Orthostatic Hypotension: Mechanisms, Causes, Management
- Affiliations
-
- 1Department of Neurology, Mayo Clinic, Rochester, MN, USA. low@mayo.edu
- KMID: 1894552
- DOI: http://doi.org/10.3988/jcn.2015.11.3.220
Abstract
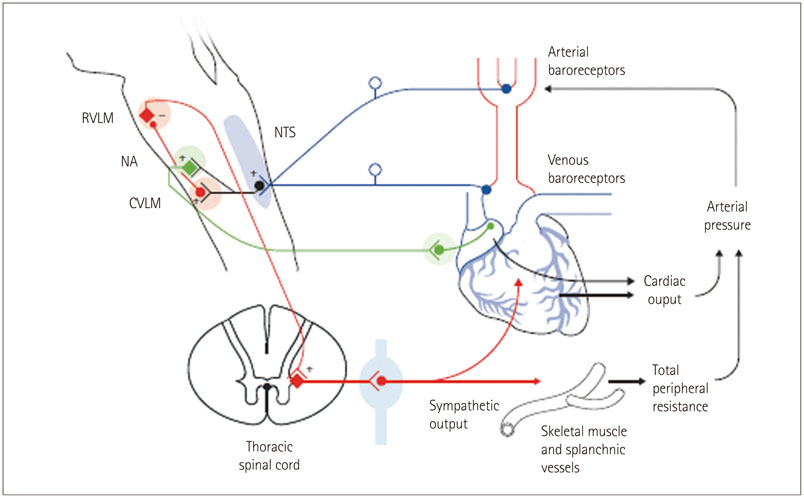
- Orthostatic hypotension (OH) occurs when mechanisms for the regulation of orthostatic BP control fails. Such regulation depends on the baroreflexes, normal blood volume, and defenses against excessive venous pooling. OH is common in the elderly and is associated with an increase in mortality rate. There are many causes of OH. Aging coupled with diseases such as diabetes and Parkinson's disease results in a prevalence of 10-30% in the elderly. These conditions cause baroreflex failure with resulting combination of OH, supine hypertension, and loss of diurnal variation of BP. The treatment of OH is imperfect since it is impossible to normalize standing BP without generating excessive supine hypertension. The practical goal is to improve standing BP so as to minimize symptoms and to improve standing time in order to be able to undertake orthostatic activities of daily living, without excessive supine hypertension. It is possible to achieve these goals with a combination of fludrocortisone, a pressor agent (midodrine or droxidopa), supplemented with procedures to improve orthostatic defenses during periods of increased orthostatic stress. Such procedures include water bolus treatment and physical countermaneuvers. We provide a pragmatic guide on patient education and the patient-orientated approach to the moment to moment management of OH.
MeSH Terms
Figure
Cited by 7 articles
-
Recent advances in pediatric headaches
Eun Sook Suh
J Korean Med Assoc. 2017;60(2):109-111. doi: 10.5124/jkma.2017.60.2.109.Normal aging: definition and physiologic changes
Chul Ho Chang, Ki-Young Lee, Yon Hee Shim
J Korean Med Assoc. 2017;60(5):358-363. doi: 10.5124/jkma.2017.60.5.358.Cardiovascular Autonomic Dysfunction in Patients with Drug-Induced Parkinsonism
Joong-Seok Kim, Dong-Woo Ryu, Ju-Hee Oh, Yang-Hyun Lee, Sung-Jin Park, Kipyung Jeon, Jong-Yun Lee, Seong Hee Ho, Jungmin So, Jin Hee Im, Kwang-Soo Lee
J Clin Neurol. 2017;13(1):15-20. doi: 10.3988/jcn.2017.13.1.15.Orthostatic hypotension with meningoencephalitis involving the rostral ventrolateral medulla
Young Ik Jung, Mun Kyung Sunwoo, Hee Jin Lee, Jeong Hee Seo, Jeongyeon Kim
Ann Clin Neurophysiol. 2019;21(1):66-69. doi: 10.14253/acn.2019.21.1.66.Update on the Impact, Diagnosis and Management of Cardiovascular Autonomic Neuropathy in Diabetes: What Is Defined, What Is New, and What Is Unmet
Vincenza Spallone
Diabetes Metab J. 2019;43(1):3-30. doi: 10.4093/dmj.2018.0259.Patterns of Orthostatic Blood Pressure Changes in Patients with Orthostatic Hypotension
Hung Youl Seok, Yoo Hwan Kim, Hayom Kim, Byung-Jo Kim
J Clin Neurol. 2018;14(3):283-290. doi: 10.3988/jcn.2018.14.3.283.Diagnosis and Management of Diabetic Autonomic Neuropathy
Chong Hwa Kim
J Korean Diabetes. 2018;19(3):160-167. doi: 10.4093/jkd.2018.19.3.160.
