J Korean Fract Soc.
2010 Jul;23(3):289-295. 10.12671/jkfs.2010.23.3.289.
Staged Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, School of Medicine, Kyungpook National University, Daegu, Korea. cwoh@knu.ac.kr
- 2Department of Orthopedic Surgery, School of Medicine, Korea University, Seoul, Korea.
- 3Department of Orthopedic Surgery, Daegu Veterans Hospital, Daegu, Korea.
- KMID: 1712344
- DOI: http://doi.org/10.12671/jkfs.2010.23.3.289
Abstract
- PURPOSE
To assess the result of staged minimally invasive plate osteosynthesis (MIPO) for distal tibial fracture with an open wound or injured soft tissue.
MATERIALS AND METHODS
In 20 patients (mean age, 47.8 year-old) with distal tibial fractures, there were 4 type A fractures and 16 type C fractures based on the AO classification system. Eight of the 20 patients had open fractures. MIPO was performed on average 23.9 days after bridging external fixation. At the final follow-up, we assessed the radiological results of bone union and alignment. Functional results were also evaluated by measuring the degrees of ankle motion and the American Orthopedic Foot & Ankle Society (AOFAS) scores.
RESULTS
Seventeen of 20 cases (85%) achieved primary union at an average of 21.3 weeks. There were 3 cases of nonunion requiring a bone graft. The mean AOFAS score was 88.5 (range, 67~92) and the average range of ankle motion was 49.2degrees (plantarflexion: 37.4degrees, dorsiflexion: 11.8degrees). Complication included 2 cases of minor mal-alignment, 1 case of claw toe and 1 case of peroneal neuropathy. Patients over the age of 60 had lower functional results. Additional factors did not affect the final results.
CONCLUSION
Staged MIPO may achieve satisfactory results in distal tibial fractures with soft tissue compromise, decreasing deep infections and soft tissue complications.
MeSH Terms
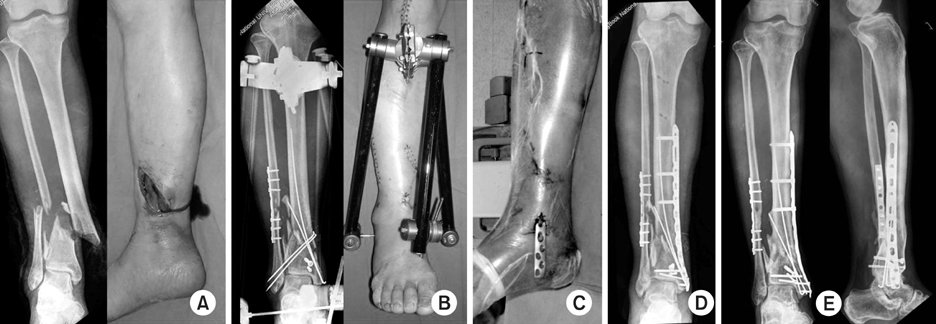
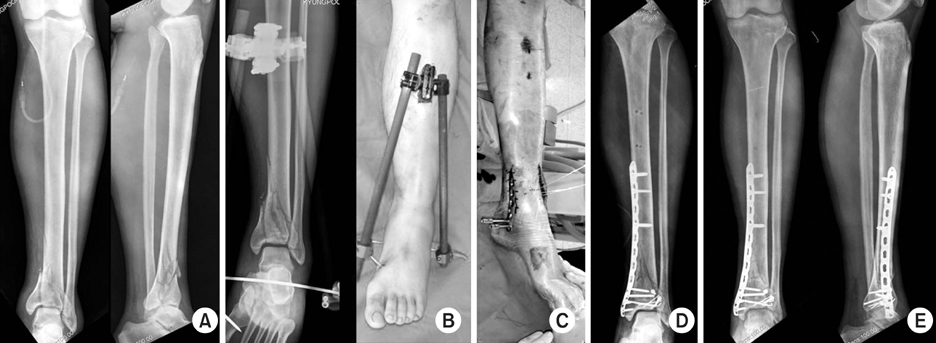
Figure
Cited by 2 articles
-
Minimally Invasive Osteosynthesis with Locking Compression Plate for Distal Tibia Fractures
Sung-Kyu Kim, Keun-Bae Lee, Keun-Young Lim, Eun-Sun Moon
J Korean Fract Soc. 2011;24(1):33-40. doi: 10.12671/jkfs.2011.24.1.33.Anterolateral Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures Using an Anterolateral Locking Plate
Dongwhan Suh, Hwan Hee Lee, Young Hoon Han, Jae Jung Jeong
J Korean Foot Ankle Soc. 2020;24(1):19-24. doi: 10.14193/jkfas.2020.24.1.19.
