPECT in the analysis of regional wall motion of the interventricular septum after coronary artery bypass grafting. Eur J Nucl Med Mol Imaging. 2004. 31:1371–1377.12. Burggraf GW, Craige E. Echocardiographic studies of left ventricular wall motion and dimensions after valvular heart surgery. Am J Cardiol. 1975. 35:473–480.13. Eslami B, Roitman D, Karp RB, Sheffield LT. The echocardiogram after pericardiectomy. Jpn Heart J. 1979. 20:1–5.14. Connolly HM, Click RL, Schattenberg TT, Seward JB, Tajik AJ. Congenital absence of the pericardium: echocardiography as a diagnostic tool. J Am Soc Echocardiogr. 1995. 8:87–92.15. Joshi SB, Salah AK, Mendoza DD, Goldstein SA, Fuisz AR, Lindsay J. Mechanism of paradoxical ventricular septal motion after coronary artery bypass grafting. Am J Cardiol. 2009. 103:212–215.16. Okada RD, Murphy JH, Boucher CA, Pohost GM, Strauss HW, Johnson G 3rd, et al. Relationship between septal perfusion, viability, and motion before and after coronary artery bypass surgery. Am Heart J. 1992. 124:1190–1195.17. Toyoda T, Akasaka T, Watanabe N, Akiyama M, Neishi Y, Kume T, et al. Evaluation of abnormal motion of interventricular septum after coronary artery bypass grafting operation: assessment by ultrasonic strain rate imaging. J Am Soc Echocardiogr. 2004. 17:711–716.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anatomy of the septal perforating arteries of the heart
- Assessment of Coronary Artery Bypass Graft Patency Using Three Dimensional Coronary Angiography by Electron Beam Tomography
- The Right Gastroepiploic Artery Graft for Coronary Artery Bypass Grafting: A 30-Year Experience
- Assessment of Patency of Coronary Artery Bypass Grafts Using Segmented K-space Breath-hold Cine Cardiovascular Magnetic Resonance Imaging: A Clinical Feasibility Study
- Noninvasive Evaluation of Coronary Artery Bypass Graft Patency by Electron Beam Tomography