Yonsei Med J.
2007 Feb;48(1):11-23. 10.3349/ymj.2007.48.1.11.
The HLA System: Genetics, Immunology, Clinical Testing, and Clinical Implications
- Affiliations
-
- 1Department of Pathology, Mount Sinai School of Medicine, New York, NY, USA. yoon.choo@mountsinai.org
- KMID: 1093518
- DOI: http://doi.org/10.3349/ymj.2007.48.1.11
Abstract
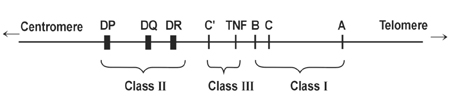
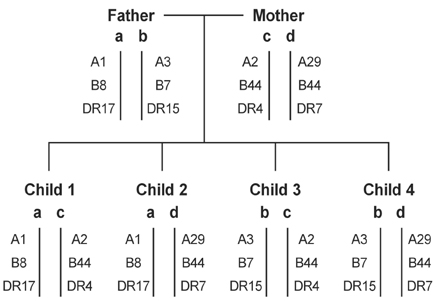
- The human major histocompatibility complex HLA is located on the short arm of chromosome 6. It is known to be the most polymorphic genetic system in humans. The biological role of the HLA class I and class II molecules is to present processed peptide antigens. The HLA system is clinically important as transplantation antigens. Molecular HLA allele typing is routinely performed to provide HLA class I and class II allele matching in unrelated donor hematopoietic stem cell transplantation. Prospective lymphocyte crossmatching is critical in solid organ transplantation to prevent allograft rejection. HLA alloimmunization causes various problems in transfusion therapy. The HLA system is associated with certain diseases, but its underlying mechanisms are not yet fully explained.
Figure
Cited by 1 articles
-
Extracting Structured Genotype Information from Free-Text HLA Reports Using a Rule-Based Approach
Kye Hwa Lee, Hyo Jung Kim, Yi-Jun Kim, Ju Han Kim, Eun Young Song
J Korean Med Sci. 2020;35(12):. doi: 10.3346/jkms.2020.35.e78.
Reference
-
1. Terasaki PI, editor. History of HLA: Ten recollections. 1990. Los Angeles: UCLA Tissue Typing Laboratory Press.2. Bjorkman PJ, Saper MA, Samraoui B, Bennett WS, Strominger JL, Wiley DC. The foreign antigen binding site and T cell recognition regions of class I histocompatibility antigens. Nature. 1987. 329:512–518.3. Beck S, Trowsdale J. The human major histocompatibility complex: lessons from the DNA sequence. Annu Rev Genomics Hum Genet. 2000. 1:117–137. http://www-immuno.path.cam.ac.uk/~immuno/mhc/mhc.html.4. Marsh SGE, Albert ED, Bodmer WF, Bontrop RE, Dupont B, Erlich HA, et al. Nomenclature for factors of the HLA system, 2004. Tissue Antigens. 2005. 65:301–369.5. Bjorkman PJ, Parham P. Structure, function and diversity of class I major histocompatibility complex molecules. Annu Rev Biochem. 1990. 59:253–288.6. Bjorman PJ, Saper MA, Samraoui B, Bennett WS, Strominger JL, Wiley DC. Structure of the human class I histocompatibility antigen, HLA-A2. Nature. 1987. 329:506–512.7. Madden DR, Gorga JC, Strominger JL, Wiley DC. The structure of HLA-B27 reveals nonamer self-peptides bound in an extended conformation. Nature. 1991. 353:321–325.8. Klein J, Sato A. The HLA system. First of two parts. N Engl J Med. 2000. 343:702–709.9. Brown JH, Jardetzky TS, Gorga JC, Stern LJ, Urban RG, Strominger JL, et al. Three-dimensional structure of the human class II histocompatibility antigen HLA-DR1. Nature. 1993. 364:33–39.10. Engelhard VH. Structure of peptides associated with class I and class II MHC molecules. Annu Rev Immunol. 1994. 12:181–207.11. Falk K, Rotzschke O, Stevanovic S, Jung G, Rammensee HG. Allele-specific motifs revealed by sequencing of self-peptides eluted from MHC molecules. Nature. 1991. 351:290–296.12. Zinkernagel RM, Doherty PC. Restriction of in vitro T cell-mediated cytotoxicity in lymphocytic choriomeningitis within a syngeneic or semiallogeneic system. Nature. 1974. 248:701–702.13. Garrett TP, Saper MA, Bjorkman PJ, Strominger JL, Wiley DC. Specificity pockets for the side chains of peptide antigens in HLA-Aw68. Nature. 1989. 342:692–696.14. Stern LJ, Wiley DC. Antigenic peptide binding by class I and class II histocompatibility proteins. Structure. 