Korean J Radiol.
2004 Sep;5(3):185-198. 10.3348/kjr.2004.5.3.185.
Radiofrequency Ablation of Liver Cancer: Early Evaluation of Therapeutic Response with Contrast-Enhanced Ultrasonography
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. hklim@smc.samsung.co.kr
- KMID: 1118824
- DOI: http://doi.org/10.3348/kjr.2004.5.3.185
Abstract
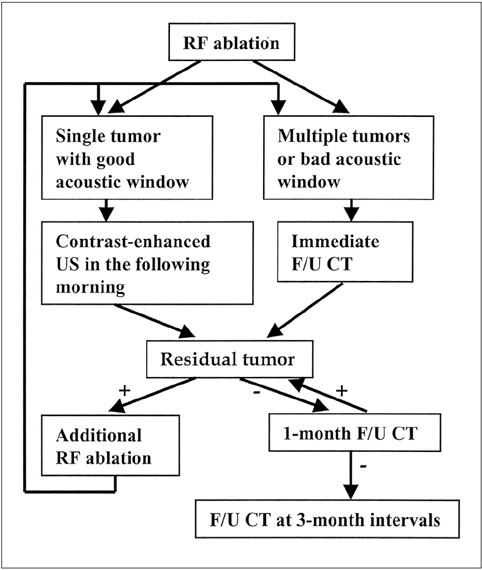
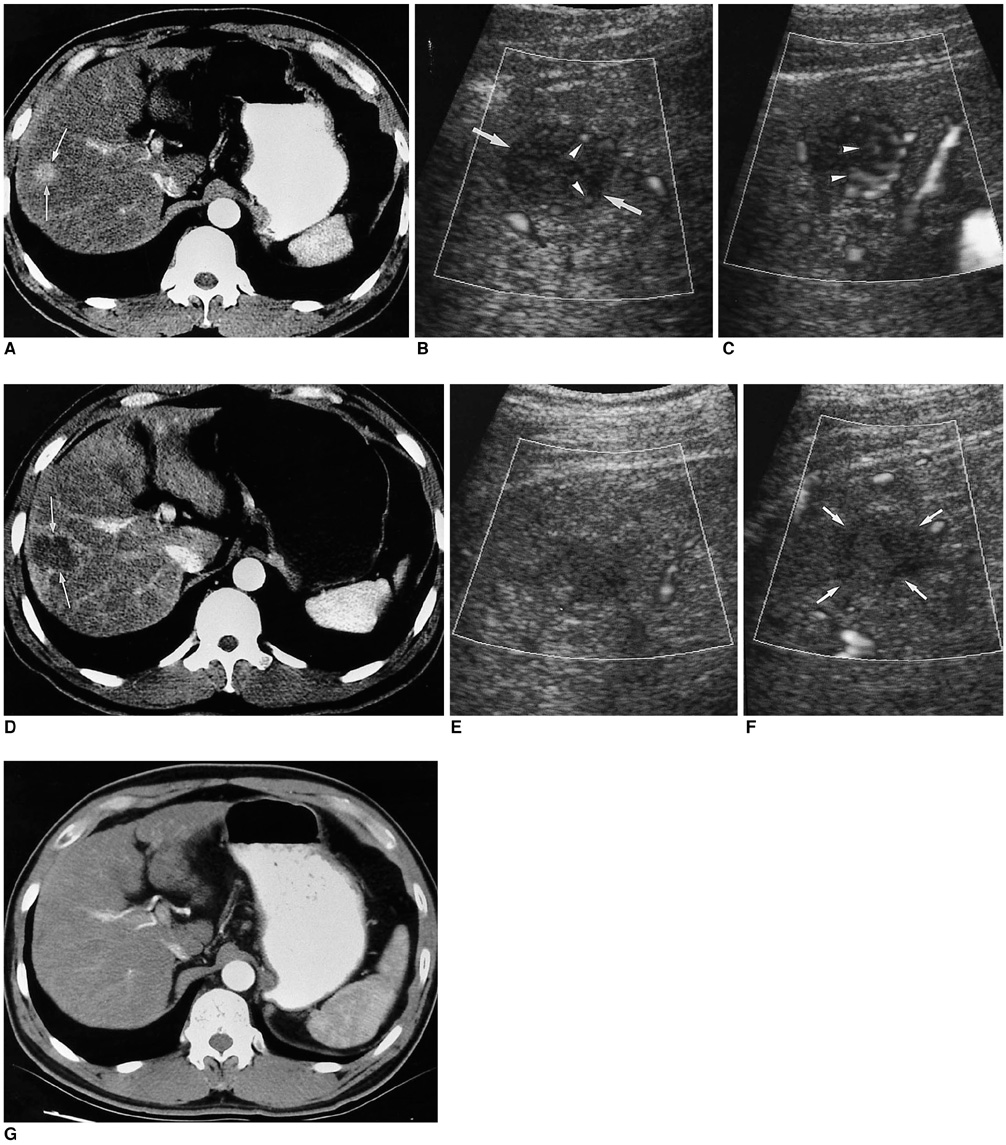
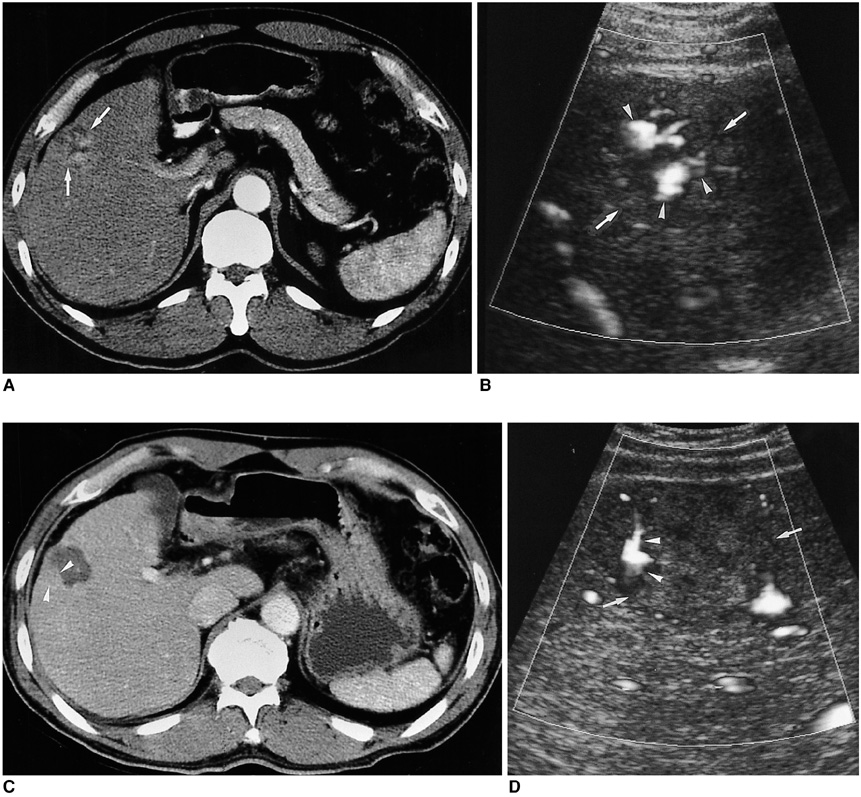
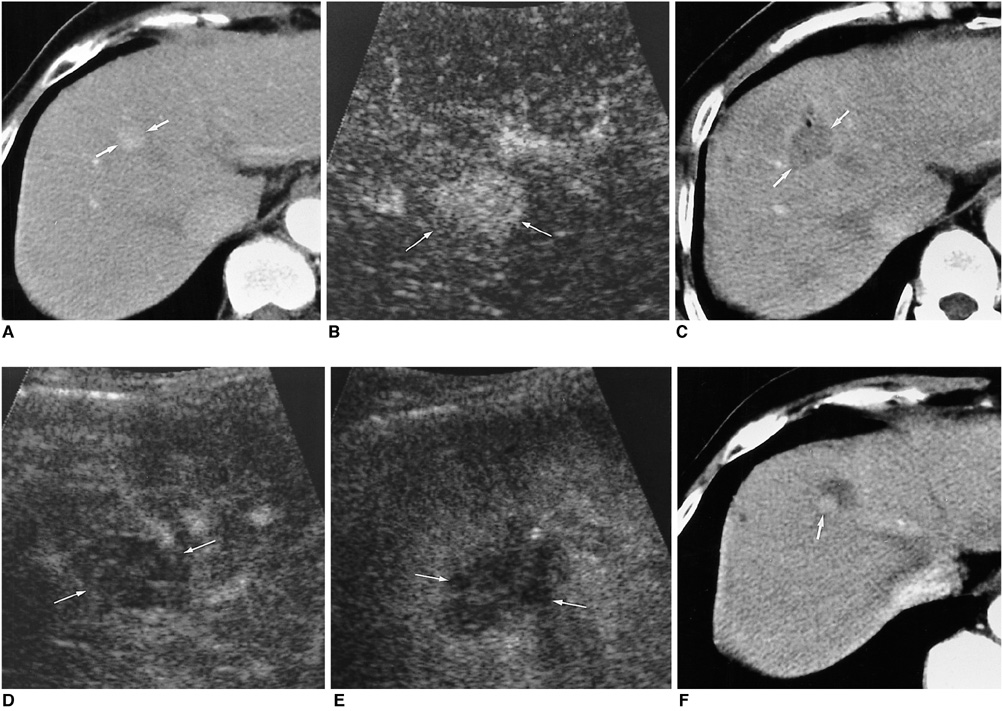
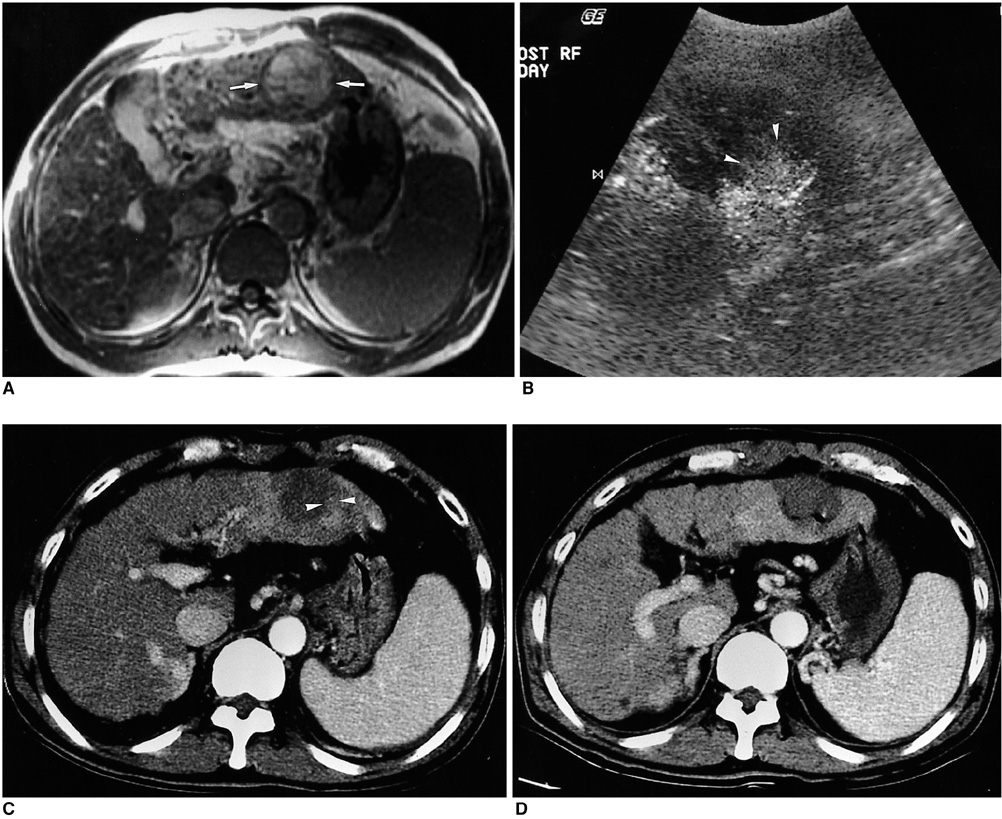
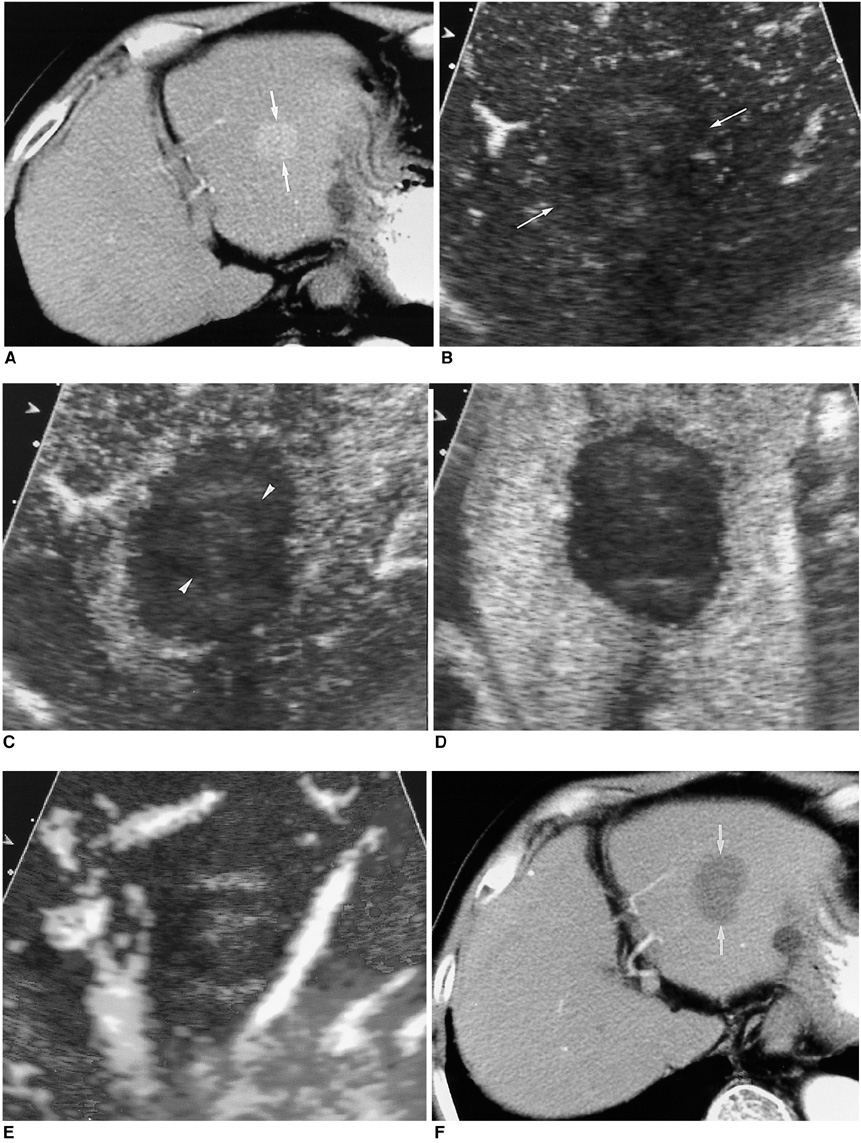
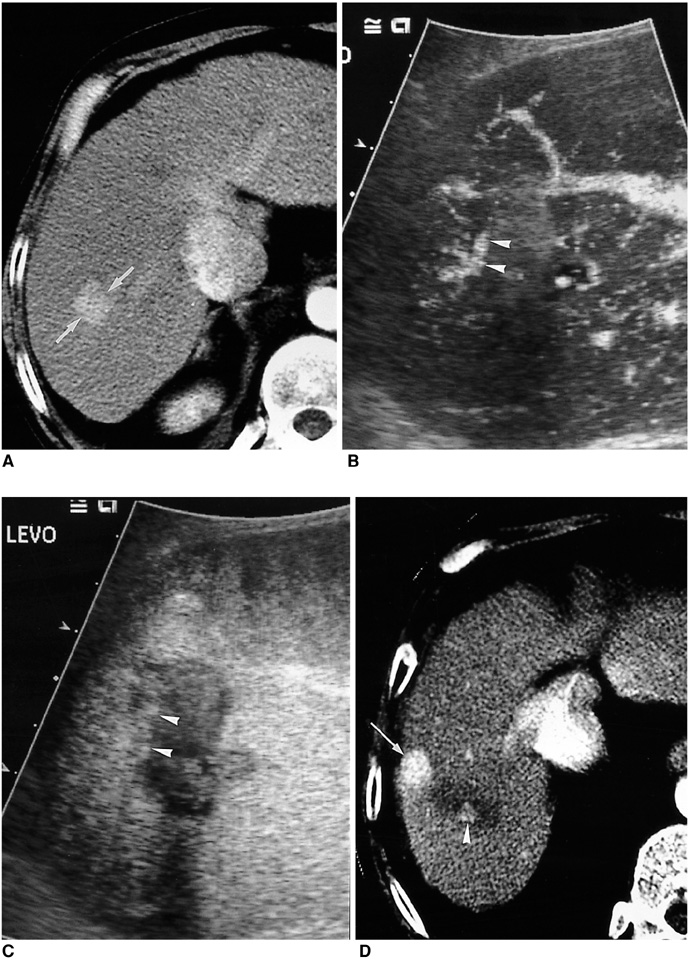
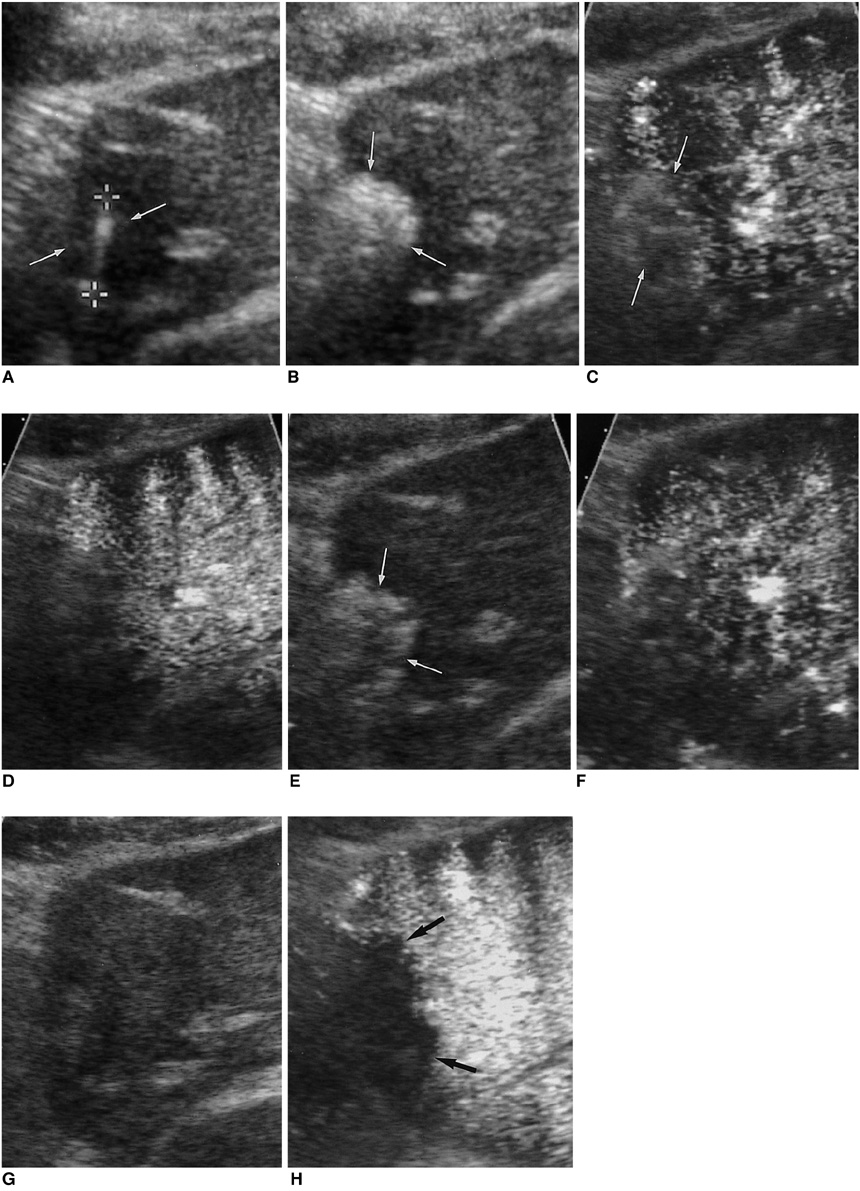
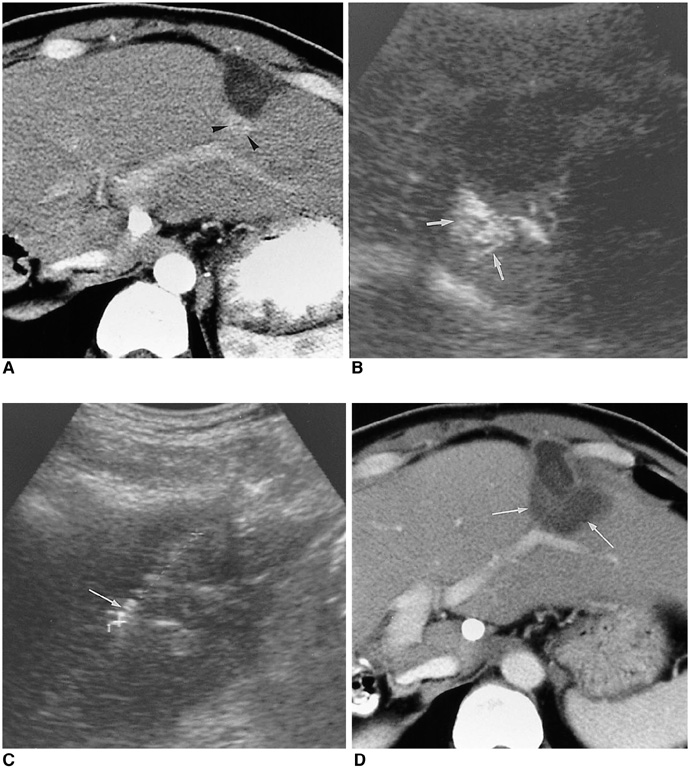
- The early assessment of the therapeutic response after percutaneous radiofrequency (RF) ablation is important, in order to correctly decide whether further treatment is necessary. The residual unablated tumor is usually depicted on contrast-enhanced multiphase helical computed