Reference
-
1. Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001. 15:153–160.
Article2. Chang SA, Ahn HS, Byun YS, Kim JH, Bang HH, Kwon DY. Minimally Invasive plate osteosynthesis in unstable fractures of the distal tibia. J Korean Fract Soc. 2005. 18:155–159.
Article3. Collinge C, Kuper M, Larson K, Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma. 2007. 21:355–361.
Article4. Dillin L, Slabaugh P. Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma. 1986. 26:1116–1119.
Article5. Egol KA, Weisz R, Hiebert R, Tejwani NC, Koval KJ, Sanders RW. Does fibular plating improve alignment after intramedullary nailing of distal metaphyseal tibia fractures? J Orthop Trauma. 2006. 20:94–103.
Article6. Grose A, Gardner MJ, Hettrich C, et al. Open reduction and internal fixation of tibial pilon fractures using a lateral approach. J Orthop Trauma. 2007. 21:530–537.
Article7. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976. 58:453–458.
Article8. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia-results in 20 patients. Injury. 2006. 37:877–887.
Article9. Heim U. Role of the fibula in distal tibial fracture. Z Unfallchir Versicherungsmed. 1990. 83:187–195.10. Helfet DL, Suk M. Minimally invasive percutaneous plate osteosynthesis of fractures of the distal tibia. Instr Course Lect. 2004. 53:471–475.11. Kim JW, Oh CW, Oh JK, et al. Staged minimally invasive plate osteosynthesis of proximal tibial fracture. J Korean Fract Soc. 2009. 22:6–12.
Article12. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994. 15:349–353.
Article13. Kumar A, Charlebois SJ, Cain EL, Smith RA, Daniels AU, Crates JM. Effect of fibular plate fixation on rotational stability of simulated distal tibial fractures treated with intramedullary nailing. J Bone Joint Surg Am. 2003. 85-A:604–608.
Article14. Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibial fractures. Int Orthop. 2008. 32:697–703.
Article15. Marsh JL, Bonar S, Nepola JV, DeCoster TA, Hurtwitz SR. Use of an articulated external fixator for fractures of the tibial plafond. J Bone Joint Surg Am. 1995. 77:1498–1509.
Article16. Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003. 408:286–291.
Article17. Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999. 13:85–91.
Article18. Pugh KJ, Wolinsky PR, McAndrew PM, Johnson KD. Tibial pilon fractures: a comparison of treatment methods. J Trauma. 1999. 47:937–941.
Article19. Ronga M, Longo UG, Maffulli N. Minimally invasive locked plating of distal tibia fractures is safe and effective. Clin Orthop Relat Res. 2010. 468:975–982.
Article20. Ronga M, Shanmugam C, Longo UG, Oliva F, Maffulli N. Minimally invasive osteosynthesis of distal tibial fractures using locking plates. Orthop Clin North Am. 2009. 40:499–504.
Article21. Rüedi TP, Allgöwer M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979. (138):105–110.
Article22. Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 1999. 2:78–84.
Article23. Sohn HM, Lee JY, Ha SH, You JW, Lee SH, Lee KC. Treatment of high-energy distal tibia intraarticular fractures with two-staged delayed minimal invasive plate osteosynthesis. J Korean Fract Soc. 2007. 20:19–25.
Article24. Strauss EJ, Alfonso D, Kummer FJ, Egol KA, Tejwani NC. The effect of concurrent fibular fracture on the fixation of distal tibia fractures: a laboratory comparison of intramedullary nails with locked plates. J Orthop Trauma. 2007. 21:172–177.
Article25. Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res. 1993. 292:108–117.26. Wyrsch B, McFerran MA, McAndrew M, et al. Operative treatment of fractures of the tibial plafond. A randomized, prospective study. J Bone Joint Surg Am. 1996. 78:1646–1657.
Article27. Yang JH, Kweon SH, Kim JW, Park JY, Kim HJ, Lim CM. Two-staged delayed minimally invasive percutaneous plate osteosynthesis for distal tibial open fractures. J Korean Fract Soc. 2008. 21:24–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Minimally Invasive Percutaneous Plate Osteosynthesis Using a Lateral Plate in Distal Tibial Fracture
- Two-staged Delayed Minimally Invasive Percutaneous Plate Osteosynthesis for Distal Tibial Open Fractures
- Minimally Invasive Percutaneous Plate Osteosynthesis Using Periarticular Plate for Distal Tibial Fractures
- Minimally Invasive Plate Osteosynthesis for Periarticular Tibial Fractures