1994. 2:245–251.15. Pamer E, Cresswell P. Mechanisms of MHC class I-restricted antigen processing. Annu Rev Immunol. 1998. 16:323–358.16. Cresswell P. Assembly, transport, and function of MHC class II molecules. Annu Rev Immunol. 1994. 12:259–293.17. van der Merwe PA, Davis SJ. Molecular interactions mediating T cell antigen recognition. Annu Rev Immunol. 2003. 21:659–684.18. Parham P. Immunogenetics of killer-cell immunoglobulin-like receptors. Tissue Antigens. 2003. 62:194–200.19. Terasaki PI, McClelland JD. Microdroplet assay of human serum cytotoxins. Nature. 1964. 204:998–1000.20. Choo SY, Fan LA, Hansen JA. Allelic variations clustered in the antigen binding sites of HLA-Bw62 molecules. Immunogenetics. 1993. 37:108–113.21. White TJ, Arnheim N, Erlich HA. The polymerase chain reaction. Trends Genet. 1989. 5:185–189.22. The IMGT/HLA Sequence Database. http://www.ebi.ac.uk/imgt/hla/ .23. Petersdorf EW, Hansen JA. A comprehensive approach for typing the alleles of the HLA-B locus by automated sequencing. Tissue Antigens. 1995. 46:73–85.24. Johnson AH, Rossen RD, Butler WT. Detection of allo-antibodies using a sensitive antiglobulin micro-cytotoxicity test: identification of low levels of preformed antibodies in accelerated allograft rejection. Tissue Antigens. 1972. 2:215–226.25. McKenna RM, Takemoto SK, Terasaki PI. Anti-HLA antibodies after solid organ transplantation. Transplantation. 2000. 69:319–326.26. Gebel HM, Bray RA, Nickerson P. Pre-transplant assessment of donor-reactive, HLA-specific antibodies in renal transplantation: contraindication vs. risk. Am J Transplant. 2003. 3:1488–1500.27. Flomenberg N, Baxter-Lowe LA, Confer D, Fernandez-Vina M, Filipovich A, Horowitz M, et al. Impact of HLA class I and class II high-resolution matching on outcomes of unrelated donor bone marrow transplantation: HLA-C mismatching is associated with a strong adverse effect on transplantation outcome. Blood. 2004. 104:1923–1930.28. Petersdorf EW, Malkki M. Human leukocyte antigen matching in unrelated donor hematopoietic cell transplantation. Semin Hematol. 2005. 42:76–84.29. Buckley RH. 27. Transplantation immunology: organ and bone marrow. J Allergy Clin Immunol. 2003. 111:2 Suppl. S733–S744.30. Whitelegg A, Barber LD. The structural basis of T-cell allorecognition. Tissue Antigens. 2004. 63:101–108.31. Hauptman PJ, O'Connor KJ. Procurement and allocation of solid organs for transplantation. N Engl J Med. 1997. 336:422–431.32. http://www.unos.org.34. Jordan SC, Tyan D, Stablein D, McIntosh M, Rose S, Vo A, et al. Evaluation of intravenous immunoglobulin as an agent to lower allosensitization and improve transplantation in highly sensitized adult patients with end-stage renal disease: report of the NIH IG02 trial. J Am Soc Nephrol. 2004. 15:3256–3262.35. Montgomery RA, Zachary AA, Racusen LC, Leffell MS, King KE, Burdick J, et al. Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. Transplantation. 2000. 70:887–895.36. Terasaki PI, Cho Y, Takemoto S, Cecka M, Gjertson D. Twenty-year follow-up on the effect of HLA matching on kidney transplant survival and prediction of future twenty-year survival. Transplant Proc. 1996. 28:1144–1145.37. Terasaki PI, Cecka JM, Gjertson DW, Takemoto S. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med. 1995. 333:333–336.38. Thomas ED. Bone marrow transplantation: a review. Semin Hematol. 1999. 36:4 Suppl 7. 95–103.39. Schoemans H, Theunissen K, Maertens J, Boogaerts M, Verfaillie C, Wagner J. Adult umbilical cord blood transplantation: a comprehensive review. Bone Marrow Transplant. 