Focal Eosinophilic Necrosis of the Liver in Patients with Underlying Gastric or Colorectal Cancer: CT Differentiation from Metastasis
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. wjlee@smc.samsung.co.kr
- 2Department of Radiology, Center for Liver Cancer, National Cancer Center, Korea.
- KMID: 1118791
- DOI: http://doi.org/10.3348/kjr.2002.3.4.240
Abstract
OBJECTIVE
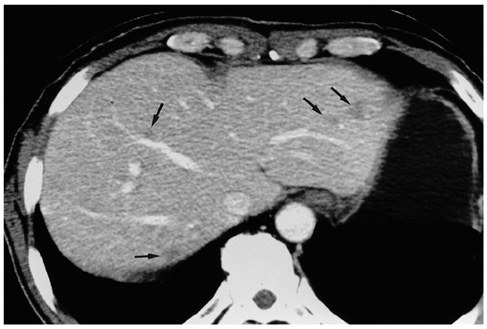
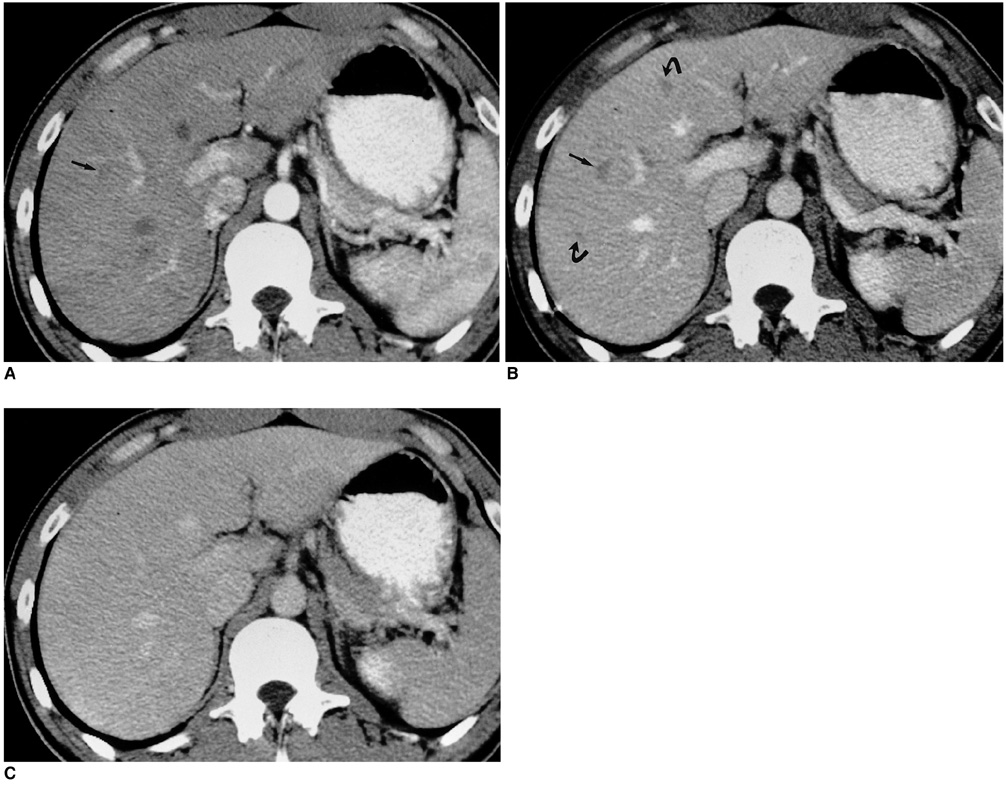
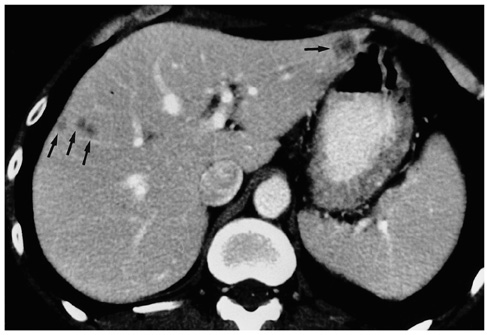
To determine the helical CT findings which help differentiate between focal eosinophilic necrosis (FEN) of the liver and metastasis in patients with underlying gastric or colorectal cancer. MATERIALS AND METHDOS: In 21 patients with underlying gastric and colorectal cancer examined during a recent 18-month period, the presence of FEN (n=90) was proven at CT. The diagnosis was verified by biopsy in eight patients and by the transient nature of the findings related to peripheral eosinophilia (>10%) in the remainder. For comparison, 20 consecutive patients with pathologically proven hepatic metastasis from gastric or colorectal cancer (n=158) were selected. Single-phase helical CT images (7-mm collimation, pitch 1:1) were independently analyzed in a random order by two blinded readers. The parameters evaluated included the margin (depicted border, fuzzy), shape (spherical, non-spherical), attenuation (subtle hypoattenuation, hypoattenuation), and the presence or absence of rim enhancement. RESULTS: FEN far more frequently showed a fuzzy margin (81%, 84%), subtle hypoattenuation (89%, 91%), and a non-spherical shape (84% for both readers) than metastasis, for which the respective findings were 6%, 22%; 20%, 39%; and 15%, 23%. Rim enhancement was seldom found in FEN (0%, 2%), but was recognized by both readers in 40% of metastases. For all parameters, the results were statistically significant (p < .01), and showed that both readers correctly differentiated FEN from metastasis in 78% of the patients (32/41). Interobserver agreement was, in addition, excellent (K= 0.66). CONCLUSION: When focal hepatic lesions with a fuzzy margin, non-spherical shape and subtle hypoattenuation without rim enhancement are found, the possibility of FEN should be considered even in patients with underlying gastrointestinal malignancy.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Enhanced Resolution of Eosinophilic Liver Abscess Associated with Toxocariasis by Albendazole Treatment
Eun Young Jang, Moon Seok Choi, Geum Youn Gwak, Kwang Cheol Koh, Seung Woon Paik, Joon Hyeok Lee, Yong Han Paik, Byung Chul Yoo
Korean J Gastroenterol. 2015;65(4):222-228. doi: 10.4166/kjg.2015.65.4.222.A Case of Eosinophilic Abscess Mistaken for Metastasis due to FDG Uptake in PET-CT
Young Seok Kim, Seong Jin Park, Hee Kyung Kim, Jeoung Mi Park
