Surgery for Adjacent Segment Changes after Lumbosacral Fusion
- Affiliations
-
- 1Department of Orthopedic Surgery, Kang-Nam St. Mary's Hospital, The Catholic University of Korea, College of Medicine, Seoul, Korea. kyh@catholic.ac.kr
- KMID: 2209715
- DOI: http://doi.org/10.4184/jkss.2002.9.4.332
Abstract
-
PURPOSE: To report upon surgical outcome in terms of adjacent segment changes after lumbosacral fusion and to analyze for
risk factors indicating early surgical intervention for adjacent segment changes.
MATERIAL AND METHODS: This was a retrospective study of twenty patients who underwent revision surgery for adjacent segment changes after lumbosacral fusion. Inclusion criteria were as follows: 1) minimum 24 months follow-up, 2) confirmed adjacent segment changes by CT-myelogram or MRI, 3) conservative treatment for at least 3months, 4) available preoperative X-ray films and 5) posterolateral fusions at a prior fusion. Correlation analysis was performed for age, sex, the number of fused levels, grade of radiographic degeneration and instrumentation using the independent sample t-Test.
RESULTS
Age, sex, the number of fused levels, the use of instrumentation and the preservation of lumbar lordosis were not correlated with the interval to revision (IR). However, the grade of radiographic degeneration (plain film and CT) were highly correlated with IR (R= -0.699, -0.654). Degenerative scoliosis had a shorter IR, with statistical significance (P<0.05), than other disease examined. Excellent and good clinical results were obtained in 14 patients (60%), and solid bony fusion was achieved in 18 patients (90%).
CONCLUSIONS