tomography (CT) as a focal enhancing structure during the arterial and portal venous phases. Contrast-enhanced color Doppler and power Doppler ultrasonography (US) have also been used to detect residual tumors. Contrast-enhanced gray-scale US, using a harmonic technology which has recently been introduced, allows for the detection of residual tumors after ablation, without any of the blooming or motion artifacts usually seen on contrast-enhanced color or power Doppler US. Based on our experience and reports in the literature, we consider that contrast-enhanced gray-scale harmonic US constitutes a reliable alternative to contrast-enhanced multiphase CT for the early evaluation of the therapeutic response to RF ablation for liver cancer. This technique was also useful in targeting any residual unablated tumors encountered during additional ablation.
Keyword
MeSH Terms
Figure
Reference
-
1. Dodd GD 3rd, Soulen MC, Kane RA, et al. Minimally invasive treatment of malignant hepatic tumors: at the threshold of a major breakthrough. RadioGraphics. 2000. 20:9–27.2. Livraghi T, Goldberg SN, Lazzarni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999. 210:655–661.3. Gazelle GS, Goldberg SN, Solbiati L, Livraghi T. Tumor ablation with radio-frequency energy. Radiology. 2000. 217:633–646.4. Lim HK. Radiofrequency thermal ablation of hepatocellular carcinomas. Korean J Radiol. 2000. 1:175–184.5. McGahan JP, Dodd GD 3rd. Radiofrequency ablation of the liver: current status. AJR Am J Roentgenol. 2001. 176:3–16.6. Shibata T, Iimuro Y, Yamamoto Y, et al. Small hepatocellular carcinoma: comparison of radio-frequency ablation and percutaneous microwave coagulation therapy. Radiology. 2002. 223:331–337.7. Lim HK, Choi D, Lee WJ, et al. Hepatocellular carcinoma treated with percutaneous radio-frequency ablation: evaluation with follow-up multiphase helical CT. Radiology. 2001. 