Yonsei Med J.
2008 Apr;49(2):255-264. 10.3349/ymj.2008.49.2.255.
Agreements between Indirect Calorimetry and Prediction Equations of Resting Energy Expenditure in End-Stage Renal Disease Patients on Continuous Ambulatory Peritoneal Dialysis
- Affiliations
-
- 1Division of Nephrology and Hypertension, Department of Internal Medicine, Kidney Disease Research Group, Inha University College of Medicine, Incheon, Korea. nhkimj@inha.ac.kr
- 2Department of Food and Nutrition, Catholic University, Buchon, Korea.
- KMID: 1084499
- DOI: http://doi.org/10.3349/ymj.2008.49.2.255
Abstract
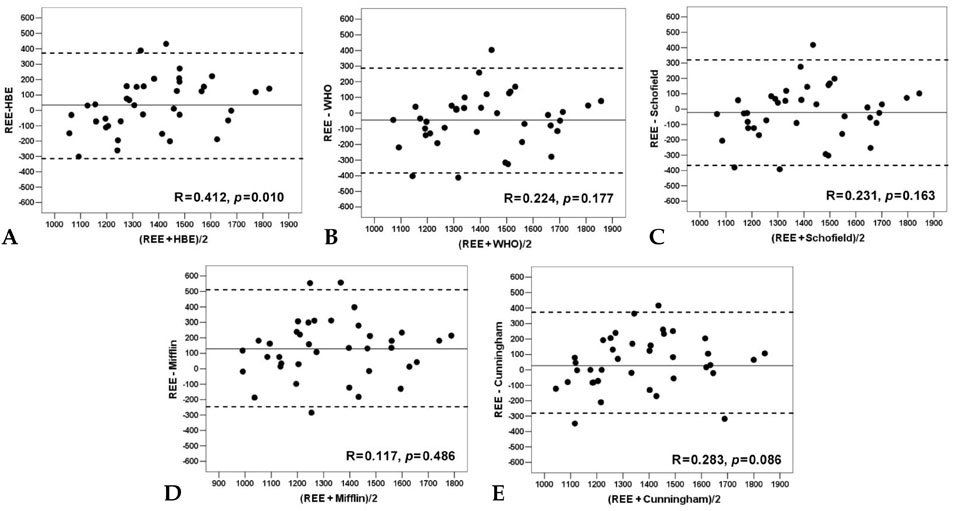
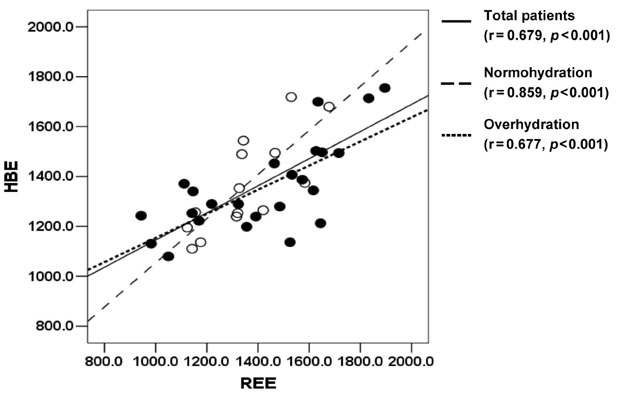
- PURPOSE
Equations are frequently used to estimate resting energy expenditure (REE) in a clinical setting. However, few studies have examined their accuracy in end-stage renal disease (ESRD) patients. PATIENTS AND METHODS: To investigate agreement between indirect calorimetry and several REE estimating equations in 38 ESRD patients on peritoneal dialysis, we performed indirect calorimetry and compared the results with REEs estimated using 5 equations [Harris-Benedict (HBE), Mifflin, WHO, Schofield, and Cunningham]. RESULTS: Measured REE was 1393.2 +/- 238.7kcal/day. There were no significant differences between measured and estimated REEs except Mifflin (1264.9 +/- 224.8kcal/day). Root mean square errors were smallest for HBE, followed by Schofield, Cunningham, and WHO, and largest for Mifflin (171.3, 171.9, 174.6, 175.3, and 224.6, respectively). In Bland-Altman plot, correlation coefficients between mean values and differences were significant for HBE (r=0.412, p=0.012) and tended to be significant for Cunningham (r=0.283, p=0.086). In DM patients and patients with overhydration, HBE showed significant underestimation when REE increased. CONCLUSION: In ESRD patients on continuous ambulatory peritoneal dialysis (CAPD), REE-estimating equations have no significant differences from indirect calorimetry, except Mifflin. However, HBE showed greater bias than others when REE was high.