When deciding upon fusion level, especially in cases of degenerative scoliosis, the need for caution could not be overemphasized. The grade of radiographic degeneration provides a useful indicator for predicting earlier adjacent segment changes.
Keyword
MeSH Terms
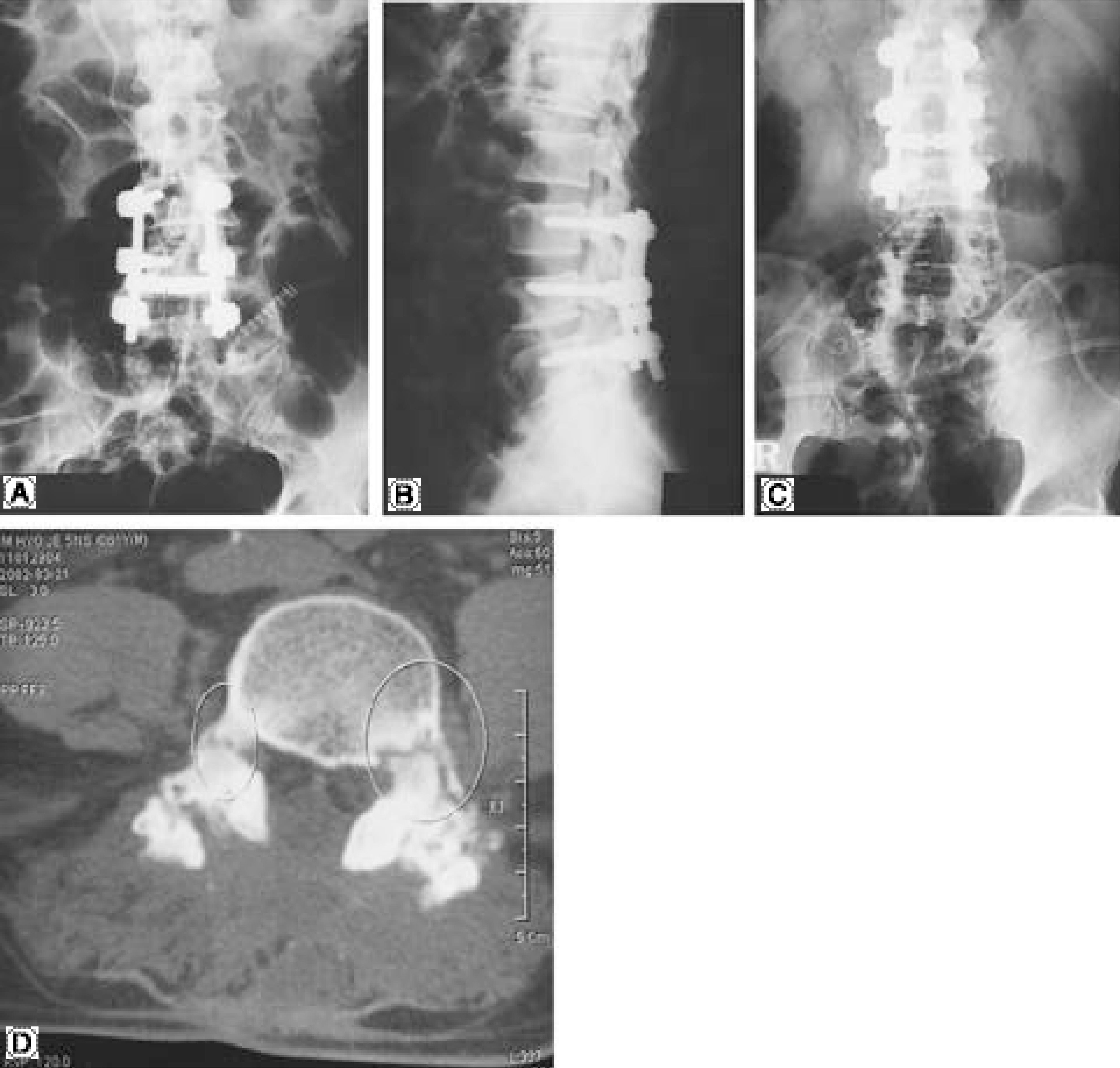
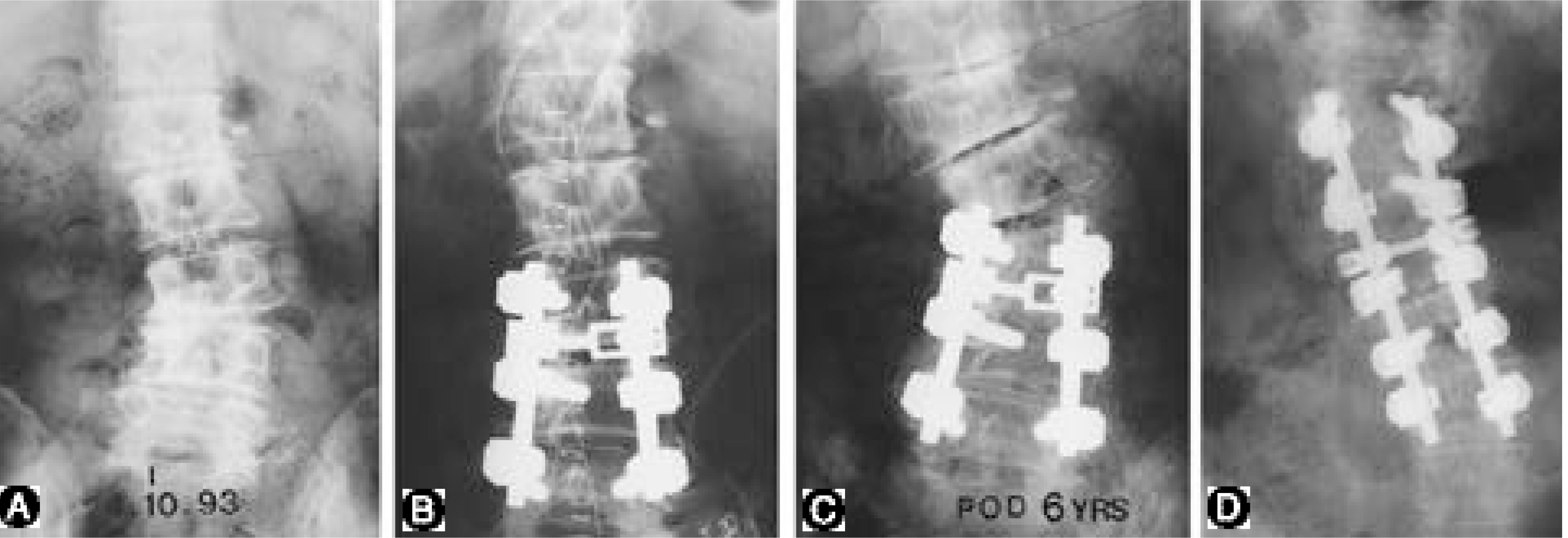
Figure
Cited by 10 articles
-
Progression of Preoperative Degeneration of the Adjacent Segment after Instrumented Lumbar Arthrodesis
Kyu-Jung Cho, Seung-Rim Park, Kyung-Ho Moon, Kang-Yun Lee, Kyung-Hoon Kim, Suk-Bong Kang
J Korean Orthop Assoc. 2007;42(4):453-460. doi: 10.4055/jkoa.2007.42.4.453.The Revision Operation Rate for Adjacent Segmental Degeneration by Survival Analysis in Mono-segment Lumbar Fusion
Tae-Hyung Kim, Jin-Hyok Kim, Sung-Soo Kim, Dong-Ju Lim, Jung-Il Han, Tai-Wan Kim, Se-Il Suk
J Korean Orthop Assoc. 2010;45(4):314-320. doi: 10.4055/jkoa.2010.45.4.314.Comparative Analysis of Revision Surgery Groups between within 5 Years and More than 10 Years after Lumbar Spinal Fusion Due to Adjacent Segment Disease
Jaewan Soh, Junghyeok Kim, Jae Chul Lee, Byung-Joon Shin
J Korean Orthop Assoc. 2016;51(3):214-220. doi: 10.4055/jkoa.2016.51.3.214.Adjacent Segment Degeneration After Spinal Fusion In Lumbar Degenerative Disorders
Chang-Hoon Jeon, Nam-Su Chung, Young-Mo Yang, Nam-Hyun Kim, Yong-Chan Kim, Kyoung-Ho Kim
J Korean Soc Spine Surg. 2004;11(4):238-245. doi: 10.4184/jkss.2004.11.4.238.Risk Factors for Adjacent Segment Disease after Posterolateral Lumbar Fusion
Kyu Yeol Lee, Sung Keun Sohn, Myung Jin Lee, Lih Wang
J Korean Soc Spine Surg. 2008;15(3):174-182. doi: 10.4184/jkss.2008.15.3.174.Risk Factors for Adjacent Segment Disease After Lumbar Fusion