221:447–454.8. Solbiati L, Goldberg SN, Ierace T, Dellanoce M, Livraghi T, Gazelle GS. Radio-frequency ablation of hepatic metastases: postprocedural assessment with a US microbubble contrast agent-early experience. Radiology. 1999. 211:643–649.9. Choi D, Lim HK, Kim SH, et al. Hepatocellular carcinoma treated with percutaneous radio-frequency ablation: usefulness of power Doppler US with a microbubble contrast agent in evaluating therapeutic response-preliminary results. Radiology. 2000. 217:558–563.10. Meloni MF, Goldberg SN, Livraghi T, et al. Hepatocellular carcinoma treated with radiofrequency ablation: comparison of pulse inversion contrast-enhanced harmonic sonography, contrast-enhanced power Doppler sonography, and helical CT. AJR Am J Roentgenol. 2001. 177:375–380.11. Wen YL, Kudo M, Zheng RQ, et al. Radiofrequency ablation of hepatocellular carcinoma: therapeutic response using contrast-enhanced coded phase-inversion harmonic sonography. AJR Am J Roentgenol. 2003. 181:57–63.12. Choi D, Lim HK, Kim SH, et al. Assessment of therapeutic response in hepatocellular carcinoma treated with percutaneous radiofrequency ablation: comparison of multiphase helical computed tomography and power Doppler ultrasonography with a microbubble contrast agent. J Ultrasound Med. 2002. 21:391–401.13. Youk JH, Lee JM, Kim JS. Therapeutic response evaluation of malignant hepatic masses treated by interventional procedures with contrast-enhanced agent detection imaging. J Ultrasound Med. 2003. 22:911–920.14. Choi D, Lim HK, Lee WJ, et al. Early assessment of the therapeutic response to radio frequency ablation for hepatocellular carcinoma: utility of gray scale harmonic ultrasonography with a microbubble contrast agent. J Ultrasound Med. 2003. 22:1163–1172.15. Goldberg SN, Charboneau JW, Dodd GD 3rd, et al. Image-guided tumor ablation: proposal for standardization of terms and reporting criteria. Radiology. 2003. 