MeSH Terms
Figure
Reference
-
1. Qureshi AR, Alvestrand A, Danielsson A, Divino-Filho JC, Gutierrez A, Lindholm B, et al. Factors predicting malnutrition in hemodialysis patients: a cross-sectional study. Kidney Int. 1998. 53:773–782.
Article2. Widdowson EM, Edholm OG, McCance RA. The food intake and energy expenditure of cadets in training. Br J Nutr. 1954. 8:147–155.
Article3. Boothby WM, Sandiford I. Summary of the basal metabolism data on 8614 subjects with special reference to the normal standards for the estimation of the basal metabolic rate. J Biol Chem. 1922. 54:783–803.
Article4. Ravussin E, Lillioja S, Knowler WC, Christin L, Freymond D, Abbott WG, et al. Reduced rate of energy expenditure as a risk factor for body weight gain. N Engl J Med. 1988. 318:467–472.
Article5. Elia M. Kinney JM, Tucker HN, editors. Energy expenditure in whole body. Energy metabolism: Tissue determinants and cellular corollaries. 1992. New York: Raven Press;19–59.6. Quenouille MH, Boyne AW, Fisher WB, Leitch I. Commonwealth Bureau of Animal Nutrition Communication No. 17. Statistical studies of recorded energy expenditure of man. Part 1. Basal metabolism related to sex, stature, age, climate and race. 1951. Bucksburn, United Kingdom: Commonwealth Agricultural Bureau, Rowett Institute.7. Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985. 39:Suppl 1. 5–41.8. Siervo M, Boschi V, Falconi C. Which REE prediction equation should we use in normal-weight, overweight and obese women? Clin Nutr. 2003. 22:193–204.
Article9. Bott L, Béghin L, Marichez C, Gottrand F. Comparison of resting energy expenditure in bronchopulmonary dysplasia to predicted equation. Eur J Clin Nutr. 2006. 60:1323–1329.
Article10. Suman OE, Mlcak RP, Chinkes DL, Herndon DN. Resting energy expenditure in severely burned children: analysis of agreement between indirect calorimetry and prediction equations using the Bland-Altman method. Burns. 2006. 32:335–342.
Article11. Cuerda Compés MC, Ruiz Sancho A, Moreno Rengel C, Iriondo Martínez MT, Velasco Gimeno C, Bretón Lesmes I, et al. Study of energy expenditure in anorexia nervosa: agreement between indirect calorimatry and several equations (in Spanish). Nutr Hosp. 2005. 20:371–377.12. Rigalleau V, Lasseur C, Pecheur S, Chauveau P, Combe C, Perlemoine C, et al. Resting energy expenditure in uremic, diabetic, and uremic diabetic subjects. J Diabetes Complications. 2004. 18:237–241.
Article13. Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949. 109:1–9.
Article14. Zurlo F, Larson K, Bogardus C, Ravussin E. Skeletal muscle metabolism is a major determinant of resting energy expenditure. J Clin Invest. 1990. 86:1423–1427.
Article15. Harris JA, Benedict FG. A biometric study of basal metabolism in man. 1919. Washington, DC, USA: Carnegie Institute of Washington;[Carnegie Institute of Washington Publication 279].16. Mifflin MD St, Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990. 51:241–247.
Article17. FAO/WHO/UNU. Energy and protein requirements. Report of a joint FAO/WHO/UNU Expert Consultation. 1985. 724:World Health Organ Tech Rep Ser;1–206.18. Cunningham JJ. A reanalysis of the factors influencing basal metabolic rate in normal adults. Am J Clin Nutr. 1980. 33:2372–2374.
Article19. Bedogni G, Malavolti M, Severi S, Poli M, Mussi C, Fantuzzi AL, et al. Accuracy of an eight-point tactileelectrode impedance method in the assessment of total body water. Eur J Clin Nutr. 2002. 56:1143–1148.
Article20. Malavolti M, Mussi C, Poli M, Fantuzzi AL, Salvioli G, Battistini N, et al. Cross-calibration of eight-polar bioelectrical impedance analysis versus dual-energy X-ray absorptiometry for the assessment of total and appendicular body composition in healthy subjects aged 21 - 82 years. Ann Hum Biol. 2003. 30:380–391.
Article21. Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, et al. What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987. 11:8–13.
Article22. Nolph KD, Moore HL, Twardowski ZJ, Khanna R, Prowant B, Meyer M, et al. Cross-sectional assessment of weekly urea and creatinine clearances in patients on continuous ambulatory peritoneal dialysis. ASAIO J. 1992. 38:M139–M142.