Korean J Gastroenterol. 2009;54(6):349-354. doi: 10.4166/kjg.2009.54.6.349.A Case of Hepatic Congestion Due to Right Heart Failure Mimicking Liver Tumor
Dong Ho Shin, Myoung Ha Lee, Do Young Kim, Kyong Joo Lee, Jun Yong Park, Sang Hoon Ahn, Kwang-Hyub Han, Chae Yoon Chon
Korean J Gastroenterol. 2010;56(4):264-267. doi: 10.4166/kjg.2010.56.4.264.
Reference
-
1. Lee WJ, Lim HK, Lim JH, Kim SH, Choi SH, Lee SJ. Foci of eosinophil-related necrosis in the liver: imaging findings and correlation with eosinophilia. AJR Am J Roentgenol. 1999. 172:1255–1261.2. Brick SH, Hill MC, Lande IM. The mistaken or indeterminate CT diagnosis of hepatic metastasis: the value of sonography. AJR Am J Roentgenol. 1987. 148:723–726.3. Gaines PA, Sampson MA. The prevalence and characterization of simple hepatic cysts by ultrasound examination. Br J Radiol. 1989. 62:335–337.4. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. 33:159–174.5. Cha SH, Park CM, Cha IH, et al. Hepatic involvement in hypereosinophilic syndrome: value of portal venous phase imaging. Abdom Imaging. 1998. 23:154–157.6. Lim JH, Lee WJ, Lee DH, Nam KJ. Hypereosinophilic syndrome: CT findings in patients with hepatic lobar or segmental involvement. Korean J Radiol. 2000. 1:98–103.7. Fauci AS, Harley JB, Robert WC, Ferrans VJ, Gralnick HR, Bjornson BH. The idiopathic hypereosinophilic syndrome: clinical, pathophysiologic, and therapeutic considerations. Ann Intern Med. 1982. 97:78–92.8. Kim GB, Kwon JH, Kang DS. Hypereosinophilic syndrome: imaging findings in patients with hepatic involvement. AJR Am J Roentgenol. 1993. 161:577–580.9. Nam KJ, Jung WJ, Choi J-C, et al. Hepatic involvement in hypereosinophilia: sonographic findings. J Ultrasound Med. 1999. 18:475–479.10. Oliver JH III, Baron RL. Helical biphasic contrast-enhanced CT of the liver: technique, indications, interpretation, and pitfalls. Radiology. 1996. 201:1–14.11. Cotran RS, Kumar V, Robbins SL. Robbins pathologic basis of disease. 1989. 4th ed. Philadelphia: Saunders;962.12. Schwartz LH, Gandras EJ, Colangelo SM, Ercolani MC, Panicek DM. Prevalence and importance of small hepatic lesions found at CT in patients with cancer. Radiology. 1999. 210:71–74.13. Wasserman SI, Goetzl EJ, Ellman L, Austen KF. Tumor-associated eosinophilotactic factor. N Engl J Med. 1974. 21:420–424.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- F-18 FDG Uptake in an Eosinophilic Liver Abscess Mimicking Hepatic Metastasis on PET/CT Images
- Characteristics of Synchronous Cancers in Gastric Cancer Patients
- Focal Fat Deposition Developed in the Segment IV of the Liver Following Gastrectomy Mimicking a Hepatic Metastasis: Two Case Reports
- Focal Hepatic Eosinophilic Infiltration in Contrast-Enhanced Ultrasonography with Sonazoid: A Case Report
- Early Gastric Mucosal Cancer Associated with Synchronous Liver Metastasis