228:335–345.16. Jang HJ, Lim HK, Lee WJ, Kim SH, Kim KA, Kim EY. Ultrasonographic evaluation of focal hepatic lesions: comparison of pulse inversion harmonic, tissue harmonic, and conventional imaging techniques. J Ultrasound Med. 2000. 19:293–299.17. Burns PN, Wilson SR, Simpson DH. Pulse inversion imaging of liver blood flow: improved method for characterizing focal masses with microbubble contrast. Invest Radiol. 2000. 35:58–71.18. Lee JY, Choi BI, Han JK, Kim AY, Shin SH, Moon SG. Improved sonographic imaging of hepatic hemangioma with contrast-enhanced coded harmonic angiography: comparison with MR imaging. Ultrasound Med Biol. 2002. 28:287–295.19. Kim JH, Kim TK, Kim BS, et al. Enhancement of hepatic hemangiomas with Levovist on coded harmonic angiographic ultrasonography. J Ultrasound Med. 2002. 21:141–148.20. Jang HJ, Lim HK, Lee WJ, et al. Focal hepatic lesions: evaluation with contrast-enhanced gray-scale harmonic US. Korean J Radiol. 2003. 4:117–123.21. Choi BI, Kim AY, Lee JY, et al. Hepatocellular carcinoma: contrast enhancement with Levovist. J Ultrasound Med. 2002. 21:77–84.22. Goldberg SN, Gazelle GS, Solbiati L, et al. Ablation of liver tumors using percutaneous RF therapy. AJR Am J Roentgenol. 1998. 170:1023–1028.23. Numata K, Isozaki T, Ozawa Y, et al. Percutaneous ablation therapy guided by contrast-enhanced sonography for patients with hepatocellular carcinoma. AJR Am J Roentgenol. 2003. 180:143–149.24. Leen E, Angerson WJ, Yarmenitis S, et al. Multi-center clinical study evaluating the efficacy of SonoVue (BR1), a new ultrasound contrast agent in Doppler investigation of focal hepatic lesions. Eur J Radiol. 2002. 41:200–206.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contrast-enhanced ultrasonography: advance and current status in abdominal imaging
- Contrast-enhanced ultrasound of hepatocellular carcinoma: where do we stand?
- Radiofrequency Ablation for Hepatocellular Carcinoma
- Contrast Enhanced US in the Abdomen
- Fusion imaging of real-time ultrasonography with CT or MRI for hepatic intervention