Article23. Watson PE, Watson ID, Batt RD. Total body water volumes for adult males and females estimated from simple anthropometric measurements. Am J Clin Nutr. 1980. 33:27–39.
Article24. Bergström J, Heimbürger O, Lindholm B. Calculation of the protein equivalent of total nitrogen appearance from urea appearance. Which formulas should be used? Perit Dial Int. 1998. 18:467–473.
Article25. van Olden RW, Krediet RT, Struijk DG, Arisz L. Measurement of residual renal function in patients treated with continuous ambulatory peritoneal dialysis. J Am Soc Nephrol. 1996. 7:745–750.
Article26. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986. 1:307–310.
Article27. Sardesai VM. Sardesai VM, editor. Requirements for energy, carbohydrates, fat, and proteins. Introduction to clinical nutrition. 1998. New York: Dekker M;1–13.28. Pupim LB, Ikizler TA. Assessment and monitoring of uremic malnutrition. J Ren Nutr. 2004. 14:6–19.
Article29. Simonson DC, DeFronzo RA. Indirect calorimetry: methodological and interpretative problems. Am J Physiol. 1990. 258:E399–E412.
Article30. Ferrannini E. The theoretical bases of indirect calorimetry: a review. Metabolism. 1988. 37:287–301.
Article31. Schutz Y, Deurenberg P. Energy metabolism: overview of recent methods used in human studies. Ann Nutr Metab. 1996. 40:183–193.
Article32. Matarese LE. Indirect calorimetry: technical aspects. J Am Diet Assoc. 1997. 97(10 Suppl 2):S154–S160.33. Avesani CM, Cuppari L, Silva AC, Sigulem DM, Cendoroglo M, Sesso R, et al. Resting energy expenditure in pre-dialysis diabetic patients. Nephrol Dial Transplant. 2001. 16:556–565.
Article34. Price SR, Bailey JL, Wang X, Jurkovitz C, England BK, Ding X, et al. Muscle wasting in insulinopenic rats results from activation of the ATP-dependent, ubiquitinproteasome proteolytic pathway by a mechanism including gene transcription. J Clin Invest. 1996. 98:1703–1708.
Article35. Ikizler TA, Wingard RL, Sun M, Harvell J, Parker RA, Hakim RM. Increased energy expenditure in hemodi alysis patients. J Am Soc Nephrol. 1996. 7:2646–2653.36. Neyra R, Chen KY, Sun M, Shyr Y, Hakim RM, Ikizler TA. Increased resting energy expenditure in patients with end-stage renal disease. JPEN J Parenter Enteral Nutr. 2003. 27:36–42.
Article37. O'Sullivan AJ, Lawson JA, Chan M, Kelly JJ. Body composition and energy metabolism in chronic renal insufficiency. Am J Kidney Dis. 2002. 39:369–375.38. Schneeweiss B, Graninger W, Stockenhuber F, Druml W, Ferenci P, Eichinger S, et al. Energy metabolism in acute and chronic renal failure. Am J Clin Nutr. 1990. 52:596–601.
Article39. Monteon FJ, Laidlaw SA, Shaib JK, Kopple JD. Energy expenditure in patients with chronic renal failure. Kidney Int. 1986. 30:741–747.
Article40. Cha K, Chertow GM, Gonzalez J, Lazarus JM, Wilmore DW. Multifrequency bioelectrical impedance estimates the distribution of body water. J Appl Physiol. 1995. 79:1316–1319.
Article41. Oe B, de Fijter WH, Oe PL, Stevens P, de Vries PM. Diameter of inferior caval vein (VCD) and bioelectrical impedance analysis (BIA) for the analysis of hydration status in patients on hemodialysis. Clin Nephrol. 1998. 50:38–43.42. Oe B, De Fijter WM, De Fijter CW, Straver B, Oe PL, Stevens P, et al. Detection of hydration status by total body bioelectrical impedance analysis (BIA) in patients on hemodialysis. Int J Artif Organs. 1997. 20:371–374.
Article43. Jaeger JQ, Mehta RL. Dry weight and body composition in hemodialysis: A proposal for an index of fluid removal. Semin Dial. 1999. 12:164–174.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Energy Expenditure in Young Adults and Newborns by Indirect Calorimetry
- Comparision of measured resting energy expenditure by indirect calorimetry and predicted value in the obese
- Accuracy of predictive equations for resting energy expenditure (REE) in non-obese and obese Korean children and adolescents
- A clinical study of continuous ambulatory peritoneal dialysis in childhood
- Accuracy of Predictive Equations for Resting Metabolic Rates and Daily Energy Expenditures of Police Officials Doing Shift Work by Type of Work