Changju Hwang, Sung-Woo Lee, Young-Joon Ahn, Yung-Tae Kim, Dong-Ho Lee, Choon-Sung Lee
J Korean Soc Spine Surg. 2008;15(1):44-53. doi: 10.4184/jkss.2008.15.1.44.Analysis of Risk Factors and Surgical Results of Lumbar Adjacent Segment Disease
Whoan Jeang Kim, Jong Won Kang, Byoung Sub Kam, Sung Il Kang, Won Cho Kwon, Kun Young Park, Jae Guk Park, Hwan Il Sung, Won Sik Choy
J Korean Soc Spine Surg. 2010;17(2):74-81. doi: 10.4184/JKSS.2010.17.2.74.A Comparison of Adjacent Segment Diseases Above One Versus Above Two Vertebral Segment after Spinal Fusion of the Degenerative Lumbar Disease
Sung-Woo Choi, Joonghyun Ahn, Jae Chul Lee, Hyoung-Mo Koo, Byung-Joon Shin
J Korean Soc Spine Surg. 2013;20(4):135-142. doi: 10.4184/jkss.2013.20.4.135.Motor Weakness of Right Ankle Dorsiflexion Caused by Increasing Size of Sacroiliac Joint Cyst after Posterior Lumbar Interbody Fusion in a Patient with Spinal Stenosis - A Case Report -
Ji-Eun Kwon, Young-Joon Ahn, Bo-Kyu Yang, Seung-Rim Yi, Se-Hyuk Lim, Ye-Hyun Lee, Hae-Min Kim
J Korean Soc Spine Surg. 2015;22(4):178-182. doi: 10.4184/jkss.2015.22.4.178.The Impact of Lumbar Lordosis on the Adjacent Segment Disease after Posterior Lumbar Interbody Fusion
Ki-Tack Kim, Kyung-Soo Suk, Sang-Hun Lee, Jung-Hee Lee, Man-Ho Kim, Dae-Hyun Park, Dae-Seok Huh, Duk-Hyun Kim
J Korean Soc Spine Surg. 2015;22(3):69-74. doi: 10.4184/jkss.2015.22.3.69.
Reference
-
1). Aota Y, Kumano K and Hirabayashi S. Pos tfus ion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 8:464–473. 1995.2). Bastian L, Lange Uta, Knop C, Tusch G and Blauth M. Evaluation of the mobility of adjacent segments after posterior thoracolumbar fixation: A biomechanical study. Eur Spine J. 10:295–300. 2001.