2006. 38:83–93.40. Martin PJ. The role of donor lymphoid cells in allogeneic marrow engraftment. Bone Marrow Transplant. 1990. 6:283–289.41. Cornelissen JJ, Lowenberg B. Developments in T-cell depletion of allogeneic stem cell grafts. Curr Opin Hematol. 2000. 7:348–352.42. Storb R, Thomas ED, Buckner CD, Clift RA, Johnson FL, Fefer A, et al. Allogeneic marrow grafting for treatment of aplastic anemia. Blood. 1974. 43:157–180.43. Beatty PG, Clift RA, Mickelson EM, Nisperos BB, Flournoy N, Martin PJ, et al. Marrow transplantation from related donors other than HLA-identical siblings. N Engl J Med. 1984. 313:765–771.44. Beatty PG, Hansen JA, Longton GM, Thomas ED, Sanders JE, Martin PJ, et al. Marrow transplantation from HLA-matched unrelated donors for treatment of hematologic malignancies. Transplantation. 1991. 51:443–447.45. McCullough J, Perkins HA, Hansen J. The National Marrow Donor Program with emphasis on the early years. Transfusion. 2006. 46:1248–1255.46. Karanes C, Confer D, Walker T, Askren A, Keller C. Unrelated donor stem cell transplantation: the role of the National Marrow Donor Program. Oncology (Williston Park). 2003. 17:1036–1038. 1043–1044. 1164–1167. http://www.marrow.org/MEDIA/facts_figures.pdf.47. Hurley CK, Fernandez Vina M, Setterholm M. Maximizing optimal hematopoietic stem cell donor selection from registries of unrelated adult volunteers. Tissue Antigens. 2003. 61:415–424.48. Petersdorf EW, Mickelson EM, Anasetti C, Martin PJ, Woolfrey AE, Hansen JA. Effect of HLA mismatches on the outcome of hematopoietic transplants. Curr Opin Immunol. 1999. 11:521–526.49. Morishima Y, Sasazuki T, Inoko H, Juji T, Akaza T, Yamamoto K, et al. The clinical significance of human leukocyte antigen (HLA) allele compatibility in patients receiving a marrow transplant from serologically HLA-A, HLA-B, and HLA-DR matched unrelated donors. Blood. 2002. 99:4200–4206.50. Dickinson AM, Charron D. Non-HLA immunogenetics in hematopoietic stem cell transplantation. Curr Opin Immunol. 2005. 17:517–525.51. Hurley CK, Baxter Lowe LA, Logan B, Karanes C, Anasetti C, Weisdorf D, et al. National Marrow Donor Program HLA-matching guidelines for unrelated marrow transplants. Biol Blood Marrow Transplant. 2003. 9:610–615.52. Jones DC, Young NT. Natural killer receptor repertoires in transplantation. Eur J Immunogenet. 2003. 30:169–176.53. Lowdell MW. Natural killer cells in haematopoietic stem cell transplantation. Transfus Med. 2003. 13:399–404.54. Goulmy E. Human minor histocompatibility antigens. Curr Opin Immunol. 1996. 8:75–81.55. Claas FH, Smeenk RJ, Schmidt R, van Steenbrugge GJ, Eernisse JG. Alloimmunization against the MHC antigens after platelet transfusions is due to contaminating leukocytes in the platelet suspension. Exp Hematol. 1981. 9:84–89.56. Abou-Elella AA, Camarillo TA, Allen MB, Barclay S, Pierce JA, Holland HK, et al. Low incidence of red cell and HLA antibody formation by bone marrow transplant patients. Transfusion. 1995. 35:931–935.57. Storb R, Thomas ED, Buckner DC, Appelbaum FR, Clift RA, Deeg HJ, et al. Marrow transplantation for aplastic anemia. Semin Hematol. 1984. 21:27–35.58. van Marwijk-Kooy M, van Prooijen HC, Moes M, Bosma-Stants I, Akkerman JW. Use of leukocyte-depleted platelet concentrates for the prevention of refractoriness and primary HLA alloimmunization: a prospective, randomized trial. Blood. 1991. 77:201–205.59. Sintnicolaas K, van Marwijk Kooij M, van Prooijen HC, van Dijk BA, van Putten WL, Claas FH, et al. Leukocyte depletion of random single-donor platelet transfusions does not prevent secondary human leukocyte antigen-alloimmunization and refractoriness: a randomized prospective study. Blood. 