Reference
-
1. Low PA. Update on the evaluation, pathogenesis, and management of neurogenic orthostatic hypotension: introduction. Neurology. 1995; 45:4 Suppl 5. S4–S5.2. Thieben MJ, Sandroni P, Sletten DM, Benrud-Larson LM, Fealey RD, Vernino S, et al. Postural orthostatic tachycardia syndrome: the Mayo clinic experience. Mayo Clin Proc. 2007; 82:308–313.
Article3. The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. Neurology. 1996; 46:1470.4. Low PA. Prevalence of orthostatic hypotension. Clin Auton Res. 2008; 18:Suppl 1. 8–13.
Article5. Low PA, Singer W. Management of neurogenic orthostatic hypotension: an update. Lancet Neurol. 2008; 7:451–458.
Article6. Low PA, Walsh JC, Huang CY, McLeod JG. The sympathetic nervous system in diabetic neuropathy. A clinical and pathological study. Brain. 1975; 98:341–356.
Article7. Fujimura J, Camilleri M, Low PA, Novak V, Novak P, Opfer-Gehrking TL. Effect of perturbations and a meal on superior mesenteric artery flow in patients with orthostatic hypotension. J Auton Nerv Syst. 1997; 67:15–23.
Article8. Lipp A, Sandroni P, Ahlskog JE, Fealey RD, Kimpinski K, Iodice V, et al. Prospective differentiation of multiple system atrophy from Parkinson disease, with and without autonomic failure. Arch Neurol. 2009; 66:742–750.
Article9. Thaisetthawatkul P, Boeve BF, Benarroch EE, Sandroni P, Ferman TJ, Petersen R, et al. Autonomic dysfunction in dementia with Lewy bodies. Neurology. 2004; 62:1804–1809.
Article10. Low PA, Walsh JC, Huang CY, McLeod JG. The sympathetic nervous system in alcoholic neuropathy. A clinical and pathological study. Brain. 1975; 98:357–364.
Article11. Ketch T, Biaggioni I, Robertson R, Robertson D. Four faces of baroreflex failure: hypertensive crisis, volatile hypertension, orthostatic tachycardia, and malignant vagotonia. Circulation. 2002; 105:2518–2523.12. Low PA, Caskey PE, Tuck RR, Fealey RD, Dyck PJ. Quantitative sudomotor axon reflex test in normal and neuropathic subjects. Ann Neurol. 1983; 14:573–580.
Article13. Low PA. Autonomic nervous system function. J Clin Neurophysiol. 1993; 10:14–27.
Article14. Low PA. Laboratory evaluation of autonomic function. Suppl Clin Neurophysiol. 2004; 57:358–368.15. Denq JC, O'Brien PC, Low PA. Normative data on phases of the Valsalva maneuver. J Clin Neurophysiol. 1998; 15:535–540.
Article16. Fealey RD, Low PA, Thomas JE. Thermoregulatory sweating abnormalities in diabetes mellitus. Mayo Clin Proc. 1989; 64:617–628.
Article17. El-Sayed H, Hainsworth R. Salt supplement increases plasma volume and orthostatic tolerance in patients with unexplained syncope. Heart. 1996; 75:134–140.