Article3). Brodsky AE, Hendricks RL and Khalil MA, et al. Segmental (floating) lumbar spine fusion. Spine. 14:447–450. 1989.4). Brunet JA and Wiley JJ. Acquired spondylolysis after spinal fusion. J Bone and Joint Surg. 66-B:720–724. 1984.5). Chen WJ, Lai PL, Niu CC, Chen LH, Fu TS and Wong CB. Surgical treatment of adjacent instability after lumbar spine fusion. Spine. 26:E519–524. 2001.
Article6). Etebar S and Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 90:163–169. 1999.7). Fritsch EW, Heisel J and Rupp S. The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine. 21:626–633. 1996.8). Frymoyer JW, Hanley E, Howe J, Kuhlmann D and Matteri R. Disc excision and spine fusion in the management of lumbar disc disease. A minimum 10 year follow-up. Spine. 13:1–6. 1978.9). Frymoyer JW, Hanley E, Howe J, Kuhlmann D and Matteri R. A comparison of radiolographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine. 4:435–440. 1979.10). Guigui P, Lambert P, Lassale B and Deburge A. Long term outcome at adjacent levels of lumbar arthrodesis. Rev Chir Orthop Reparatrice Appar Mot. 83:685–696. 1997.11). Ha KY and Sung TP. Changes of the adjacent mobile segment after cat spine fixation. J of Korean Orthop Surgery. 32:1808–1816. 1997.12). Ha KY, Schendel MJ, Lewis JL and Ogilvie JW. Effect of immobilization and configuration on lumbar adjacent segment biomechanics. J Spinal Disord. 6:99–105. 1993.13). Ha KY, Kim KY, Park SJ and Lee YH. Changes of the adjacent-unfused mobile segment after instrumental lumbar fusion. - More than 5years follow-up-. J Kor Spine Surg. 5:205–214. 1998.14). Ha KY, Moon MS and Paek SY. Effect of Instumental stabilization and fusion of degenerative lumbar scoliosis on unfused adjacent segment. J Kor Spine Surg. 2:270–278. 1995.15). Hambly MF, Wiltse LL, Raghavan N, Schneiderman G and Koenig C. The transition zone above a lumbosacral fusion. Spine. 23:1785–1792. 1998.
Article16). Harris RI and Wiley JJ. Acquired spondylolysis as a sequel to spine fusion. J Bone and Joint Surg. 45-A:1159–1170. 1963.17). Kettler A, Wilke HJ, Haid C and Claes L. Effects of specimen length on the monosegmental motion behaviour of the lumbar spine. Spine. 25:543–550. 2000.18). Kellgren. The epidemiology of chronic rheumatism, Vol 2: Atlas of standard radiographs of arthritis. England: Blackwell Scientific Publications Ltd;1963.19). Kim SS and Michelsen CB. Revision surgery for failed back surgery syndrome. Spine. 17:957–960. 1992.
Article20). Kumar MN, Baklanov A and Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 10:314–319. 2001.
Article21). Kumar MN, Jacquot F and Hall H. Long-term follow- up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 10:309–313. 2001.22). Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 13:375–7. 1988.
Article23). Lee CK and Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine. 9:574–581. 1984.
Article24). Lehmann TR, Spratt KF, Tozzi JE, et al. Long-term follow-up of lower lumbar fusion patients. Spine. 12:97–104. 1987.
Article25). Rahm MD and Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: A retrospective study. J Spinal Disord. 9:392–400. 1996.26). Schlegel JD, Smith JA and Schleusener RL. Lu mbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine. 21:970–981. 1996.27). Whitecloud TS, Davis JM and Olive PM. Operative treatment of the degenerated segment adjacent to a lumbar fusion. Spine. 19:531–536. 1994.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Causes of Revision Arthrodesis for the Degenerative Changes at the Adjacent Segment after Lumbosacral Fusion for Degenerative Lumbar Diseases
- Clinical Results and Changes of Adjacent Segment after Whole Lumbosacral Fusion
- Surgery for Adjacent Segment Changes after Lumbosacral Fusion
- Preliminary Report on Usefulness of Adjacent Interspinous Stabilization using Interspinous Spacer Combined with Posterior Lumbosacral Spinal Fusion in Degenerative Lumbar Disease
- Radiologic Comparison of the Sacroiliac Joint Degeneration Following Lumbar or Lumbosacral Fusion