1995. 85:824–828.60. McFarland JG, Anderson AJ, Slichter SJ. Factors influencing the transfusion response to HLA-selected apheresis donor platelets in patients refractory to random platelet concentrates. Br J Haematol. 1989. 73:380–386.61. Doughty HA, Murphy MF, Metcalfe P, Rohatiner AZ, Lister TA, Waters AH. Relative importance of immune and non-immune causes of platelet refractoriness. Vox Sang. 1994. 66:200–205.62. International Forum. Detection of platelet-reactive antibodies in patients who are refractory to platelet transfusions, and the selection of compatible donors. Vox Sang. 2003. 84:73–88.63. Rachel JM, Summers TC, Sinor LT, Plapp FV. Use of a solid phase red blood cell adherence method for pretransfusion platelet compatibility testing. Am J Clin Pathol. 1988. 90:63–68.64. Seftel MD, Growe GH, Petraszko T, Benny WB, Le A, Lee CY, et al. Universal prestorage leukoreduction in Canada decreases platelet alloimmunization and refractoriness. Blood. 2004. 103:333–339.65. Petz LD, Calhoun L, Yam P, Cecka M, Schiller G, Faitlowicz AR, et al. Transfusion-associated graft-versus-host disease in immunocompetent patients: report of a fatal case associated with transfusion of blood from a second-degree relative, and a survey of predisposing factors. Transfusion. 1993. 33:742–750.66. Shivdasani RA, Anderson KC. HLA homozygosity and shared HLA haplotypes in the development of transfusion-associated graft-versus-host disease. Leuk Lymphoma. 1994. 15:227–234.67. Davey RJ. Transfusion-associated graft-versus-host disease and the irradiation of blood components. Immunol Invest. 1995. 24:431–434.68. Popovsky MA, Moore SB. Diagnostic and pathogenetic considerations in transfusion-related acute lung injury. Transfusion. 1985. 25:573–577.69. Kopko PM, Paglieroni TG, Popovsky MA, Muto KN, MacKenzie MR, Holland PV. TRALI: correlation of antigen-antibody and monocyte activation in donor-recipient pairs. Transfusion. 2003. 43:177–184.70. Silliman CC, Paterson AJ, Dickey WO, Stroneck DF, Popovsky MA, Caldwell SA, et al. The association of biologically active lipids with the development of transfusion-related acute lung injury: a retrospective study. Transfusion. 1997. 37:719–726.71. Deaver JE, Leppert PC, Zaroulis CG. Neonatal alloimmune thrombocytopenic purpura. Am J Perinatol. 1986. 3:127–131.72. Valentin N, Vergracht A, Bignon JD, Cheneau ML, Blanchard D, Kaplan C, et al. HLA-DRw52a is involved in alloimmunization against PL-A1 antigen. Hum Immunol. 1990. 27:73–79.73. Saito S, Ota M, Komatsu Y, Ota S, Aoki S, Koike K, et al. Serologic analysis of three cases of neonatal alloimmune thrombocytopenia associated with HLA antibodies. Transfusion. 2003. 43:908–917.74. Thorsby E. Invited anniversary review: HLA associated diseases. Hum Immunol. 1997. 53:1–11.75. Feder JN, Gnirke A, Thomas W, Tsuchihashi Z, Ruddy DA, Basava A, et al. A novel MHC class I-like gene is mutated in patients with hereditary haemochromatosis. Nat Genet. 1996. 13:399–408.76. Pena SD, Chakraborty R. Paternity testing in the DNA era. Trends Genet. 1994. 10:204–209.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Genetic Testing and Genetic Counseling
- Is There Any Relationship Between Human Leucocyte Antigen Class II and Chronic Urticaria? (Chronic Urticaria and HLA Class II)
- New HLA Nomenclature (2010) and Its Clinical Application in Koreans
- Tourette disorder and HLA typing
- Alterations of HLA class I and class II antigen expressions in borderline, invasive and metastatic ovarian cancers