Article18. Low PA, Gilden JL, Freeman R, Sheng KN, McElligott MA. Midodrine Study Group. Efficacy of midodrine vs placebo in neurogenic orthostatic hypotension A randomized, double-blind multicenter study. JAMA. 1997; 277:1046–1051.
Article19. Figueroa JJ, Basford JR, Low PA. Preventing and treating orthostatic hypotension: as easy as A, B, C. Cleve Clin J Med. 2010; 77:298–306.
Article20. Smit AA, Wieling W, Fujimura J, Denq JC, Opfer-Gehrking TL, Akarriou M, et al. Use of lower abdominal compression to combat orthostatic hypotension in patients with autonomic dysfunction. Clin Auton Res. 2004; 14:167–175.
Article21. Denq JC, Opfer-Gehrking TL, Giuliani M, Felten J, Convertino VA, Low PA. Efficacy of compression of different capacitance beds in the amelioration of orthostatic hypotension. Clin Auton Res. 1997; 7:321–326.
Article22. Jordan J, Shannon JR, Grogan E, Biaggioni I, Robertson D. A potent pressor response elicited by drinking water. Lancet. 1999; 353:723.
Article23. Jordan J, Shannon JR, Black BK, Ali Y, Farley M, Costa F, et al. The pressor response to water drinking in humans: a sympathetic reflex? Circulation. 2000; 101:504–509.24. Bouvette CM, McPhee BR, Opfer-Gehrking TL, Low PA. Role of physical countermaneuvers in the management of orthostatic hypotension: efficacy and biofeedback augmentation. Mayo Clin Proc. 1996; 71:847–853.
Article25. Maule S, Papotti G, Naso D, Magnino C, Testa E, Veglio F. Orthostatic hypotension: evaluation and treatment. Cardiovasc Hematol Disord Drug Targets. 2007; 7:63–70.
Article26. Kaufmann H, Freeman R, Biaggioni I, Low P, Pedder S, Hewitt LA, et al. Droxidopa for neurogenic orthostatic hypotension: a randomized, placebo-controlled, phase 3 trial. Neurology. 2014; 83:328–335.
Article27. Singer W, Sandroni P, Opfer-Gehrking TL, Suarez GA, Klein CM, Hines S, et al. Pyridostigmine treatment trial in neurogenic orthostatic hypotension. Arch Neurol. 2006; 63:513–518.
Article28. Shibao C, Gamboa A, Diedrich A, Biaggioni I. Management of hypertension in the setting of autonomic failure: a pathophysiological approach. Hypertension. 2005; 45:469–476.
Article29. Rodstein M, Zeman FD. Postural blood pressure changes in the elderly. J Chronic Dis. 1957; 6:581–588.
Article30. Caird FI, Andrews GR, Kennedy RD. Effect of posture on blood pressure in the elderly. Br Heart J. 1973; 35:527–530.
Article31. Myers MG, Kearns PM, Kennedy DS, Fisher RH. Postural hypotension and diuretic therapy in the elderly. Can Med Assoc J. 1978; 119:581–585.32. MacLennan WJ, Hall MR, Timothy JI. Postural hypotension in old age: is it a disorder of the nervous system or of blood vessels? Age Ageing. 1980; 9:25–32.
Article33. Lennox IM, Williams BO. Postural hypotension in the elderly. Clin Exp Gerontol. 1980; 2:313–329.34. Palmer KT. Studies into postural hypotension in elderly patients. N Z Med J. 1983; 96:43–45.35. Mader SL, Josephson KR, Rubenstein LZ. Low prevalence of postural hypotension among community-dwelling elderly. JAMA. 1987; 258:1511–1514.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orthostatic Intolerance Syndrome
- Diagnosis and management of neurogenic orthostatic hypotension
- Isolated Orthostatic Hypotension Secondary to Pontine Hemorrhage
- Orthostatic Hypotension: Mechanisms, Causes, Management
- Risk Factors of Orthostatic Hypotension among the Long-term Hospitalized Elderly Patients